Causes of encephalitis
The main cause of this disease is an infectious lesion, which can be:
- Viral etiology (occurs in most cases). The following groups of viruses can be distinguished that are tropic (targeted to damage) the nervous system: viruses of the herpes group (herpes simplex virus types 1 and 2, varicella zoster virus, cytomegalovirus, Epstein-Barr virus);
- enteroviruses;
- paramyxoviruses (measles, mumps virus);
- arboviruses (tick-borne, Japanese encephalitis);
- adenovirus;
- influenza virus, parainfluenza;
- HIV infection.
Encephalitis can also occur as a complication after vaccination.
Types of encephalitis
Depending on the cause of occurrence, the following types of this disease are distinguished:
- Primary is an independent disease that is caused by an infection that affects the nervous system. It is divided into the following subtypes: viral (herpetic, arbovirus, influenza, tick-borne encephalitis virus, etc.);
- microbial.
- post-viral (as a complication of measles, rubella, etc.);
Depending on the location of the disease, it can be:
- cortical;
- subcortical;
- stem;
- cerebellar
According to the clinical course, they are distinguished:
- ultra-sharp;
- spicy;
- subacute;
- chronic;
- recurrent encephalitis.
Depending on the prevalence there are:
- leukoencephalitis (inflammation of white matter);
- polioencephalitis (inflammation of gray matter);
- panencephalitis (damage to both structures).
Tick-borne encephalitis
Encephalitis
Tick bite
Vomit
6147 01 February
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Tick-borne encephalitis: causes, symptoms, diagnosis and treatment methods.
Description
Tick-borne encephalitis is a dangerous viral infection that occurs in persistent natural foci and is manifested by high fever, intoxication and damage to the nervous system.
Causes of tick-borne encephalitis
The cause of the disease is an RNA-containing tick-borne encephalitis virus, which belongs to the genus of flavoviruses. Based on the composition of the genetic material and location of distribution, the Far Eastern, Ural-Siberian and Western subtypes are distinguished.
The virus is carried by ixodid ticks, which are also its main reservoir.
Thus, the virus is found where ixodid ticks live, the maximum increase in incidence is observed in May-June, and a second, less pronounced increase is recorded in late summer and early autumn, which is associated with the activity of ticks.
The virus cannot be transmitted from a person infected with tick-borne encephalitis to a healthy person.
The tick-borne encephalitis virus enters the human body in the first minutes of a tick bite or, which happens much less frequently, with the milk of an infected goat, or even less often, a cow. The virus initially multiplies and accumulates in the cells of the immune system, then enters the bloodstream and enters the lymph nodes, liver, spleen and other organs. There it multiplies and attacks the nerve cells of the cervical spinal cord, cerebellum, meninges, remaining there for a long time and penetrating deeper into the brain tissue.
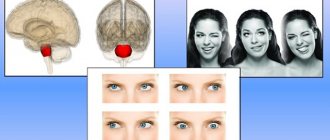
Classification of the disease
The disease can occur in acute
or
chronic
form.
Non-focal acute forms are distinguished
, in the clinical picture of which it is impossible to identify a specific damaged structure of the nervous system, and
focal acute forms
with symptoms indicating the localization of damage to the nervous system.
The severity of the condition with tick-borne encephalitis can be mild , moderate and severe
.
Symptoms of tick-borne encephalitis
The incubation period (from the moment of infection to the first clinical manifestations) averages 7–12 days, but can vary from 1 to 30 days. Rarely during this period, precursors of the disease occur - general malaise, weakness in the muscles of the limbs and neck, numbness of the facial skin, headache, insomnia, nausea.
The disease begins acutely: with an increase in body temperature to 38–40°C, symptoms of intoxication (severe weakness, fatigue, sleep disturbances), as well as symptoms of irritation of the membranes of the brain (nausea, vomiting, severe headache, inability to press the chin to the chest ).
There is lethargy, confusion, redness of the face, neck, and upper half of the body. The patient may feel pain in the muscles of the whole body, most severely where movement disturbances will subsequently be observed; There may be numbness in areas of the skin or a sensation of crawling, burning, etc.
As the disease develops, the main symptoms appear, which determine its form. Most often, tick-borne encephalitis occurs according to the following clinical variants:
- in the form of fever
, lasting 3-5 days with symptoms of general intoxication, but without signs of damage to the nervous system. The outcome is a rapid recovery; - in the form of damage to the membranes of the brain
(most common in adults), which is manifested by unbearable headache, dizziness, nausea and vomiting that does not bring relief, photophobia; lethargy and lethargy appear. Body temperature is elevated, fever lasts 7–14 days. The prognosis is favorable; - in the form of damage to the membranes and substance of the brain
, when the symptoms of irritation of the meninges are accompanied by disturbances in movements in the limbs, including paralysis, visual impairment, hearing, speech, difficulty swallowing, etc. Sometimes convulsive seizures occur. The patient is poorly oriented in place and time, delusions and hallucinations are often observed. Recovery takes a long time, and movement disorders often remain for life. This is a severe form of tick-borne encephalitis, so death cannot be ruled out; - in the form of damage to the spinal cord
with the development of movement disorders (paresis and paralysis) in the muscles of the neck and limbs; - in the form of damage to nerve roots
and fibers with the development of disturbances in sensitivity and movement in the limbs.
Tick-borne encephalitis with a two-wave course of fever
is distinguished separately . The first rise in temperature is relatively mild, accompanied by symptoms of intoxication and irritation of the meninges, and the second (after a two-week break) with the development of a full clinical picture with signs of damage to the nervous system. Despite this, the prognosis is favorable, although transition to the chronic stage is possible.
Tick-borne encephalitis in children most often occurs in the form of fever or with signs of damage to the membranes of the brain.
Immunity to the virus after tick-borne encephalitis is lifelong.
Diagnosis of tick-borne encephalitis
To diagnose tick-borne encephalitis, it is necessary to confirm the fact of tick bite and the place where it occurred (find out whether the area is endemic for tick-borne encephalitis), clarify whether the patient has been vaccinated and whether immunoglobulin has been administered to him.
The doctor carefully examines the patient and conducts a complete neurological examination. It is important to exclude the possibility of other diseases, both infectious and non-infectious, accompanied by similar symptoms.
Laboratory diagnosis of tick-borne encephalitis includes determining the presence and increase in dynamics of the titer of IgM class antibodies and IgG class antibodies in the blood to the tick-borne encephalitis virus.
Symptoms of encephalitis
Clinical manifestations and severity of the disease depend on the age of the child, the state of reactivity of the body, the type of infectious agent, the nature and location of the lesion in the central nervous system. The younger the child, the more severely he suffers from this disease.
In most cases, this disease begins acutely, after a viral infection, but subacute onset of the disease is also possible. The following symptoms are characteristic of this disease:
- fever , feeling of nausea, vomiting that does not bring relief;
- memory loss , headache, adynamia, apathy, visual impairment and decreased intelligence (more typical for older children);
- emotional and mental disorders;
- drowsiness , irritability, weakness, moodiness, refusal to eat (typical for infants);
- conduct disorder;
- disturbance of consciousness , from stupor to coma;
- increase in focal neurological symptoms (unsteadiness of gait, speech impairment, paresis, paralysis);
- seizures.
Encephalitis in children
Primary encephalitis
Epidemic encephalitis. Children in the first 10 years of life rarely get sick, but their disease (especially under the age of 5 years) is severe. The causative agent of epidemic encephalitis has not been determined. The structures of the brain that are directly adjacent to the cerebrospinal fluid pathways are predominantly affected. In the acute stage of epidemic encephalitis, ptosis, strabismus, double vision, gaze paresis in combination with sleep disturbance are often observed, often in the form of severe drowsiness, hibernation against the background of a flu-like illness. The chronic stage, which can develop several months and even years after the acute stage, is characterized by parkinsonism syndrome. In children, body temperature rises, chills, vomiting, convulsions, and meningeal syndrome appear. In older children, symptoms develop gradually. Already in the acute stage of the disease, in addition to oculomotor and autonomic disorders, symptoms of damage to the brain system are observed, mainly in the form of hyperkinesis (choric, athetoid, myoclonic). Sometimes there are disturbances of the pyramidal and cerebellar systems, psychomotor restlessness appears, and vestibular disorders often occur. In the chronic stage, children and adolescents often experience mental changes, decreased intelligence, changes in character, and pathological desires (tendency to vagrancy, theft, hypersexuality, etc.).
Tick-borne and mosquito encephalitis. This disease is transmitted by blood-sucking insects from sick animals and birds. This infection is due to the seasonality of the insect life cycle, geographic location, and natural focality. The incubation period is 7-21 days. The following clinical forms of tick-borne encephalitis are distinguished:
Poliomyelitis and polioencephalomyelitis forms can take a chronically progressive course. The disease usually begins acutely: fever, headache, vomiting, impaired consciousness. In the polioencephalomyelitis form, there are disturbances in phonation and swallowing, respiratory and circulatory disorders are often observed, spinal cuts, paralysis of the muscles of the neck and upper limbs, and there may be death.
The meningeal form is the most common and is accompanied by high blood pressure. With this form, complete recovery is usually noted.
The cerebral form with predominant damage to the cerebral hemispheres is characterized by various disorders of consciousness and epileptic seizures.
The erased form proceeds as an acute febrile illness, without clear neurological symptoms.
Clinical symptoms develop quickly, with a high rise in body temperature, pronounced general infectious symptoms, have a difficult course, are accompanied by delusions, hallucinations, psychomotor agitation, and sometimes a coma. There may be epileptic seizures. Muscle hypertension is significantly pronounced, and decerebrate rigidity is sometimes observed. However, children more often than adults have a meningeal form with a favorable course.
Enteroviral encephalitis . Caused by various types of ECHO and Coxsackie viruses. There are the following forms of enteroviral encephalitis: brainstem, cerebellar, hemispheric.
The stem form is characterized by general cerebral symptoms - headache, fever, vomiting, impaired consciousness, and possible damage to the facial nerve.
With the cerebellar form in severe cases, the child cannot walk, stand, sit, and speech is impaired.
In the hemispheric form, general cerebral symptoms, epileptic seizures followed by the development of paresis and paralysis are usually observed, and hyperkinesis (involuntary movements) may be observed. Young children often experience epileptic seizures and unconsciousness. The course of enteroviral encephalitis is usually favorable, only in some cases (with damage to the medulla oblongata) it can be fatal.
Herpetic encephalitis. 10% of all encephalitis in children are caused by herpes viruses, most often type 2. Newborns may experience herpetic sepsis with damage to the liver, spleen and brain. The course of the disease is very severe. Severe general infectious and cerebral symptoms, epileptic seizures, paresis and paralysis, and meningeal symptoms are observed.
Polyseasonal encephalitis in children occurs throughout the year. Already on the 2-3rd day, focal symptoms appear. In younger children, a more severe course is observed with frequent seizures, unconsciousness, severe focal symptoms, and sometimes death. In older children, death is rare; complete recovery occurs, but more often certain focal symptoms, mental disorders, and epileptic seizures remain.
Secondary encephalitis
Secondary encephalitis includes encephalitis due to exanthemal infections and post-vaccination encephalitis. Characterized by a delayed onset of neurological symptoms, there is diffuse damage to the central nervous system with predominant damage to the white matter of the brain. Inflammatory foci are located mainly around medium and small veins (perivenous encephalitis).
Measles encephalitis. It appears on the 3-4th day of the rash, affecting the white matter of the hemispheres. Symptoms are expressed by disorders of consciousness of varying degrees - confusion, stupor, deep unconsciousness, coma. The second most common symptom is convulsions, which appear already in the first days of the disease and progress to paralysis or paresis of the corresponding limbs. Psychosensory disturbances, hallucinations, the development of parkinsonism syndrome, obesity, blindness such as retrobulbar neuritis with subsequent restoration of vision are possible. Spinal paralysis or paresis, dysfunction of the pelvic organs, inflammatory changes in the meninges are observed, and a transition to meningoencephalomyelitis is possible.
Chickenpox encephalitis. This is a complication of chickenpox. On the 3-8th day after the appearance of the rash, symptoms of neurological disorders appear. Disorders can begin to develop both with the appearance of the rash and at a later date. Young children are characterized by high fever, convulsions, vomiting, impaired consciousness, sensitivity and function of the pelvic organs, cerebellar and vestibular disorders, head tremors, unsteady gait, scanned speech, nystagmus, intention tremor, aphasia, agnosia.
Rubella encephalitis. Neurological disorders usually appear on the 3-4th day of the rash or from the 1st to the 15th day of the disease; they can rarely appear 1-12 days before the rash appears. Rubella encephalitis can develop without skin rashes. The disease begins in acute form with the appearance of high body temperature, headache, vomiting, and confusion; this is associated with edema-swelling of the brain. After which motor disorders appear in the form of myoclonus, opisthotonus, choreoathetosis, central paresis, damage to cranial nerves, cerebellar disorders, ataxia, hyperthermia, central respiratory and cardiovascular disorders. Children often experience disturbances of consciousness: mild confusion or deep coma.
Encephalitis due to pertussis-diphtheria-tetanus vaccination. Encephalitis that occurs after adsorbed pertussis-diphtheria-tetanus vaccine (DPT) has a wide range of symptoms: damage to cranial nerves, convulsions, hallucinations, paralysis or paresis, hyperkinesis, optic nerve atrophy, etc. The disease is severe with a high probability of mortality, Sick children have many residual effects, manifested by epileptic seizures and developmental delay.
Measles post-vaccination encephalitis is characterized by symptoms in the form of seizures and coordination disorders. Treatment occurs individually; in some cases there is a favorable result, in others there are pronounced residual effects.
Encephalitis due to rabies vaccinations. In children of the first years of life, the nervous system is rarely affected, unlike school-age children.
The disease occurs in acute or subacute forms. Various neurological disorders develop as a general malaise. Symptoms of myelitis, encephalomyelitis, meningoincephalomyelitis, encephalopolyradiculoneuritis may be observed. The most severe course is observed with ascending Landry's paralysis (starting in the lower extremities and spreading up the spinal cord).
Diagnosis of encephalitis
To establish a diagnosis, a detailed collection of medical history data is extremely important. Therefore, during a visit to the doctor, parents need to be prepared to answer the following questions:
- what diseases has the child recently had?
- whether there was contact with infectious patients during the last month;
- have there been any insect bites (mosquitoes, ticks);
- what diseases is the child vaccinated against?
- whether the child or any close relatives have traveled abroad in the last month.
The doctor also necessarily conducts a general and neurological examination of the child. After collecting anamnesis and examination, additional laboratory and instrumental studies may be prescribed:
- general blood analysis;
- general urine analysis;
- blood chemistry;
- coagulogram;
- lumbar puncture;
- microscopy of cerebrospinal fluid;
- bacteriological examination of cerebrospinal fluid with an antibiogram;
- serological blood test;
- PCR (polymerase chain reaction) of cerebrospinal fluid;
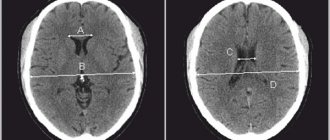
- MRI (magnetic resonance imaging) of the brain;
- CT (computed tomography) of the brain.
Treatment methods for encephalitis
Encephalitis is a serious and dangerous disease that requires timely and adequate treatment. Children with this disease must be hospitalized in the infectious diseases department or intensive care unit (depending on the severity of the disease). If necessary, the child is transferred to mechanical ventilation (artificial ventilation) and oxygen therapy is performed.
drug therapy individually for each patient, based on the causes and severity of the disease. The essence of drug treatment for encephalitis is to prescribe diuretics and glucocorticosteroids to reduce cerebral edema, drugs to correct water and electrolyte balance, antibacterial or antiviral drugs, depending on the etiological factor. In addition, symptomatic therapy is also important: anticonvulsants, antihistamines, NSAIDs (non-steroidal anti-inflammatory drugs), blood pressure correction agents, etc. Etiotropic therapy consists of prescribing antiviral drugs (for example, for herpetic or cytomegalovirus encephalitis), as well as immunoglobulins.
After overcoming a life-threatening period, additional treatment methods : physiotherapy, massage. Drug correction of such consequences of encephalitis as parkinsonism, hyperkinesis or epileptic seizures is also carried out.
Detailed description of the study
Infections carried by ixodid ticks are dangerous, and their symptoms are similar to each other. Some ticks can carry pathogens of several diseases at once, which complicates the course of the disease and complicates diagnosis.
Tick-borne encephalitis is a viral infection that affects the tissues of the brain and spinal cord and/or their membranes. You can get sick when ixodid ticks are active: in spring and summer. On average, 6 out of 10 ticks carry the virus across the country, but due to the uneven distribution of these insects, the likelihood of infection varies depending on the area. Regions in which a tick bite is likely to cause encephalitis are called endemic. In total, half of the country’s population lives in such territories. We have prepared a visual illustration of the prevalence of tick-borne encephalitis in Russia by region. https://www.gemotest.ru/news/119135/
A complete list of areas endemic for tick-borne encephalitis is provided on the Rospotrebnadzor website (https://www.mossanexpert.ru/novosti/?ELEMENT_ID=3386)
You can get sick not only from a tick bite. Domestic animals and birds can be carriers and sources of infection. Thus, you can become infected by consuming raw goat or cow milk. But tick-borne encephalitis is not transmitted from person to person.
When a virus enters the bloodstream, cells of the immune system capture it, but cannot neutralize it. It multiplies in them, new viral particles enter the lymph nodes, spleen, liver, where re-multiply occurs. When the number of viral particles has been increased, the virus enters the cells of the nervous system and meninges. Clinically, the disease begins acutely after an incubation period (7-35 days). Symptoms increase rapidly: the temperature rises to 38-39 °C, and a feeling of chills occurs. Weakness, drowsiness, headache and muscle pain, and possibly vomiting appear. All this lasts 2-4 days, after which relief occurs, which can be mistaken for recovery. Sometimes this is true, but in 20-30% symptoms return after a week. Due to damage to the nervous system, neurological pathologies are added. Motor disturbances occur: arms and legs begin to twitch or tremble, sometimes on the contrary - motor activity becomes more difficult to the point of paralysis, stiffness of the neck muscles occurs, which manifests itself in the inability to tilt the head or touch the chin to the chest. For the Far Eastern subtype of tick-borne encephalitis, the period of the disease is not typical: the disease begins even more acutely, the nervous system is affected already on days 3-5. The mortality rate from this subtype of the disease is higher: 20% versus 2% of the European form described above.
To prevent the disease, people living in or traveling to endemic regions are vaccinated. Immunity to tick-borne encephalitis develops within a month. If an infected tick bites a person, he is injected with anti-encephalitis serum. It is effective only for 4 days from the moment the tick bites. This is less than the incubation period, therefore, for timely measures to prevent infection, in the event of a tick bite, it must be submitted to the laboratory for analysis without waiting for the manifestations of the disease.
Lyme disease (borelliosis) is the most common tick-borne disease in the Northern Hemisphere. The most characteristic manifestation of the disease is a ring-shaped redness at the site of the bite, which is called erythema vagus. Erythema occurs on average 7-10 days after the bite, although this does not always happen. Even if redness does not appear, a tick bite is a reason to test the tick for Lyme borelliosis without waiting for symptoms of the disease, which on average appear two weeks from the moment of the bite. They include fever, weakness, headache and muscle pain. Sometimes cough, nausea, vomiting and diarrhea appear, and joint pain is often noted. As you can see, they are nonspecific - from the clinical picture it is difficult to understand that this is Lyme disease. Most often, the joints, nervous system and skin are affected as a result. The effectiveness of therapy and the outcome of the disease depend on timely diagnosis: without treatment, it can lead to disability and even death.
The nonspecificity of symptoms is due to the fact that the causative agent of the disease, a spiral-shaped bacterium (spirochete) of the genus Borrelia, affects various tissues and organs. Spirochetes enter the human body with the saliva of a tick during a bite.
You can become infected from May to September, especially likely in places where tick-borne encephalitis is endemic. If the ixodid tick carries pathogens of both diseases, a mixed infection may occur.
Two other diseases transmitted by Ixodid ticks are granulocytic anaplasmosis and monocytic ehrlichiosis. These are bacterial diseases. The causative agent of the first of them, Anaplasma phagocytophilum, affects granulocytes, cells of the immune system. The second disease is caused by bacteria of the genus Ehrlichia, they multiply in monocytes. Hence the names of these diseases. The symptoms of these infections are nonspecific and similar to each other: fever, weakness, headaches. They usually begin to appear within 12 days after the tick bite. In severe cases of the disease, damage to the skin, liver, kidneys, central nervous system, and bone marrow is noted. The infection is severe and has a high mortality rate, especially among immunocompromised people.
Consequences of encephalitis
This disease has a fairly high risk of death. This is a very dangerous disease that needs to be diagnosed promptly and adequately treated. Self-medication of this pathology at home is categorically unacceptable.
Even after recovery, residual neurological symptoms may be present, which include:
- memory loss;
- severe and prolonged headaches;
- loss of coordination, paresis, paralysis;
- mental disorder;
- decreased intelligence;
- constant fatigue, apathy, fatigue.