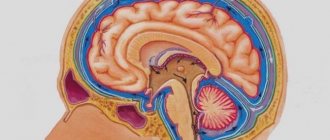
Atrophic hydrocephalus of the brain is characterized by excessive accumulation of cerebrospinal fluid in the cerebrospinal fluid cavities of the brain. The pathological process develops against the background of diseases that cause atrophy of brain tissue. Moderate asymmetric hydrocephalus occurs when one of the ventricles of the brain expands. Atrophic hydrocephalus is asymptomatic for a long time. To identify signs of the disease, neurologists at the Yusupov Hospital conduct a comprehensive examination of patients.
The Neurology Clinic has created all the conditions for the treatment of patients with atrophic hydrocephalus. The rooms are equipped with air conditioning, allowing you to create a comfortable temperature regime. Patients are provided with individual personal hygiene products and dietary nutrition. The staff of the neurology clinic is attentive to the wishes of all patients.
The Yusupov Hospital employs candidates and doctors of medical sciences, leading experts in the field of hydrocephalus treatment. Doctors of the highest category have the necessary knowledge and experience and apply individual treatment regimens for patients depending on the cause and severity of the disease. Specialists at the rehabilitation clinic use modern methods of restoring neurological functions, perform massage, conduct manual therapy and a course of physical therapy.
Causes
Atrophic hydrocephalus develops against the background of the following diseases:
- tumors of the ventricles and brain matter;
- toxic and alcoholic encephalopathies;
- infectious brain lesions (ventriculitis, encephalitis, meningitis);
- vascular cerebral pathology, including rupture of an aneurysm and intraventricular and subarachnoid cerebral hemorrhages resulting from defects in arteriovenous connections;
- pathologies of the development of the nervous system (Dandy-Walker syndrome, stenosis of the Sylvian aqueduct);
- post-traumatic conditions and brain injuries.
In atrophic encephalopathy, cerebrospinal fluid fills the space formed inside the skull as a result of a decrease in brain volume. Atrophic hydrocephalus of the brain in elderly and senile people can develop against the background of impaired blood supply to the brain due to arterial hypertension, atherosclerosis of cerebral vessels, and diabetic angiopathy.
Causes of cortical atrophy development
The reasons for the development of age-related atrophic processes in the brain are complex. Thus, the following factors influence the formation of senile dementia:
- Impaired blood supply to brain tissue due to a significant decrease in vascular capacity (atherosclerosis)
- Deterioration of blood oxygen saturation, which contributes to chronic ischemic phenomena in the nervous tissue
- Activation of genetic factors of predisposition to atrophic phenomena
- Deterioration of the body's regenerative abilities
- Significant reduction in mental workload
It is important! In addition to all of the above, the chances of developing brain atrophy in old age depend to some extent on the level of mental development of the patient in his youth. It has been proven that people who have a high level of intelligence, speak foreign languages, and actively work intellectually are less susceptible to developing senile dementia.
Congenital cortical cerebral atrophy, in fact, is hypoplasia of the organ, since in this case its initial normal formation does not occur, in relation to which atrophy develops. However, in most cases this process is also called atrophic.
In some cases, atrophic phenomena can develop in adulthood. So, the factors in the formation of the disease in this case are:
- Injuries, especially those accompanied by the development of cerebral edema. In this case, compression of blood vessels often occurs, ischemia of brain tissue and their atrophy.
- Toxic effects (chronic alcoholism). One of the features of the effects of alcohol metabolites on the body is the destruction of neurons. Restoration of the affected nervous tissue under conditions of ongoing intoxication does not occur, which is the cause of the development of atrophy.
- Tumors and cysts, which also lead to pinching of blood vessels. As a rule, neoplasms with frozen growth, which have a long-term moderate negative impact, are important in the formation of atrophy. Growing tumors simply do not have time to lead to the development of atrophy.
- In rare cases, the development of the disease may be caused by a history of neurosurgery.
Degrees and types
Acquired hydrocephalus develops after injury or disease of the brain. The cause of congenital hydrocephalus is infectious lesions of the brain during intrauterine development of the fetus. Internal hydrocephalus of the brain in adults is characterized by impaired distribution of cerebrospinal fluid due to the formation of blood clots, neoplasms or adhesions. Internal open hydrocephalus of the brain occurs due to the destruction of part of the brain matter, due to which the cerebrospinal fluid does not have a complete outflow of cerebrospinal fluid.
Based on the location of the cerebrospinal fluid, the following types of hydrocephalus are distinguished:
- moderate external hydrocephalus - accumulation of cerebrospinal fluid passes in the subarachnoid space;
- moderate internal hydrocephalus, characterized by the accumulation of cerebrospinal fluid in the ventricular space;
- mixed replacement hydrocephalus occurs due to the accumulation of cerebrospinal fluid both under the meninges and in the ventricular space.
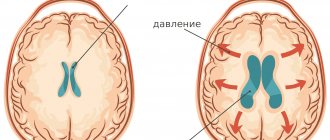
Internal asymmetric hydrocephalus develops when one of the ventricles of the brain expands. According to the severity of the disease, neurologists distinguish stabilized, progressive and regressive hydrocephalus.
Therapy of atrophic pathology of the brain and prognosis of the disease
It is important! Age-related atrophy of the cerebral cortex cannot be completely cured. In this case, maintenance therapy is carried out aimed at slowing the development of symptoms of the disease. Atrophies acquired at a young age at their initial stage can be corrected provided the etiological factor is eliminated.
Drug treatment of atrophic brain pathology involves the use of the following groups of drugs:
- Drugs that improve brain metabolism and blood circulation in it (nootropic drugs). The most prominent representatives of this pharmacological group are: piracetam, Cerepro, Ceraxon, Cerebrolysin. Their administration leads to a significant improvement in the patient’s thinking abilities.
- Antioxidants (mexidol). They have a stimulating effect on regeneration processes, slow down atrophy, help increase metabolic rate, and counteract oxygen free radicals.
- Drugs that improve blood microcirculation. The most commonly prescribed drug is trental (pentoxifylline). The drug has a vasodilating effect, increases the lumen of capillaries, improves blood microcirculation and gas exchange through the vascular wall.
Some signs of cortical atrophy require symptomatic therapy. For headaches, patients are recommended to take non-steroidal anti-inflammatory drugs.
In addition to the use of medication, it is necessary to monitor the patient’s neuropsychic state. Moderate physical activity, daily walks in the fresh air, and self-care procedures are recommended. If the patient is in a neurasthenic state, the use of mild sedatives is indicated.
Rate this article:
(votes: 8 , average: 4.63 out of 5)
Loading...
Related posts:
- What is bronchial atrophy and how to treat it
- Brain atrophy: causes, pathogenesis and signs
- Problems of dental transplantology and atrophy of the alveolar process of the jaw
- Spinal muscular atrophy and prognosis of this disease
- Causes and signs of leg muscle atrophy, as well as the basis for its recovery
- Causes, symptoms and treatment of atrophy of the frontotemporal regions
Symptoms
For a long time, patients may not notice signs of replacement hydrocephalus. Computed tomography or magnetic resonance imaging allows you to establish the correct diagnosis. These research methods at the Yusupov Hospital are used by all patients immediately after hospitalization at the neurology clinic.
In the presence of subacute and acute occlusive hydrocephalus of the brain, patients feel a bursting headache, which is accompanied by nausea and vomiting, which brings relief. There is a feeling of pressure on the eyeballs, a feeling of “sand” in the eyes, a burning sensation in the eyeballs. With increased cerebrospinal fluid pressure, drowsiness is noted, which is a sign of disease progression.
Patients experience a feeling of “fog” before the eyes, and vision deteriorates. In the fundus, ophthalmologists identify congested optic discs. If the patient does not promptly seek qualified medical help, then an increase in the amount of cerebrospinal fluid leads to the appearance of dislocation syndrome, which threatens the patient’s life. Depression of consciousness rapidly increases, paresis of upward gaze develops, depression of reflexes, divergent strabismus develops, and coma develops. These symptoms appear when the midbrain is compressed. In the case of compression of the medulla oblongata, the voice changes, swallowing is impaired, respiratory and cardiac activity are depressed, which can lead to death.
With chronic internal hydrocephalus of the brain in adults, intracranial pressure may be normal or slightly increased. Initially, the sleep cycle is disrupted, drowsiness or insomnia appears. Patients complain of fatigue, lethargy, and memory impairment. As the disease progresses, cognitive impairment, including dementia, develops. Patients behave inappropriately and lose the ability to self-care.
Walking is impaired, the gait becomes unstable and slow. Over time, difficulty arises when starting to move, and uncertainty in a standing position. The patient can imitate cycling or walking in a sitting or lying state, but in an upright state he loses this ability. The gait becomes “magnetic”: the person seems to be glued to the floor, and, leaving his place, takes short shuffling steps on widely spaced legs. Neurologists determine an increase in muscle tone; in severe stages of the disease, paresis of the lower extremities appears and muscle strength decreases. Balance disorders may progress and the patient may become unable to sit or stand independently over time.
Subsequently, urination becomes more frequent, especially at night. There is an urge to urinate, requiring immediate emptying of the bladder. Over time, urinary incontinence develops. Neurologists at the Yusupov Hospital use the following methods for diagnosing atrophic hydrocephalus:
- magnetic resonance or computed tomography, which allows you to determine the size and shape of the cisterns of the brain, ventricles and subarachnoid space;
- radiography of the tanks, with the help of which the type of hydrocephalus is clarified and the direction of the cerebrospinal fluid flow is determined;
- diagnostic test spinal puncture with collection of 40-55 ml of cerebrospinal fluid, accompanied by a short-term improvement in the patient’s condition;
- ultrasound examination of cerebral vessels to determine the state of arterial and venous blood flow.
After analyzing the results of a comprehensive study, individual treatment is prescribed. The tactics for managing patients with severe hydrocephalus are developed at a meeting of the expert council with the participation of professors and doctors of the highest category. Neurosurgeons determine indications for surgical intervention.
Focal cortical atrophies (FCAs) are rare degenerative diseases of the nervous system associated with selective atrophy of individual lobes of the cerebral cortex [1, 2, 4]. Due to the lack of epidemiological studies, their true frequency is unknown. PKA belongs to the class of tauopathies, as they develop due to the pathological accumulation of fragments of phosphorylated t-protein in neurons of the parieto-occipital and temporal lobes. As a result, damage to cell membranes, an increase in the content of intracellular calcium, disturbances in the functioning of mitochondria of the respiratory chain and, as a consequence, apoptosis of neurons are observed [7]. The formation of various FKA phenotypes is associated with a certain anatomical dysfunction of t-immunoreactive structures, the ultrastructure of t-filaments and various haplotypes of the t-protein gene [8]. The causes of selective atrophy of individual areas of the cerebral cortex are unclear. The clinical spectrum of FKA includes posterior cortical atrophy and primary progressive isolated aphasia (ICD-10 G31.0) [1]. The nosological status of FKA has not been definitively determined. Thus, a number of researchers [3, 5, 10] classify them as atypical forms of Alzheimer’s disease or corticobasal degeneration. The extreme rarity of FCA explains significant difficulties in diagnosing this pathology in the daily practice of neurologists. Often, patients with FCA come to the attention of doctors of other specialties (ophthalmologists, angiosurgeons) and even undergo unjustified surgical interventions, which delays the appointment of differentiated therapy.
Over the past 5 years, several cases of FCA have been observed in the neurological departments of the 5th Clinical Hospital in Minsk. When making a diagnosis, frequent diagnostic errors were noted, which prompted their analysis and comparison of our own observations with literature data.
Patient D.
, 68 years old, disabled group II, right-handed, was admitted to the hospital with complaints of visual impairment and decreased memory for current events. He was ill for 4 years, when gradually, for no apparent reason, he noticed difficulty in perceiving visual information. During this period, he could look at an object and sometimes not recognize it, had difficulty recognizing the faces of friends and family members, read text written only in a special font, and began to have difficulty navigating familiar streets, which, in his words, began to “look somehow strange.” Despite visual impairments, he continued to work as a chief designer, but repeatedly consulted an ophthalmologist and was observed for glaucoma, which was excluded by dynamic measurement of intraocular pressure. Subsequently, he was referred to a neurologist for consultation, and Doppler ultrasound of the brachiocephalic arteries was performed, which revealed pathological tortuosity of the internal carotid artery on the left and kinking on the right. The specialists associated the patient’s complaints with these changes and in the angiosurgery department performed a reconstructive operation of resection of the internal carotid artery on the left with elimination of the loop formation (2010), which did not bring improvement. The patient's condition has noticeably worsened over the past year, when, due to visual impairments, he began to move independently with difficulty, decreased memory, the inability to read text in any font, count, and lost 10-20 kg for no apparent reason. He has been examined many times in neurological institutions in our country and in a number of clinics in the USA. Various diagnoses were made: ischemic optic neuropathy, Alzheimer's disease, degenerative disease of the central nervous system. Disability group II has been established. Repeated magnetic resonance imaging (MRI) of the brain excluded ischemic or tumor damage. I took Aricept (donepezil) 5 mg/day and Namenda (memantine) 10 mg/day with some improvement in my condition. Among the previously suffered diseases, he noted rare colds, sometimes increased blood pressure (BP), and benign prostatic hyperplasia. Denied smoking, drinking alcohol or other toxic substances. Higher education, no family history. There were no cases of early dementia in the family: the mother died at the age of 89, the father died young during the Great Patriotic War, two adult sons are healthy. Currently he lives alone, and therefore self-care is significantly difficult.
Objectively upon admission: general condition is satisfactory, low nutrition, blood pressure 130/80 mm Hg, rhythmic pulse 68 beats/min. There is a postoperative scar along the front surface of the neck on the left. No somatic pathology was identified. In consciousness, partially oriented in place and time. Speech is free. The mood is even, behavior is adequate, criticism of one’s condition is somewhat reduced. The memory is weakened, he names the main historical events, but does not remember the age of his youngest son. Serial counting is difficult, he performs multi-step tasks with errors, and is not always able to identify household items by touch (furniture, clothing, keys, etc.). Does not write and cannot read any text. Mini-Mental State Examination (MMSE) score: 16 points (cognitive decline). Performs tests of the frontal dysfunction battery satisfactorily, with the exception of attention tasks when repeating movements, but at the same time he tries to imitate given movements by ear. Associative thinking is impaired: when explaining the main differences between a bird and an airplane, he only names their different wing geometry (an aircraft designer by profession) and the pilot’s control. Cranial nerves: pupils are equal in size, direct and friendly reaction to light is preserved, movements of the eyeballs are complete, distorted color perception (yellow is perceived as red - achromatopsia). The face is symmetrical, the tongue is in the midline, the Marinescu-Radovici reflex is moderately expressed on both sides. Swallowing is not impaired, the soft palate is mobile. The range of motion in the limbs is full, muscle tone is not changed. Tendon-periosteal reflexes are of average vivacity, D=S, there are no pathological foot signs. All types of sensitivity (superficial, deep muscle, two-dimensional-spatial) are preserved. Performs finger-nose and knee-heel tests satisfactorily. The functions of the pelvic organs are not impaired. Walking independently is difficult due to lack of vision control (optical ataxia), but when supported by an accompanying person, the gait is not significantly impaired.
Examination: routine general clinical and biochemical blood tests (including multiple tests for total cholesterol and triglycerides) - without deviations from the norm. In blood serum: vitamin B1 - 59 nmol/l (normal 70-180 nmol/l); vitamin B12 - 440 pg/ml (220-1000 pg/ml); free T4 - 0.9 ng/dl (0.9-1.8 ng/dl); thyroid-stimulating hormone - 1.63 ng/dl (0.35-5.5 ng/dl). ECG: sinus rhythm, horizontal position of the electrical axis of the heart. Ultrasound of the brachiocephalic arteries 6 months after surgery: kinking of the right internal carotid artery with an increase in the linear velocity of blood flow to 128 cm/s, main type; blood flow in the left internal carotid artery is free, the course is straight, moderate hypertonicity in all branches, compression tests are unremarkable. Ultrasound of the heart: atherosclerosis of the aorta and valve structures, systolic function is satisfactory, the chambers of the heart are not dilated. Consultation with a urologist: stage I benign prostatic hyperplasia. Repeatedly examined by an ophthalmologist: visual acuity cannot be checked; When examined with a fundus lens, the optic discs have a grayish tint, there is no edema. Electroretinography: response from both eyes of normal amplitude and shape to all types of stimuli. Tomography of the optic nerve: the structure of the nerve layers in all segments is preserved (Fig. 1).
| Rice. 1. Tomography of the optic nerve of patient D., 68 years old, diagnosed with posterior cortical atrophy: the structure of the nerve layers in all segments is preserved. |
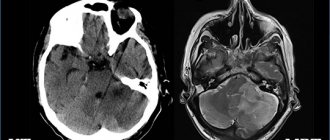
Visual evoked potentials: evidence of bilateral deterioration of visual afferentation to the cortex, more pronounced with stimulation of the left eye. MRI of the brain: expansion of the cortical grooves and ventricles of the brain, expressed in the occipital and parietal lobes, more on the right (Fig. 2).
| Rice. 2. MRI of the brain of the same patient: expansion of the cerebral ventricles and cortical sulci (a), more pronounced in the occipital and parietal lobes on the right (b). |
| ]]> |
| Rice. 2. MRI of the brain of the same patient: expansion of the cerebral ventricles and cortical sulci (a), more pronounced in the occipital and parietal lobes on the right (b). |
| ]]> |
Thus, the patient, aged 64 years, gradually developed visual agnosia, which was initially mistakenly regarded as a pathology of the organ of vision. Subsequently, visual disturbances were explained by chronic cerebrovascular insufficiency in the carotid artery basins due to their kinking and cowling, and even an unsuccessful reconstructive operation was performed. Meanwhile, post factum detected changes should be considered clinically insignificant. Subsequently, after 3 years, cognitive impairment of the cortical type, achromatopsia, acalculia, optical ataxia, apraxia and weight loss were added. Laboratory and instrumental examinations made it possible to exclude pathologies of the eyes, optic nerves, and other somatic or neurological pathologies. A pronounced local bilateral atrophic process, predominant in the parietal and occipital lobes, more on the right, discovered during MRI of the brain, confirmed the diagnosis of posterior cortical atrophy. Combination therapy with cholinergic drugs (dopenesil and akatinol) led to stabilization of the process. A comparison of clinical manifestations, dynamics of the process and examination results in our patient with literature data confirmed their almost complete similarity, with the exception of weight loss, which had not previously been found in the literature.
Posterior cortical atrophy (PCA, Benson's syndrome, visual variant of Alzheimer's disease) as an independent nosological form was first described by F. Benson in 1988 [cit. according to 6]. The author summarized the results of an examination of 5 patients with early development of a complex of visual impairments and progressive dementia.
Subsequently, the mean age of onset was found to be 58 years (range 51 to 64 years). All researchers emphasize the rarity of this pathology. Thus, in a specialized clinic in Lyon in 2001, the share of PCA in the structure of all cases of dementia was only 4% (6 out of 154 new patients with various causes of dementia). The onset of the disease is gradual over several years. The initial manifestations of PCA are visual agnosia and apraxia, which remain the leading symptoms throughout the disease [1, 3].
Visual agnosia is an obligate symptom of PCA, characterized by the inability to identify and identify individual objects or people, despite knowledge of their characteristics, which is associated with damage to the occipital lobes [6, 10]. The complex of visual disturbances in PCA may include elements of Balint's syndrome (optical ataxia, oculomotor apraxia), apperceptive visual agnosia (difficulty in recognizing the features of an object, while its naming is not impaired), alexia, disorientation (patients can get lost in a familiar place), simultaneous agnosia (difficulty in general recognition of an object), prosopagnosia (inability to recognize familiar faces). Unusual visual disturbances in PCA include patients being more fluent in reading small text or unusual font; they see distant objects better than nearby ones [3, 5].
Apraxia in PCA is manifested by difficulties in performing simple and complex movements while maintaining the physical ability to perform them, which is explained by damage to the parietal lobes. Patients with PCA may experience constructive apraxia (the inability to perform a simple configuration or drawing), the inability to dress or undress independently, ideomotor (the inability to perform symbolic gestures) and ideational (impaired creation of a plan for complex movements, use of household appliances or accessories) apraxia. In PCA, Gerstmann's syndrome has been described, which is manifested by agraphia, acalculia, left- or right-sided disorientation, and finger agnosia [1, 5, 6].
Mild cognitive impairment occurs already in the early stages of PCA. Subsequently, they may increase, but never reach the level of severe dementia as in Alzheimer's disease [3]. Speech and motor areas are usually intact. Affective disorders are not observed in patients with PCA, and their behavior resembles that of blind people. The course of the disease is slowly progressive and typically ends in death after 8-12 years, usually from somatic causes, more often from bronchopneumonia [3, 5].
Diagnosis of PCA is based on neurological examination and results of neuropsychological testing. To date, there are no laboratory biomarkers of PCA in serum and cerebrospinal fluid. Neuroophthalmological examination usually does not reveal pathology, but homonymous hemianopsia may be observed. On MRI of the brain, a typical manifestation of PCA is bilateral predominantly parieto-occipital atrophy, more pronounced in the right hemisphere [3]. Unlike Alzheimer's disease, PCA does not show atrophy of the hippocampus and temporal lobes. With single-photon and positron emission tomography, symmetrical areas of hypoperfusion or hypometabolism in the occipital and parietal lobes are typical [3, 5, 6, 10]. Differential diagnosis of PCA is carried out with Creutzfeldt-Jakob disease, tumors or infarctions of the brain in the parietal or occipital localization, and Alzheimer's disease. Treatment of PCA consists of long-term use of cholinergic drugs in an adequate dose and periodic courses of neuroprotectors.
The second observation illustrates the classic course of primary progressive isolated aphasia, in the diagnosis of which diagnostic errors were also observed.
Patient M.
, 66 years old, right-handed, disabled group II (previously worked as an operator), upon admission to the neurological department of the 5th clinical hospital in Minsk, she did not make any complaints due to speech disorders. From the words of relatives and analysis of medical documentation, it was clarified that she had been ill for 3 years, when those around her gradually noticed her “poverty” of speech, difficulty in finding words, and could not always remember the names of objects. The speech disorder slowly increased, which forced the patient to consult a neurologist at the district clinic. Suspected of a cerebral infarction, she was sent for emergency hospitalization to one of the neurological departments in Minsk, where after an examination this diagnosis was confirmed. She was discharged from the hospital with a diagnosis of atherothrombotic cerebral infarction in the left carotid system with moderate motor aphasia, despite the fact that there were no paresis of the limbs, MRI of the brain showed only a diffuse atrophic process, and ultrasound of the great vessels of the head and neck showed only hemodynamically insignificant disorders. Courses of antioxidants, antihypoxants, and nootropics were prescribed—without effect. Speech impairments progressed; therefore, a year later she was hospitalized in the neurological department of another hospital, from where she was discharged with a diagnosis of discirculatory encephalopathy stage II on the background of a cerebral infarction in the left carotid system (no paresis of the limbs was noted in the epicrisis, a repeat MRI also did not reveal any in the brain focal disorders). For this reason, disability group II was established. Speech disorders continued to increase, which forced relatives to go to a third medical institution. Among the previously suffered diseases, she noted calculous cholecystitis, polyosteoarthrosis, and “mild” arterial hypertension (she was inconsistently taking antihypertensive drugs). There is no family history (including dementia).
Objectively upon admission: the patient’s general condition is satisfactory, she has increased nutrition (height 160 cm, body weight 98 kg). Restriction of movement and deformation of both knee joints. Respiratory rate 16/min, blood pressure 130/80 mm Hg, pulse 76 beats/min, rhythmic. No somatic pathology was identified. In consciousness, productive contact is not available. Spontaneous speech is completely absent. Partially understands spoken speech and follows simple instructions. Reading, writing and counting are impaired. The pupils are equal in size, their reaction to light is preserved. The face is symmetrical, slight deviation of the tongue to the right. The strength in the limbs is sufficient, muscle tone is not changed. Tendon-periosteal reflexes are live, D=S, there are no pathological foot signs. Sensitivity cannot be reliably verified. Statics, coordination and gait are not changed. Controls the function of the pelvic organs.
Examination: general clinical blood test - no pathology. In a biochemical blood test, except for an increase in the level of total cholesterol to 6.6 mmol/l, no other abnormalities were detected. ECG: moderate sinus bradycardia, deviation of the electrical axis of the heart to the left. Oculist: it is impossible to check visual acuity; in the fundus, the veins are dilated and the arteries are narrowed. X-ray of the knee joints: pronounced narrowing of the joint spaces, marginal bone growths. Consultation with a speech therapist: severe sensorimotor aphasia. MRI of the brain: diffuse expansion of the ventricular system and cortical sulci, more pronounced in the left hemisphere of the brain. Single photon emission tomography: focus of hypoperfusion in the left frontotemporal region. She received anticholinesterase drugs (neuromidin), pentoxifylline, mildronate without effect. During follow-up, the patient's condition continued to deteriorate. A year later, total aphasia developed, and after 2 years she stopped moving independently, mainly due to apraxia of walking, along with a diffuse increase in muscle tone of the extrapyramidal type, mild right-sided hemiparesis and extensive bedsores. She died at home 6 years later from the first symptoms of the disease; no autopsy was performed.
Thus, a 63-year-old patient gradually developed dysphasia, then isolated motor, and a few years later sensorimotor aphasia, alexia, agraphia and acalculia. These focal symptoms of damage to the higher cortical functions of the dominant hemisphere were initially mistakenly regarded as a cerebral infarction, and then as chronic cerebrovascular insufficiency against the background of residual phenomena after a cerebral infarction in the left carotid system. Meanwhile, the patient had no clinical and instrumental signs of cerebral infarction, and her motor sphere remained completely intact. Only 4 years after the onset of the disease, a diagnosis of primary progressive isolated aphasia was made, confirmed by single-photon emission tomography.
Primary progressive aphasia (PPA) is another clinical form of PCA, the development of which is associated with predominant atrophy in the speech areas of the cortex of the dominant hemisphere while other parts of the brain are intact [1]. With this pathology, patients experience an isolated speech disorder for several years. In the literature [2, 8], PPA is usually divided into three forms depending on the location of atrophy detected on neuroimaging: primary progressive motor aphasia (PPMA), semantic dementia (SD), and logopenic aphasia (LA). PPMA develops with atrophy of the insula and the posterior part of the left frontal lobe, including Broca's area. At the onset, patients’ speech is characterized by agrammatism, difficulty in choosing words and names of objects, slowness, and short phrases. Impressive speech is not impaired. As the process progresses, complete apraxia of speech develops [4, 9]. SD is manifested by a lack of understanding of phrases with complex constructions (father's brother, brother's father), the meaning of prepositions, suffixes, endings, word meanings and speech formulas with spatial relationships. This pathology develops with asymmetric atrophy of the anterior part of the temporal lobe on the left [8]. LA is characterized by a disorder in understanding one's own and others' speech, lack of control, and paraphasia (omissions, substitutions, repetition of sounds or words). The advanced stage of LA is characterized by a “word salad” in the form of an abundance of incomprehensible speech products. The morphological pattern of atrophy in this form is localized in the posterior part of the temporal and lower part of the parietal lobe on the left [2]. After 5-8 years from the onset of the disease, the degenerative process in any form of PPA spreads to the gray and white matter of other parts of the brain, which explains the addition of motor disorders, apraxia and dementia in the clinical picture in these patients [9]. The diagnosis of PPA is confirmed by an asymmetric atrophic process in the frontotemporal region of the dominant hemisphere on MRI and the detection of a hypoperfusion zone there on single-photon emission tomography. A comparison of the clinical manifestations, dynamics of the process and examination results in our patient with literature data confirmed the classic course of PPMA.
Thus, focal cortical atrophies are rare clinical forms of neurodegenerative diseases of the central nervous system, which are distinguished by the selective localization of the atrophic process in individual lobes of the brain and have significant clinical polymorphism. Their etiology and pathogenesis have not yet been fully elucidated. In our opinion, FKA is a neurological syndrome, which, despite its common pathogenesis and pathomorphology, is significantly different from Alzheimer's disease and corticobasal degeneration. Knowledge by practicing doctors of the features of their clinical picture allows them to avoid unnecessary examinations and surgical interventions, timely prescribe differentiated therapy and correctly resolve expert issues.
Treatment in an adult
For increased intracranial pressure, neurologists at the Yusupov Hospital prescribe diuretics. Mannitol, mannitol and diacarb in combination with furosemide or lasix have a diuretic effect. To prevent hypokalemia, they are used simultaneously with asparkam or panangin.
To improve the nutrition of brain tissue, Actovegin, Cavinton choline, gliatilin, Cerebrolysin, Cortexin, Memoplant, Semax are prescribed. These drugs have a nootropic effect. In case of severe atrophic hydrocephalus, neurosurgeons at partner clinics perform surgical interventions.
If the patient's condition is life-threatening, craniotomy is performed and external drains are installed to allow excess fluid to escape. Medicines are administered through the drainage system. Such an operation for hydrocephalus of the brain is traumatic.
Endoscopic ventriculocisternostomy of the ventricular fundus is a minimally invasive surgical procedure. Neurosurgeons insert a microscopic surgical instrument with a camera at the end into the ventricles of the brain, which makes it possible to monitor all procedures. An additional hole is made at the bottom of the ventricle, which is connected to the cisterns of the brain. The operation allows you to eliminate the cause of the disease and normalize the physiological flow of cerebrospinal fluid between the cisterns and ventricles.
Atrophic hydrocephalus of the brain in adults is a dangerous disease that leads to irreversible changes in the substance of the brain. At the slightest suspicion of hydrocephalus, call the Yusupov Hospital. After the examination, neurologists will prescribe treatment to slow the progression of hydrocephalus symptoms.