Ependymomas are rare tumors arising from the ependyma, the membrane lining the inside of the ventricles of the brain and the central canal of the spinal cord. It follows that in the vast majority of cases, ependymomas are located intradurally in the ventricular system and in the spinal cord. Much less often, ependymomas occur outside the ventricular system, directly in the brain. A distinctive feature of these formations is that they are better demarcated from the medulla compared to most other intracerebral tumors. It follows from this that the task of the neurosurgeon is to remove the tumor as radically as possible, both in the case of intracranial localization and when the ependymoma is localized in the spinal cord. If radical removal is not possible, subsequent radiation therapy may be performed.
Ependymomas arise from ependymal cells lining the ventricles of the brain and the central canal of the spinal cord. They can be located along the entire length of the neural tube.
Frequency:
Intracranial location: constitute ≈5-6% of intracranial gliomas, 69% occur in children, accounting for 9% of pediatric brain tumors.
Spinal location: ≈60% of spinal cord gliomas, 96% of cases occur in adults, especially in the region of the filum terminale.
Average age of patients at the time of tumor diagnosis:
Intracranial localization: adults - 17 years old, children - 5 years old.
Infratentorial localization: adults - 14 years, children - 4 years.
Supratentorial localization: adults - 22 years old, children - 6 years old.
Spinal localization: 40 years.
Intramedullary localization: 47 years.
Caudal part: 32 years.
Ependymomas have the ability to spread along the neural tube along the cerebrospinal fluid tract, a process called seeding, which leads to the occurrence of “lost” metastases in 11% of cases. The incidence of metastasis increases as the tumor grade increases. In rare cases, systemic spread occurs.
Causes of brain ependymoma
What serves as a prerequisite for the development of a tumor is unknown, but still there are several factors that can influence the development of pathology:
- heredity;
- long-term use of potent drugs;
- ionizing radiation;
- trauma to the skull or central nervous system;
- oncogenic viral diseases (human papillomavirus, herpes);
- poor environmental conditions;
- smoking and alcohol abuse.
The cancer trigger was initially thought to be the SV40 virus, which was discovered in ependymoma cells. However, subsequent studies did not confirm this theory, so the etymology of the disease is still unknown. As practice shows, cerebral ependymoma most often occurs in children and adolescents, less often in adults.
Pathology
WHO classification:
1. Nonanaplastic (low grade of malignancy)
2. Papillary: “classic lesion” of the GM and SM. Metastasis is possible up to 30%.
3. Myxopapillary ependymoma: a separate form, found only in the area of the filum terminale. Papillary ependymoma with microcystic vacuoles and mucous contents.
4. Subependymoma
5. Anaplastic: pleomorphism, multinucleation, giant cells, mitoses, vascular changes, areas of necrosis (sometimes when anaplastic changes are more pronounced, the term ependymoblastoma is used, but this term should be reserved for a separate type of tumor, rare primitive neuroectodermal tumors in children). Whether the degree of anaplasia influences outcomes is unclear.
Forecast
Prediction is individual for each patient. After all, many factors are taken into account, such as:
- the stage at which the tumor was detected,
- localization and size of the tumor,
- the result of surgical treatment and accompanying therapy,
- the patient's health status and the presence of concomitant diseases.
If the tumor is completely removed, the 5-year survival rate of patients is about 80%.
After partial removal, there is a risk of relapse of the disease. In any case, patients should be regularly monitored by a doctor: these can be annual examinations or consultations as indicated. Relapse occurs most often in the first 5 years after treatment. In some cases, repeated intervention is performed. In addition to secondary cancer, patients who have had tumors in the central nervous system are susceptible to a number of other problems:
- sleep disorders,
- hearing loss,
- deterioration of cognitive functions,
- hormonal imbalance,
- stroke.
Therefore, timely monitoring and diagnosis significantly increase the chance of protecting yourself from complications and difficult treatment. Onco Check-Up allows you to identify violations when they can still be corrected. This diagnosis includes consultations with specialists, necessary diagnostics, and laboratory tests. You only need to spend 4+4 hours on this, but it will help you not worry about your health or identify pathology in time.
Intracranial ependymomas
Key Features:
1. Often occur in the bottom of the fourth ventricle
2. There is a potential threat of spread along the neural tube
3. Young patients have a worse prognosis
4. Treatment: maximum resection followed by radiation therapy.
They are usually well-circumscribed and benign tumors (although malignant ependymomas also occur). They often arise in the floor of the IV ventricle (in 60-70% of cases they are located infratentorially, always near the IV ventricle, they account for 25% of all tumors in the IV ventricle region). Posterior fossa ependymomas in children are often anaplastic and have a greater risk of spreading through the neural tube. Although histologically they do not appear as malignant as medulloblastomas, they have a worse prognosis due to the fact that they tend to grow into the obex, which prevents their complete removal. Subependymomas: they are typically located in the anterior sections of the lateral ventricles or in the posterior part of the IV ventricle, with a pronounced role of subependymal glial cells. They are often detected at autopsies and are subject to surgical treatment in rare cases.
Signs of the disease
When the tumor expands, the following symptoms appear:
- progressive pain in the head;
- feeling of pressure on the eyes;
- nausea and vomiting, independent of food intake;
- irritability, behavioral changes;
- loss of coordination control, unsteadiness of gait;
- violations of fine motor skills (the patient loses the ability to write accurately and quickly);
- decreased level of memorability;
- impairment of auditory (hearing loss) and visual perception (double vision).
With subsequent growth of ependymoma, the cerebrospinal fluid channels may become blocked, hydrocephalus develops, internal pressure increases, and the described symptoms tend to worsen. The pain syndrome increases in intensity and is not relieved even by strong analgesics; vomiting does not stop and does not bring relief. Systematic seizures are often found in the pediatric clinical picture.
Diagnostics
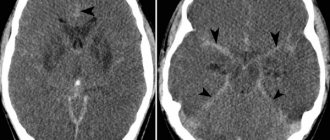
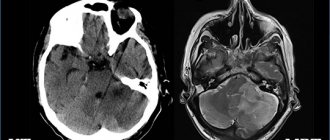
CT/MRI:
Typically, a mass is found in the floor of the fourth ventricle, often with occlusive hydrocephalus.
Radiologically it may be difficult to differentiate from medulloblastoma, but the following signs may help:
1. Calcifications are common in ependymomas, but rare (<10%) in medulloblastomas
2. Medulloblastomas usually arise from the roof of the IV ventricle (from its apex, fastigium), which covers the tumor (“banana sign”), ependymomas tend to grow into the IV ventricle from the bottom
3. Ependymomas have a non-homogeneous structure on MRI in T1 mode
4. The exophytic component in ependymomas tends to show a high signal on T2 MRI (in medulloblastomas it is only slightly hyperintense)
Myelography
Myelography with water-soluble contrast agent has the same sensitivity for detecting metastases as MRI with gadolinium. It is also possible to do a cytological examination of the cerebrospinal fluid to determine the stage of the tumor.
Symptoms
Unlike other types of brain tumors, ependymoma is rare. Cancer cells can have different levels of malignancy. Some tumors grow slowly, while others grow quickly, compressing surrounding vessels and tissues, causing characteristic symptoms.
Clinical signs of ependymoma directly depend on the location and size of the formation. As with other types of cancer, in the early stages it does not cause obvious symptoms and only as the tumor grows do the symptoms become more noticeable and, in some cases, severe.
The main signs of the disease are blurred vision and hearing, convulsions, difficulty swallowing and speech impairment, which are manifested as a result of increased intracranial pressure. Other characteristic symptoms include:
- headache of a bursting or aching nature;
- dizziness;
- impaired coordination of movements;
- unsteady gait;
- tremor of the limbs;
- chronic fatigue;
- a sharp decrease in body weight;
- nausea, urge to vomit;
- memory loss;
- sudden change of mood;
- “floaters” or “fog” before the eyes;
- convulsions, numbness of extremities;
- difficulty swallowing.
Symptoms depend on where the formation is located. If the tumor is located in the cerebellum, balance and gait will be affected. Its location in the cerebrum causes seizures. The presence of a formation in the spinal cord - numbness of the face, disturbances in the functioning of the digestive system. The exact location of cancer can only be recognized with the help of comprehensive diagnostics, which is prescribed by a doctor if an oncological process is suspected.
Treatment
Surgical resection
The purpose of the operation: maximum removal of the intracranial part of the tumor without neurological deficit. If there is significant tumor invasion into the bottom of the fourth ventricle, then it is completely impossible to remove it. After surgery, radiation therapy and myelography are performed to exclude possible metastasis. 10 ml of cerebrospinal fluid is sent for cytological examination to determine the number of malignant cells (if any) and can also be used as a way to monitor the effectiveness of treatment.
Radiation therapy
Ependymomas are second in radiosensitivity after medulloblastomas. Radiation therapy is prescribed after surgical removal of the tumor (survival improves after radiation therapy in the postoperative period: survival of 50% of patients was 2 years longer with radiation therapy than without it, while the number of patients who had a 5-year survival period increases from 20 -40% to 40-80%)
Specific treatment of ependymoma depending on stage
A personal treatment regimen is developed for each patient. Methods are selected taking into account a number of factors, the leading among which is the stage of the tumor.
The most effective way to combat ependymoma is surgery, during which the tumor tissue is completely removed. As a result, the cerebrospinal fluid begins to circulate normally, the pressure returns to normal, and the chances of a full recovery significantly increase.
If the tumor is large and cannot be removed surgically, then other, equally effective methods of treatment are prescribed. An alternative to surgery is stereotactic radiosurgery - the tumor is removed using a modern CyberKnife device. This technique is especially effective in the treatment of subependymoma and myxopapillary ependymoma.
For tumors located in hard-to-reach places, radiation therapy is carried out with precise impact on the affected area. Healthy tissues are not affected by this method of treatment. Radiation therapy is also included in the complex therapy program and is prescribed in the postoperative period. When metastases are detected in the spinal cord and in the ventricular system of the brain, the affected areas are also irradiated.
Ependymomas are practically insensitive to chemotherapy, so cytostatic drugs are prescribed in rare cases to reduce the size of the tumor in later stages.
High treatment effectiveness and minimal health risks are the main goals pursued by Israeli oncologists, which is why thousands of patients from different countries turn to them. Clinics in Germany, Switzerland, and the USA also provide effective treatment, but the cost of cancer treatment abroad in this case will be 20-40% higher than in Israel.
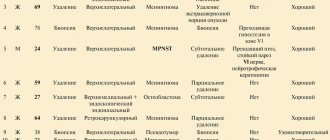
A comment
The article contains a description of two clinical observations and a literature review on rare cases of the formation of intra-extramedullary ependymomas. Such observations should indeed be recognized as exclusive, although in our practice there are observations of this kind. Despite the limited number of described cases, it is noted that ependymomas with intra-extramedullary growth occur predominantly in young men (25-40 years old) and, based on the description of clinical observations, as well as based on our own experience, we can say that such formations are always are on the border of benign and anaplastic neoplasms - GradeII-GradeIII. In particular, we observed the development of anaplasia in the tumor, followed by a rapid relapse - postoperative observation for a year did not reveal continued growth, and in the next 3 months, rapid development of the tumor with pronounced compression of the spinal cord was detected, which required emergency intervention.
These patterns, described in the article in the form of characteristics of Ki-67, indicate the initial tendency of intra-extramedullary ependymomas to anaplasia, which requires correction of postoperative tactics with possible radiation therapy. This work is useful and noticeable in a series of publications devoted to rare neurosurgical pathologies.
A.O. Guscha (Moscow)