The expansion of the external cerebrospinal fluid spaces of the brain in adults can develop in the same way as in small children. In childhood, it is provoked by a violation of the formation of central nervous system structures during the prenatal period of fetal development, trauma during childbirth, and intrauterine infection. In adults, hydrocephalus is usually a consequence of head injury or infectious diseases of the central nervous system.
What it is
Externally, the brain is reliably protected from external influences by the bones of the skull. Cerebrospinal fluid is responsible for its internal protection: it prevents injury to the organ on the inner surface of the skull, ensures the maintenance of optimal intracranial pressure and regulates the internal state of the water-electrolyte environment.
In addition, cerebrospinal fluid is responsible for metabolic processes between blood and brain matter and removes the products of its metabolism.
Thus, cerebrospinal fluid plays a secondary, but no less significant role in the functioning of all brain structures. Therefore, any disturbances in its composition or deviations in concentration inside the skull immediately affect a person’s well-being.
The production of cerebrospinal fluid occurs in the ventricles of the brain through the epithelium lining them inside. From there, the fluid is delivered through the cerebrospinal fluid pathways to the outer surface of the organ, where it is collected in tanks, washes it and is absorbed through the venous sinuses and granulations of the arachnoid membrane.
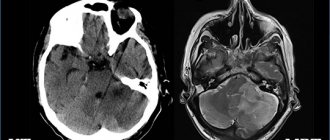
The expansion of the external cerebrospinal fluid spaces of the brain in adults is characterized by the accumulation of cerebrospinal fluid on the surface of the organ. This disease is called external hydrocephalus. It manifests itself in the expansion of the external brain cavities and deformation of brain tissue due to their compression.
The following external liquor spaces of the brain are prone to such changes:
- Tanks (located in the subarachnoid space in the areas of divergence of the arachnoid and pia mater);
- Subarachnoid fissures (located under the arachnoid membrane).
The accumulation of cerebrospinal fluid in them leads to an increase in intracranial pressure and the appearance of signs of hypertensive-hydrocephalic syndrome. It manifests itself in neurological abnormalities: convulsions, cephalgia, deterioration of hearing and vision, and in especially severe cases – paresis, paralysis, and decreased mental abilities. These manifestations are caused by increased pressure on neurons and their dysfunction.
Stages of expansion of subarachnoid spaces
The location of the liquor-containing spaces determines the possibility of free flow from one tank to another. An increase in intracranial pressure is promoted by compression of blood vessels and ventricles of the brain by external formations, accumulation of blood (hematoma), edema, and inflammatory foci.
The main stages of expansion of the subarachnoid spaces:
- Moderate – exceeding the size by up to two millimeters;
- Average - up to four millimeters;
- Heavy – over 4 mm.
In an adult, the expansion of liquor-containing spaces is proportional to the growth of the head and swelling of the fontanelles. Detection of external changes requires timely treatment to prevent irreversible complications. Correct therapy allows you to restore dilated ventricles and liquor spaces to normal.
Causes and symptoms
The expansion of the cerebrospinal fluid spaces of the brain is caused by impaired circulation of cerebrospinal fluid along the cerebrospinal fluid pathways.
This may happen for the following reasons:
- Increased cerebrospinal fluid production;
- Delays its absorption into the circulatory system;
- Due to the blocking of the main pathways for fluid removal by various formations: tumor, blood clots, cyst.
In young children, expansion of the functional cavities of the liquor system can be provoked by:
- Intrauterine infection;
- Head injuries;
- Inflammation of the meninges;
- Exposure to toxic chemicals;
- Congenital anomalies of the structure of the central nervous system structures;
- Presence of intracerebral tumors, cysts;
- Ischemic damage to brain structures due to prolonged hypoxia.
With the expansion of the subarachnoid convexital spaces (in the area of the central sulcus), children experience more serious neurological disorders, including heart rhythm disturbances. In adults, expansion of external liquor spaces most often becomes a consequence of head injury, infectious diseases of the central nervous system, and tumors of the brain.
Pathology can be suspected by the following manifestations:
- Morning headache;
- Nausea and vomiting that does not depend on food intake;
- Dizziness;
- Drowsiness, apathy;
- Hearing and vision impairment;
- Decreased mental abilities;
- Memory problems;
- Movement disorders: apraxia, limb tremor;
- Convulsions, paresis, paralysis.
In especially severe cases, increased pressure on brain structures leads to a displacement of important functional centers of the nervous system. This condition is life-threatening for the patient: for example, when the trunk is displaced, serious problems with breathing and cardiac activity are observed.
Reasons for the expansion of convexital liquor spaces in children
Etiology of congenital forms:
- Benign and malignant neoplasms;
- Inflammatory processes (meningitis, meningoencephalitis);
- Traumatic brain injuries;
- Cerebral origin when passing through the birth canal;
- Hydrocephalus (dropsy);
- Increased intracranial pressure.
The first signs of pathology can be detected by parents by the protrusion of the skull in the area of the sutures. The second specific manifestation is the divergence of the gap between the hemispheres. The changes lead to limited head elevation. Initially, neuropathologists make a diagnosis of perinatal encephalopathy. Diagnostic methods allow you to more accurately identify cerebral changes.
Secondary symptoms:
- Decrease in reflex activity of the limbs;
- Loss of appetite, weight loss;
- “Moonlight gaze” - lower drooping of the eyelids, visualization of the iris and pupil.
The expansion of the convexital grooves of the brain in the subarachnoid spaces can result in atrophy of the parietal, frontal, temporal, and occipital regions. Against the background of pathology, deformation of the ventricular system occurs.
Atrophic cerebral changes provoke post-ischemic conditions, meningococcal, tuberculous encephalitis, and cancer processes. Expansion of the subarachnoid space is a consequence of the destruction of certain areas of the cerebral parenchyma. A decrease in the amount of white and gray matter leads to the filling of free spaces with cerebrospinal fluid and blood.
Treatment
Treatment tactics for neurological disorders caused by expansion of external liquor spaces depend on the form and stage of the disease:
- Acute hydrocephalus of the brain threatens the patient’s life and therefore requires radical measures: neurosurgical surgery. During this procedure, craniotomy is performed, followed by the installation of an external drainage system, which will ensure continuous outflow of excess cerebrospinal fluid. One of the advantages of this method of treatment is the possibility of administering drugs directly to the brain structures, for example, blood thinners and anti-inflammatory drugs. At the moment, this treatment option is considered outdated and is rarely used in practice due to the inconvenience of the drainage system design and the high risk of patient infection.
- Treatment of chronic expansion of external liquor spaces involves performing liquor shunt operations. This type of surgery involves the installation of a complex system of valves and catheters through which excess cerebrospinal fluid is discharged into the natural cavities of the body - the abdominal, pelvic or atrium.
If the patient has been diagnosed with the initial stage of expansion of the external liquor spaces, then conservative treatment is used.
It consists of taking the following medications:
- To reduce intracranial pressure, diuretics (Diacarb, Mannitol) are prescribed - drugs that can remove excess fluid from the cerebrospinal fluid spaces through urine. They are used only when the natural outflow of cerebrospinal fluid is preserved.
- Maintaining the required potassium concentration in the body (Panangin).
- To restore brain activity and improve metabolic processes in brain tissue, nootropic drugs (Cebrolysin, Cavinton, Actovegin) are prescribed.
These measures are aimed at reducing intracranial pressure, normalizing the main functions of the central nervous system, as well as providing brain tissue with the necessary nutrients. If conservative therapy is ineffective and the patient’s condition continues to deteriorate, then surgical treatment is indicated.
Alarming symptoms
When the convexital spaces expand, the following symptoms are observed:
- constant headache (it appears immediately after waking up);
- nausea;
- vomit;
- dizziness;
- memory impairment (in adults);
- irritability;
- drowsiness;
- fatigue;
- in children, the size of the skull increases;
- high sensitivity to light and sound.
At first, the disease occurs without visible symptoms. Then they make themselves felt, but the intensity may vary. It depends on the degree of brain damage and the amount of cerebrospinal fluid released. If the lesion is local and minor, symptoms may be minimal. This condition responds well to treatment, but it is important to start it at the first sign of pathology, before irreversible structural changes occur.
The causes of pathology at different ages differ. In infants, this is most often birth trauma, meningitis, arachnoiditis, or developmental pathologies (genetic code is disrupted). In adults – mechanical trauma, pseudocyst or tumor.
There are different degrees of uniform expansion of the subarachnoid space:
- light (1-2 mm);
- average (3-4 mm);
- severe (4 mm or more).
Localization also varies (interhemispheric, posterior, anterior, etc.). Different amounts of fluid may accumulate, and the external manifestations will also be different. Sometimes the skull becomes enlarged and there is pronounced asymmetry.
Leukoaraiosis
Doctors call leukoaraiosis a thinning of the white matter of the brain. Due to structural changes in the nervous tissue, patients have enlarged perivascular spaces. This is also a sign of diseases characteristic of older people:
- hypertension;
- atherosclerosis;
- senile dementia.
Changes in the white matter of the brain cause cognitive impairment. Patients are treated symptomatically with nootropic drugs. These drugs improve the nutrition of neurons and stop their death. For atherosclerosis, statins are indicated. For high blood pressure, antihypertensive drugs are prescribed.
Brain infarction
Often the perivascular spaces are dilated in patients who have suffered a cerebral infarction. This disease is a consequence of prolonged ischemia. In some cases, cerebral infarction is asymptomatic and goes unnoticed by the patient. Its consequences can only be seen in an MRI scan.
It is important to remember that if the patient has risk factors (high blood pressure, atherosclerosis, diabetes), then the heart attack may recur in severe form. To prevent a recurrent attack of acute ischemia, patients are prescribed antihypertensive medications, hypoglycemic agents, and blood thinners.
Additional diagnostic methods
What to do if the MRI results indicate that you have dilated perivascular Virchow-Robin spaces? It is necessary to show the transcript of the study to a neurologist. Only a specialist can determine whether this is a variant of the norm, an age-related feature, or a sign of pathology.
There are cases when MRI does not reveal any changes in the brain, but the image shows dilated perivascular Virchow-Robin spaces. What does this mean? As a rule, such a sign does not indicate pathology. Doctors consider an increase in criblures only in combination with other changes identified during an MRI examination.
If necessary, the doctor may prescribe additional tests:
- multislice computed tomography;
- vascular angiography;
- Dopplerography;
- cerebrospinal fluid examination.
Let's take a closer look at the most common diseases and conditions that can lead to expansion of criblures.