What it is
Perivascular spaces are located between the walls of blood vessels and the white matter of the brain. These formations are also called criblures or Virchow-Robin spaces. They are filled with cerebrospinal fluid and regulate the outflow of cerebrospinal fluid.
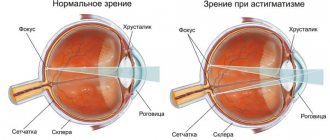
Normally, criblures are so small that they are not visible on an MRI image. However, there are cases when examination reveals expanded perivascular spaces. What does this diagnostic result mean? This suggests that criblures are visualized during an MRI examination. They look like white spots in the photo.
Perivascular spaces of Virchow-Robin
Perivascular canals can only be seen using MRI.
Often Virchow-Robin spaces are not visualized even on MRI images due to their small area. The resolution of the tomograph matters. A size of up to 2 mm is normal and occurs in all people.
- Causes of conditions associated with expansion of the subarachnoid space
- Focal changes in the brain: development, types, symptoms, dangerous or not, how to treat
- Expanded spaces in pathology
- Brain infarction
- Treatment
- Symptoms
- Perivascular spaces are expanded along the penetrating vessels
- Gliosis of the white matter of the brain - what is it?
- Sites of Alzheimer's disease
- Causes of spots on MRI of the brain
- Diagnostics and MRI
Enlarged perivascular spaces are called criblures.
Their increase does not always indicate pathology. The mechanism of their expansion is still being studied. This is possible due to inflammation of the vessel wall, when the latter becomes thinner and becomes more permeable. The released liquid causes the criblure to expand. Another reason is a violation of the flow of cerebrospinal fluid, and another is the lengthening of blood vessels.
Scientists and practicing doctors have not come to a consensus on what is considered pathology and what is not. As a rule, fixation of spaces on MRI images in people of the older age group is a variant of the norm.
They are usually localized in three areas:
- Along the course of the lenticular arteries supplying blood to the basal ganglia - the caudate nucleus, internal capsule, fence.
- Along the course of certain arteries that enter the brain from its outside, and not like most branches of the carotid and vertebral arteries from the inside.
- Along the vessels supplying the midbrain (posterior thalamoperforating and median mesencephalothalamic arteries).
Appear symmetrically. Most often, expansion of the perivascular spaces occurs in the region of the lower basal structures and very rarely in the cerebellum. As a rule, the dimensions do not exceed 5 mm.
CSF flows in the perivascular canals, so on MRI the criblures have the same plane as the latter and appear isodense.
There are 2 projections in which MRI images of the brain are usually taken: frontal and axial. In the first case, the expanded spaces appear in the form of stripes, and in the second they take on a round or oval shape corresponding to the cross-section.
Criblurs on MRI images
The localization and intensity of the MRI signal will help to distinguish pathology or age-related norms.
If criblure is visualized in an atypical place and there is an asymmetrical picture, then most likely we are talking about a disease.
This connection is still being studied
Cryptococcosis
This is a fungal disease that occurs in people with immunodeficiency. Most often occurs in HIV-infected people. In this case, fungal spores can be localized inside the perivascular spaces, causing their expansion. Such accumulations are called gelatinous pseudocysts. Their difference from normal dilated spaces is the preservation of hyperdensity in FLAIR mode.
An MRI picture of concomitant meningitis, hydrocephalus and the presence of foci of cryptococcosis in the brain substance also helps to identify the disease.
Treatment is carried out with antifungal drugs.
Mucopolysaccharidosis
This is an inborn metabolic disease in which the decomposition of glycosaminoglycans is impaired. Excess substances accumulate, forming criblures. In the pictures they look like latticework. Hyperintense white matter is also visualized, which helps distinguish pathology from normality.
Since the disease is based on enzyme deficiency, the goal of therapy is their synthetic replacement: Aldurazyme, Elaprase.
When cerebral circulation is impaired, the criblures expand. Because they are filled with cerebrospinal fluid. They contain a large number of hydrogen atoms. And in this area the response signal will be of high intensity, which can be seen in the photographs as a white spot.
Causes
Enlarged perivascular Robin-Virchow spaces are not always a sign of pathology. This diagnostic result is also observed in completely healthy people. Most often, expansion of criblures is observed in elderly patients and is associated with age-related changes in the brain.
However, in some cases, dilated perivascular spaces may be a sign of the following diseases and conditions:
- brain atrophy;
- leukoaraiosis;
- cerebral ischemia (including cerebral infarction);
- disseminated encephalomyelitis.
In elderly people, expansion of criblures is often observed with hypertension, atherosclerosis, and dementia. These pathologies are usually accompanied by memory impairment and other cognitive impairment.
Epidemiology
The mean age was 58 years (range 24–86 years); the majority (69%) were women [2]. Small VR spaces (<2 mm) are detected in all age groups. With age, VR spaces are found with greater frequency and larger size (> 2 mm) [1]. Some studies have found a correlation between expanded VR spaces and neuropsychiatric disorders [1], multiple sclerosis [1], mild traumatic brain injury [1], and diseases associated with microangiopathy [1].
Additional diagnostic methods
What to do if the MRI results indicate that you have dilated perivascular Virchow-Robin spaces? It is necessary to show the transcript of the study to a neurologist. Only a specialist can determine whether this is a variant of the norm, an age-related feature, or a sign of pathology.
There are cases when MRI does not reveal any changes in the brain, but the image shows dilated perivascular Virchow-Robin spaces. What does this mean? As a rule, such a sign does not indicate pathology. Doctors consider an increase in criblures only in combination with other changes identified during an MRI examination.
If necessary, the doctor may prescribe additional tests:
- multislice computed tomography;
- vascular angiography;
- Dopplerography;
- cerebrospinal fluid examination.
Let's take a closer look at the most common diseases and conditions that can lead to expansion of criblures.
Sources
- "Virchow-Robin Spaces at MR Imaging." Robert M. Kwee, Thomas C. Kwee link
- "Large anterior temporal Virchow-Robin spaces: unique MR imaging features." Lim AT1, Chandra RV, Trost NM, McKelvie PA, Stuckey SL. link
- "Virchow-Robin spaces at MR imaging." Kwee RM1, Kwee TC. link
Author: radiologist, Ph.D. Vlasov Evgeniy Alexandrovich
Full or partial reprint of this article is permitted by installing an active hyperlink to the source
If you still have doubts about the conclusions of your MRI, you can order a review of your study with a detailed transcript here:
Brain atrophy
If the patient’s perivascular spaces are expanded and the volume of the brain is reduced, then doctors talk about organ atrophy. Most often this is a sign of the following diseases:
- senile dementia;
- atherosclerosis;
- Alzheimer's disease.
In these diseases, neurons die. This is accompanied by memory impairment, mental impairment, and mental disorders. Typically, such diseases occur in elderly patients.
In some cases, dilated perivascular Virchow-Robin spaces are detected in newborns. This may be a sign of serious genetic diseases accompanied by the death of neurons.
How to treat such pathologies? After all, it is no longer possible to restore lost neurons. You can only slow down the process of death of nerve cells. Patients are prescribed the following drugs for symptomatic therapy:
- nootropics: Piracetam, Cavinton, Nootropil;
- sedatives: “Phenazepam”, “Phenibut”;
- antidepressants: Valdoxan, Amitriptyline.
The prognosis of such pathologies is usually unfavorable, as brain atrophy and neuronal death progress.
In the last decade, a clinical radiological phenomenon called “small vessel disease” has appeared and is being studied in clinical medicine. Small vessel disease is a systemic disease that affects various organs, but most often the main target of this pathology is the brain, which is why cerebral small vessel disease (CSVD) is identified as a separate concept. This term combines clinical, radiological, biochemical signs of damage to perforating arteries, arterioles, venules and capillaries, which are elements of the blood supply to the deep structures of the brain [1].
BCMS is the cause of 45% of dementia, about 20% of all strokes (of which 25% are lacunar), and 20% of all ischemic strokes are disabling [2]. BCMS currently includes recent small subcortical infarction (NSSI), lacunae, white matter hyperintensity (WMH), lacunae of presumably vascular origin, dilated perivascular spaces (DPVS), cerebral microbleeds (CMB) and atrophy of brain matter [3]. To unify the conclusions of magnetic resonance imaging (MRI), it is recommended to describe changes in BCMS according to the STRIVE standard ( ST
andards for
Report
I
ng
V
ascular changes on n
E
) [3].
Typically, NMSI causes an acute neurological deficit, and the other listed variants of BCMS are clinically unnoticeable and are therefore called “silent” (asymptomatic) lesions. All subtypes of BCMS are characterized by diffuse pathology of small vessels and are more dynamic than previously thought (Fig. 1).
Rice. 1. NMSI.
Clinically diagnosed lacunar syndrome can be a consequence of both ischemia and minor hemorrhage. Often the cause of hemorrhagic strokes in adults is BCMS [2]. Lacunar syndrome may be caused by a recent small infarction of the white matter, basal ganglia, pons, or brainstem less than 1.5–2 cm in diameter [3], which is usually explained by changes in a single thin deep artery. About 20% of NMSIs can cause cortical symptoms, and conversely, cortical infarcts can manifest as lacunar syndromes, which probably occurs when lacunar infarcts are close to the cortex [4]. It should be noted that even with sensitive MRI imaging such as DWI, about 30% of patients with clinical symptoms of stroke do not have any recent ischemic lesions [5], however, at 1-year follow-up, patients with DWI-negative results develop recurrent stroke. stroke and, as a consequence, disability and cognitive impairment, as in patients with NMSI on primary DWI. Thus, a negative DWI MRI result cannot exclude the diagnosis of stroke [6]. It should be noted that DWI-positive lesions may be clinically asymptomatic (“silent”), for example as a second asymptomatic acute infarction in patients with another acute symptomatic infarction or in patients with acute hemorrhagic stroke, as well as in patients with significant WMH who have no obvious stroke symptoms.
No association has been found between lacunar stroke and middle cerebral artery stenosis [7, 8]. Larger and tubular lacunar infarcts may be caused by proximal artery disease. The results of the studies indicate that it is impossible to determine the etiology of a specific recent lacunar ischemic stroke based on its size, shape or location [9, 10]. The evidence for embolism as a cause of lacunar ischemic stroke is inconclusive [11]. Intrinsic small vessel pathology remains the most likely cause of NMSI, although the underlying mechanism is unclear. Current epidemiological data show that hypertension is equally common in both non-lacunar and lacunar ischemic stroke, and many patients with lacunar stroke are normotensive [11]. Similarly, other traditional identified risk factors (diabetes mellitus, hypercholesterolemia and smoking) occur with equal frequency in both lacunar and other ischemic strokes [12].
The American Heart Association and the American Stroke Association (AHA/ASA) distinguish a group of so-called asymptomatic cerebrovascular diseases - Silent Cerebrovascular Diseases, which include asymptomatic cerebral infarction (BCI), WMH of presumably vascular etiology, CMB. BCI, also called silent stroke, presents as subcortical cavities or cortical areas of atrophy and gliosis that are thought to be due to a previous infarction. Approximately 25% of people over 80 years of age have one BCI. There are approximately ten BCIs per symptomatic stroke. Thus, we see differences in the definitions of NMSI and BCI [13].
WMH of vascular origin is common in older adults and is considered a typical feature of BCMS with clinical correlates of cognitive impairment and depression. WMH develops subclinically, but almost triples the risk of stroke, doubles the risk of dementia and increases the risk of death [2, 14]. The AHA/ASA defines WMH as areas of demyelination, gliosis, arteriosclerosis, and microinfarcts presumably caused by ischemia [13] (Fig. 2).
Rice. 2. WMH of presumably vascular etiology.
WMH is usually symmetrically distributed in the white matter, including the pons, brainstem, and deep gray matter. WMH is hyperintense on T2 or FLAIR scans and may be heterogeneous depending on stage of development and severity. WMH is a rather heterogeneous phenomenon, possibly reflecting different stages of the disease [15].
MRI studies and autopsies revealed swelling of the brain substance in the area of the WMH, which probably develops due to leakage of plasma proteins through the damaged blood-brain barrier (BBB) [16, 17]. Although these "white" areas have so far been considered uniform, different degrees of "whiteness" may indicate different stages of the disease: some very white areas of WMH are likely to be end-stage and irreversible, other less white lesions may be reversible if are the result of an imbalance of interstitial fluid that occurred before permanent tissue damage developed. The described microstructural changes occur not only in hyperintense white matter, but also in apparently normal white matter [18], the intactness of which decreases as it approaches the area of the WMH [19].
It is assumed that the cause of WMH may be incomplete infarction and chronic hypoperfusion, but there is little evidence for this. Disruption of the BBB was found in areas of the WMH at autopsy [15, 16], which is confirmed by MRI studies with the determination of albumin in the cerebrospinal fluid and blood plasma [20]. It is assumed that disruption of the BBB leads to the penetration of plasma and blood cells into the perivascular spaces, activation of autoimmune perivascular inflammation, demyelination and gliosis. Thus, the formation of WMH is a multifactorial process. Hypoperfusion, venous compromise, and BBB disruption with subsequent autoimmune inflammation may play a critical role in the initiation or progression of WMH.
Another variant of BCMS are lacunae of presumably vascular origin, which on MRI appear as round or ovoid subcortical cavities with a diameter of 3-15 mm, filled with fluid. They can either occur without any preliminary symptoms or be a consequence of a previous acute NMSI or hemorrhage [3]. RPVP, if their diameter exceeds 3 mm, can imitate lacunae. Lacunae are usually surrounded by a hyperintense rim that helps differentiate them from RPVP, but in some cases the rim may be absent. It is important to differentiate between lacunae and RPVP, as they reflect different pathological conditions and differ in clinical associations and consequences. Lacunae do not usually cause acute symptoms, but an increasing number of lacunae is associated with dementia, cognitive impairment, gait disturbances, and an increased risk of stroke. Among the elderly population (average age 50–75 years), the prevalence of lacunae ranges from 8 to 28% [21] (Fig. 3).
Rice. 3. Lacunae of presumably vascular etiology.
The dilated perivascular spaces surrounding the cerebral vessels are fluid-filled spaces that follow the course of the vessel through the brain parenchyma [22]. Perivascular spaces are usually microscopic and undetectable on routine neuroimaging. When dilated, they are most often hyperintense on T2 scans and appear either as a point signal with a diameter of less than 3 mm, if the scanning plane is perpendicular to the course of the vessel, or as linear, if the scanning plane is parallel to the course of the vessel [23]. RPVPs are most common in the lower basal ganglia and centrum semiovale but can also be found in the brainstem. Although a diameter of 3 mm has generally been considered as distinguishing RVP from lacunae, sometimes perivascular spaces can be larger and even cause mass effect [3, 24]. RPVPs usually do not have a hyperintense rim on T2 or FLAIR scans (Figure 4).
Rice. 4. RPVP.
The clinical significance of RPVP remains unclear. In some studies, RPVP was correlated with an increased risk of cognitive decline or hypertension [24]. The mechanisms underlying enlarged perivascular spaces are not fully understood. In normal aging and other neurological diseases (for example, multiple sclerosis), RVP correlates with markers of inflammation [25], and in BCMS this may be a sign of BBB disruption [20].
Another variant of BCMS are CMBs, which appear as small round and homogeneous foci of hypointensity in T2* or SWI MRI modes. It was found that CMBs are mainly macrophages located in perivascular spaces containing hemosiderin. Other possibilities include old hematomas, intact red blood cells, and (very rarely) vascular pseudocalcification, microaneurysms, and vessel dissection [26]. The AHA/ASA defines CMBs as small areas of hemosiderin deposition after a previous asymptomatic hemorrhage, which are detected in special MRI modes that are optimal for their detection [13] (Fig. 5).
Rice. 5. CMC.
Lipofibrohyalinosis and amyloid angiopathy are the most common vascular factors associated with CMB. The two vasculopathies are thought to have different distribution patterns: CMBs in the basal ganglia, thalamus, brainstem, and cerebellum are usually attributed to lipofibrohyalinosis, while amyloid angiopathy is more characterized by lobar CMBs [27]. Most CMBs are asymptomatic and can be found in healthy adults, but are more often a marker of vascular risk or amyloid accumulation. CMBs are also correlated with cognitive impairment, dementia, and transient neurological deficits [28]. In patients with ischemic stroke and non-traumatic intracerebral hemorrhage, the incidence of CMB can reach 33.5–67.5% [29].
Among the markers of BCMS, cerebral atrophy is distinguished, which is characterized by a decrease in the volume of brain matter that is not associated with such focal lesions as trauma and heart attack. The atrophied tissue is replaced by cerebrospinal fluid, resulting in replacement hydrocephalus [3].
To prevent BCMS, vascular risk factors should be taken into account and controlled. Modifiable risk factors include hypertension, hypercholesterolemia, smoking and diabetes mellitus. Lipohyalinosis, typical vascular changes in BCMS, has long been considered a result of hypertension. The theory is supported by clinical evidence that hypertension is more common in patients with WMH and higher blood pressure is associated with more severe BCMS [30]. High salt intake is associated with more severe disease, causing increased blood pressure and directly affecting the endothelium [31]. Smoking is an independent predictor of progression of WMH and is associated with a high burden of association of different types of BCMS [32, 33]. Physical inactivity is a risk factor for a greater number of WMH lesions in old age [34].
When diagnosing BCMS, the following recommendations must be taken into account: 1) MRI is more sensitive than computed tomography (CT) in the diagnosis of asymptomatic cerebrovascular diseases; 2) the description of MRI should be carried out in accordance with the STRIVE standard; 3) WMH should be described using validated jackal rating scales, such as the Fazekas MRI scale [13].
When examining patients with BCMS, the following recommendations should be taken into account: 1) assess vascular risk factors and pulse rate for atrial fibrillation; 2) consider visualization of the carotid arteries during BCI in the carotid region; 3) consider echocardiography if cardioembolic origin of BCI is suspected; 4) consider non-invasive CT or MRI angiography in the presence of large (more than 1 cm) asymptomatic cerebral hemorrhage [13].
Prevention of stroke in BCI: 1) history should be assessed to ensure that the infarction was asymptomatic; 2) it is recommended to carry out preventive measures according to the guidelines for the primary prevention of ischemic stroke; 3) it must be borne in mind that the effectiveness of aspirin has not been studied for these situations; 4) Clinicians should understand that there is an increased risk of further stroke and keep this in mind when deciding on anticoagulation for atrial fibrillation, revascularization for carotid stenosis, treatment of hypertension, or initiation of statins. However, clinicians should also understand that BCIs have not been studied in randomized clinical trials [13].
Prevention of stroke in case of WMH: 1) carry out preventive measures according to the guidelines for the primary prevention of ischemic stroke; 2) it is unclear whether WMH without other risk factors warrants prescribing aspirin; 3) clinicians should understand that there is an increased risk of another stroke in the future and remember this when deciding on anticoagulants for atrial fibrillation, revascularization for carotid stenosis, treatment of hypertension, and initiation of statins. However, clinicians should also be aware that the role of WMH burden has not been studied in randomized clinical trials [13].
Anticoagulants and other treatment for asymptomatic CMB: 1) it is advisable to provide anticoagulant therapy to patients with CMB, if indicated (for example, for atrial fibrillation); 2) new oral anticoagulants are preferable to warfarin; 3) percutaneous closure of the left atrial appendage can be considered as an alternative to anticoagulants; 4) antiplatelet therapy is appropriate for patients with CMB, if indicated; 5) MRI screening for CMB is not advisable before starting antithrombotic therapy; 6) persons with asymptomatic CMB have an increased risk of ischemic and hemorrhagic stroke [13].
Safety of treatment of acute ischemic stroke in patients with asymptomatic CMB: 1) intravenous administration of alteplase to patients with acute ischemic stroke and proven CMB is advisable if indicated; 2) it is advisable to perform endovascular thrombectomy in patients with acute ischemic stroke and proven CMB; 3) for patients with acute ischemic stroke and CMB, intravenous administration of alteplase followed by endovascular thrombectomy is not an approved strategy [13].
Taking into account the heterogeneity, complexity and little knowledge of the pathogenesis of BCMS, questions about the treatment of these conditions have a meager number of answers. It is likely that prophylactic measures designed to prevent large artery disease and cardioembolism (including antiplatelet, antihypertensive drugs and statins) may be ineffective in BCMS, and intensive antiplatelet therapy may be dangerous in CMMC due to the risk of major hemorrhage [35]. ].
Pathogenetic mechanisms of BCMS include damage to arteries, arterioles (fibrinoid necrosis and lipohyalinosis), capillaries and small veins (collagenosis) of the brain, which, in addition to impaired cerebral perfusion, causes disruption of the BBB with the migration of blood plasma proteins, disruption of the circulation of intercellular fluid in the perivascular spaces ( waterlogging) and activation of macrophages with the development of local inflammation [36]. In light of these data, the use of neuroprotectors of a peptide nature may be unsafe due to the possible potentiation of tissue immune-mediated inflammation.
One of the promising groups of drugs for BCMS may be drugs that activate the endogenous system of the atypical messenger nitric oxide (NO) through inhibition of phosphodiesterase. Eleven types of phosphodiesterase have been found in the human body [37]. Phosphodiesterase type 1 is expressed in the myocardium, arterial smooth muscle, and neurons. The most famous and studied representative of phosphodiesterase type 1 inhibitors is vinpocetine (Cavinton) [38]. In addition to the vasoactive effect mediated through the NO system, vinpocetine has a vasodilating effect, suppressing the calcium-dependent angiospastic reaction. In addition to the cerebral vasodilating effect, vinpocetine has been found to restore the structure of the altered vascular wall (anti-remodeling effect) [39], which is a pathogenetically substantiated indication for BCMS.
Currently, various medical schools support the opinion of other mechanisms of action of vinpocetine. Vinpocetine inhibits the kinase pathway of the cellular inflammatory response, which allows it to be positioned as a new anti-inflammatory agent, which is undoubtedly important given the role of neuroinflammation in BCMS and other acute and chronic encephalopathies (for example, in traumatic brain disease). In an experiment, vinopcetin demonstrated an anti-inflammatory effect on cultures of endothelial cells and vascular smooth muscle cells, monocytes/macrophages, neutrophils, microglia and dendritic cells [40]. In a clinical multicenter study of patients with carotid stroke, vinpocetine (30 mg per day intravenously for 14 days) showed the ability to suppress neuroinflammation with improved clinical parameters compared with the control group 3 months after stroke [41]. The authors note that the study was conducted with the original Gedeon Richter drug.
An important property of vinpocetine is the ability to block presynaptic Na channels, which suppresses glutamate secretion and reduces glutamate excitotoxicity. This effect of vinpocetine exceeds the similar activity of some anticonvulsants [42] and determines the high clinical effectiveness of the drug not only in vascular pathology, but also in neurodegenerative diseases such as Alzheimer's disease, as well as in traumatic brain injury (post-traumatic encephalopathy, or traumatic brain disease ). The effectiveness of vinpocetine as an anticonvulsant in these clinical situations is explained by the fact that disinhibition in the central nervous system with the formation of a community of epileptic neurons (a generator of pathologically enhanced excitation) is a typical pathological process in acute and chronic diseases of the central nervous system of various etiological factors [43].
Russian researchers have shown an improvement in cognitive function after 3 months of treatment with Cavinton Comfort in patients with chronic cerebral ischemia of the 1st-2nd degree [44] and dyscirculatory encephalopathy [45].
In conclusion, it should be noted that there is currently convincing evidence of the multimodal action of vinpocetine, including vasodilation, antioxidant, anti-inflammatory, antiplatelet, and anti-remodeling effects. These synergistically working mechanisms explain the effectiveness of vinpocetine in many vascular diseases of the brain (including BCMS). Vinpocetine can also be considered as a potentially effective agent in other pathological conditions due to its anti-inflammatory effect, the ability to provide a cytoprotective effect in ischemic damage and activate vasodilation with an increase in blood flow not only in nervous tissue [40]. Considering the fact that BCMS is a chronic multifactorial process, its treatment should comply with the principles of treatment of chronic diseases - targeted long-term (lifelong) pharmacotherapy. The presence of signs of BCMS indicates a long-standing brain disorder, which is potentially reversible in some regions; therefore, vinpocetine (Cavinton Comfort as an innovative form) in such a situation should be recommended for continuous use of 30 mg per day for several years or for life. The lack of drug interactions between vinpocetine and cardiac medications makes it especially attractive for patients receiving cardiac medications.
Thus, BCMS is a dynamic disease of the entire brain. All subtypes of the disease may have common signs characteristic of BCMS. Some pathological changes in the early stage of the disease are reversible, but they can gradually progress and become irreversible. Modification of traditional risk factors and maintaining a healthy lifestyle are currently the most important preventive and therapeutic approaches for BCMS. Future studies of BCMS should stratify by stroke subtype and carefully examine risk factors. Clinical trials and experimental studies targeting endothelial and BBB integrity should be conducted.
The work was carried out using subsidies allocated to the Kazan Federal University to fulfill the state assignment in the field of scientific activity. Task No. 17.9783.2017/8.9.
The authors declare no conflict of interest.
Information about authors
Esin Radiy Germanovich
- Doctor of Medical Sciences, Prof. Department of Neurology of the Kazan Medical Academy - a branch of the Russian Medical Academy of Continuing Professional Education, prof. Department of Russian Language and Applied Linguistics, Department of Fundamentals of Clinical Medicine, Kazan Federal University; https://orcid.org/0000-0001-6762-8845
Khairullin Ilshat Khamzovich
— Candidate of Medical Sciences, senior researcher at the Research Laboratory of Clinical Linguistics, Kazan Federal University; https://orcid.org/0000-0003-0919-035x
Abrarova Gulshat Fagimovna
— student of Kazan Federal University; https://orcid.org/0000-0001-5971-2211
Esin Oleg Radievich
— Candidate of Medical Sciences, Associate Professor of the Department of Russian Language and Applied Linguistics, Senior Researcher at the Clinical Linguistics Research Laboratory of Kazan Federal University, Neurologist at the Kazan University Clinic; https://orcid.org/0000-0003-4244-4446
Leukoaraiosis
Doctors call leukoaraiosis a thinning of the white matter of the brain. Due to structural changes in the nervous tissue, patients have enlarged perivascular spaces. This is also a sign of diseases characteristic of older people:
- hypertension;
- atherosclerosis;
- senile dementia.
Changes in the white matter of the brain cause cognitive impairment. Patients are treated symptomatically with nootropic drugs. These drugs improve the nutrition of neurons and stop their death. For atherosclerosis, statins are indicated. For high blood pressure, antihypertensive drugs are prescribed.
Kidneys as a factor of pathology
Kidney pathology can cause a moderate edematous syndrome, in which there will be a situation associated with the expansion of the spaces under the meninges. Sometimes this may be due to poisoning with heavy metal salts. Chronic alcohol intoxication may also be a cause.
Of course, all these conditions are more typical for adults. In children, the predominant causes are congenital anomalies. The cause may also be birth trauma, which disrupts the circulation of fluid in the cranial cavity.
Ischemic conditions
With ischemia, the blood supply to the brain deteriorates. This is usually a consequence of atherosclerotic changes in the vessels. The patient periodically experiences dizziness, double vision, motor coordination disorders, speech and memory disorders. Due to changes in the vessels, the spaces around their walls also expand.
Patients are prescribed nootropic drugs (Piracetam, Cerebrolysin, Actovegin), as well as drugs that normalize metabolism in brain cells (Cortexin, Ceraxon). In this case, it is very important to carry out etiotropic treatment of atherosclerosis with statins. The drugs Lovastatin, Atorvastatin, and Simvastatin are prescribed. This therapy eliminates the cause of ischemia.
function
One of the most basic roles of the perivascular space is to regulate the movement of fluid in the central nervous system and its drainage. The gaps eventually drain fluid from the neuronal cell bodies into the cervical lymph nodes. Specifically, the "Tide Hypothesis" proposes that cardiac contraction creates and maintains pressure waves to modulate flow to and from the subarachnoid space and perivascular spaces. Acting as a sort of sponge, they are essential for signal transmission and extracellular fluid maintenance.
Another function is as an integral part of the blood-brain barrier (B). While Bs are often described as tight junctions between endothelial cells, this is a simplification that neglects the complex role that perivascular spaces take in separating venous blood from the brain parenchyma.
Often, cell debris and foreign particles that are impermeable to B will get through the endothelial cells, only to be phagocytized into the perivascular spaces. This is true for many T and B cells as well as monocytes, giving this small fluid-filled space an important immunological role.
Perivascular spaces also play an important role in immunoregulation; They contain not only interstitial and cerebrospinal fluid, but they also have a constant flow of macrophages, which is regulated by mononuclear cells through the blood, but do not pass through the basement membrane of the glial membrane limiting.
Likewise, as part of its role in signal transduction, the perivascular spaces contain vasoactive neuropeptides (VNS), which, in addition to regulating blood pressure and heart rate, have an important role in the control of microglia. ANS serves to prevent inflammation by activating the enzyme adenylate cyclase, which then produces cAMP.
The production of cAMP mediates the modulation of autoreactive T cells by regulatory T cells. The perivascular space is a susceptible space for VN compromise and, when their function is reduced to a space, the immune response is negatively affected and the potential for increased degradation. When T cell inflammation begins, astrocytes begin to undergo apoptosis, due to their CD95 receptor to open the glial limiting membrane and let T cells into the brain parenchyma.
Brain infarction
Often the perivascular spaces are dilated in patients who have suffered a cerebral infarction. This disease is a consequence of prolonged ischemia. In some cases, cerebral infarction is asymptomatic and goes unnoticed by the patient. Its consequences can only be seen in an MRI scan.
It is important to remember that if the patient has risk factors (high blood pressure, atherosclerosis, diabetes), then the heart attack may recur in severe form. To prevent a recurrent attack of acute ischemia, patients are prescribed antihypertensive medications, hypoglycemic agents, and blood thinners.
Disseminated encephalomyelitis
Disseminated encephalomyelitis (DEM) is an acute pathology of the central nervous system. In this disease, the myelin sheath of nerve fibers is destroyed. The perivascular Virchow-Robin spaces are dilated due to damage to the white and gray matter. The MRI image shows foci of demyelination.
This pathology is of autoimmune origin. The clinical picture of the disease resembles signs of multiple sclerosis. Patients experience gait and movement disturbances, speech disorders, dizziness, and inflammation of the optic nerve.
Unlike many other demyelinating diseases, REM is treatable. Patients are prescribed corticosteroids to suppress the autoimmune reaction:
- "Prednisolone";
- "Dexamethasone";
- "Metypred."
After a course of therapy, 70% of patients experience complete recovery. In advanced cases, patients may still experience the consequences of the disease: impaired sensitivity of the limbs, gait disturbances, and visual disturbances.
Compound
Perivascular spaces are gaps containing interstitial fluid that span between blood vessels and their host organ, such as the brain, that they penetrate and serve as extravascular channels through which solutes can pass. Like the blood vessels around which they form, perivascular spaces occur in both the brain's subarachnoid space and subpial space.
The perivascular spaces surrounding arteries in the cerebral cortex and basal ganglia are separated from the subpial space by one or two layers of the leptomeninges, respectively, as well as the pia mater. By virtue of the leptomeningeal cell layer, the perivascular spaces belonging to the subarachnoid space are continuous with those of the subpial space.
The direct connection between the perivascular spaces of the subarachnoid space and subpial space is unique to the cerebral arteries, since no leptomeningeal layers surround the cerebral veins. Using a scanning electron microscope, it was determined that the spaces surrounding the blood vessels in the subarachnoid space are not continuous with the subarachnoid space due to the presence of mater PIA cells connected by desmosomes.
Perivascular spaces, especially around fenestrated capillaries, are found in many organs, such as the thymus, liver, kidney, spleen, bone, and pineal gland. Particularly within the brain circumventricular organs—subfornical organs, area postrema, and median eminence—large perivascular spaces are present around fenestrated capillaries, indicating that the spaces serve a dispersive role as brain- or blood-transmitting messengers.
Perivascular spaces can be enlarged to a diameter of five millimeters in healthy individuals and do not imply disease. When increased, they can impair the function of the areas of the brain to which they project. The stretch may occur on one or both sides of the brain.
Perivascular spaces differ on MRI in several key features. The spaces appear in contrast to round or oval objects with a signal intensity visually equivalent to that of the cerebrospinal fluid in the subarachnoid space. Additionally, the perivascular space has no mass effect and is located along the blood vessel around which it forms.
Prevention
How to prevent the above pathologies? It can be concluded that older patients are more susceptible to such diseases. Therefore, all people over 60 years of age need to regularly visit a neurologist and undergo an MRI examination of the brain.
It is also important to constantly monitor blood cholesterol levels and blood pressure. After all, diseases accompanied by pathological changes in the white matter most often develop against the background of atherosclerosis and hypertension.