Varieties, reasons
Brain edema occurs:
- vasogenic;
- cytotoxic;
- interstitial;
- osmotic.
The signs of cerebral edema depend on the type of developing pathology.
Causes of disease progression:
- Vasogenic edema occurs due to increased cerebral vascular permeability.
- Cytotoxic is the “swelling” of brain cells due to an increase in the amount of fluid inside them.
- Interstitial edema develops when there is increased pressure of the cerebrospinal fluid in the ventricles of the brain.
- Osmotic edema - with an increase in the osmolarity of brain tissue.
The most common reasons that cause brain swelling are: brain injury and disruption of its tissues in various pathologies.
Brain edema most often occurs in the following pathological conditions of a traumatic nature:
- brain contusion;
- fracture of the base of the skull;
- intracerebral hematoma;
- subdural hematoma. The prognosis of surgery for cerebral edema depends on its size.
The described pathology develops against the background of such organic brain lesions:
- ischemic and hemorrhagic stroke;
- hemorrhage under the arachnoid membrane;
- tumors;
- infectious diseases - encephalitis (inflammation of brain tissue) and meningitis (inflammation of the meninges).
Extracranial causes of cerebral edema can result from:
- Quincke's edema is a severe allergic reaction of the body;
- infectious diseases - scarlet fever, measles, mumps;
- diabetes;
- liver failure;
- alcoholism.
On our website Dobrobut.com you will find more information about the causes of cerebral edema in a newborn child, the development of pathology in the elderly and other facts.
Causes of cerebral edema in children
Brain edema occurs with traumatic brain injury (TBI), intracranial hemorrhage, cerebral embolism, and brain tumors. In addition, various diseases and pathological conditions leading to cerebral hypoxia, acidosis, disturbances of cerebral blood flow and liquor dynamics, changes in colloid-osmotic and hydrostatic pressure and acid-base status can also lead to the development of AMS.
The occurrence of cerebral edema
There are 4 main mechanisms in the pathogenesis of cerebral edema:
1.
Cytotoxic.
It is a consequence of the effects of toxins on brain cells, resulting in a disorder of cellular metabolism and disruption of ion transport through cell membranes. The process is expressed in the cell losing mainly potassium and replacing it with sodium from the extracellular space. Under hypoxic conditions, pyruvic acid is reduced to lactic acid, which causes a disruption of the enzyme systems responsible for removing sodium from the cell - a blockade of sodium pumps develops. A brain cell containing an increased amount of sodium begins to intensively accumulate water. A lactate content above 6-8 mmol/l in the blood flowing from the brain indicates brain edema. The cytotoxic form of edema is always generalized, spreading to all parts, including the stem, so signs of herniation may develop quite quickly (within several hours). Occurs in cases of poisoning, intoxication, ischemia.
2.
Vasogenic.
It develops as a result of damage to brain tissue with disruption of the blood-brain barrier (BBB). This mechanism for the development of cerebral edema is based on the following pathophysiological mechanisms: increased capillary permeability; increase in hydrostatic pressure in capillaries; accumulation of fluid in the interstitial space. Changes in the permeability of brain capillaries occur as a result of damage to endothelial cell membranes. Violation of the integrity of the endothelium is primary, due to direct injury, or secondary, due to the action of biologically active substances such as bradykinin, histamine, arachidonic acid derivatives, hydroxyl radicals containing free oxygen. When the vessel wall is damaged, blood plasma, along with the electrolytes and proteins it contains, moves from the vascular bed to the perivascular areas of the brain. Plasmorrhagia, increasing oncotic pressure outside the vessel, helps to increase the hydrophilicity of the brain. Most often observed with head injury, intracranial hemorrhage, etc.
3.
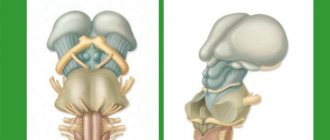
Hydrostatic.
It manifests itself when the volume of brain tissue changes and the ratio of blood inflow and outflow is disturbed. Due to the difficulty of venous outflow, hydrostatic pressure increases at the level of the venous knee of the vascular system. In most cases, the cause is compression of large venous trunks by a developing tumor.
4.
Osmotic.
It is formed when there is a disruption of the normally existing small osmotic gradient between the osmolarity of the brain tissue (it is higher) and the osmolarity of the blood. Develops as a result of water intoxication of the central nervous system due to hyperosmolarity of brain tissue. Occurs in metabolic encephalopathies (renal and liver failure, hyperglycemia, etc.).
Signs of cerebral edema
Symptoms depend on how quickly brain swelling develops.
Signs of acute cerebral edema:
- disturbance of consciousness - from slight stupor to a state of coma with cerebral edema;
- convulsions – occur as swelling progresses;
- muscle atony – develops after seizures;
- membrane symptoms.
Gradual increase in edema – additional symptoms of cerebral edema in adults:
- headache;
- nausea and vomiting that does not bring relief;
- movement disorders;
- visual and speech disorders;
- hallucinatory syndrome.
Signs indicating critical development of the condition:
- paradoxical breathing (deep breaths with long gaps between them);
- a sharp decrease in blood pressure;
- unstable pulse;
- increase in body temperature above 40 degrees Celsius.
The appearance of such signs indicates compression of the brain stem, which leads to death.
What types of brain tumors are common in children and what are the characteristics of these tumors?
First of all, it should be noted that most cancers that develop in adults can also occur in children. However, there are specific tumors that are considered more common at a young age:
- Medulloblastoma : Considered by many to be the most common type of brain tumor that develops in children, it is estimated to account for approximately 20% of the total number of these tumors. The tumor originates in embryonic cells that have not had time to undergo differentiation during the development of the fetus in the womb, and, therefore, such a tumor is considered embryonic. This tumor typically occurs in the back of the brain (also called the posterior fossa) and tends to grow relatively quickly
- PNET - primitive neuroectodermal tumor - a tumor very similar in its characteristics to medulloblastoma and also develops from embryonic cells. PNET is typically found in the medullary region (in contrast to medulloblastoma) and is generally considered a high-grade tumor.
- Germ cell tumor of the brain : This tumor also originates in germ cells that form already in the very early stages of pregnancy. Such tumors usually develop in the area of the pineal gland or near the sella turcica, located at the base of the brain. They are common mainly in children and young adults
- Gliomas: Tumors that develop from glial cells (which line nerve fibers and the spinal cord) are also relatively common in children. They can develop in various parts of the body, for example, on the optic nerve or in the ventricles of the brain themselves. The most common types of gliomas in children are astrocytoma and ependymoma.
To date, the true cause of the development of brain tumors in children is unknown. Most cases of brain cancer occur in children under 10 years of age, however, as mentioned above, we are talking about a fairly rare disease, developing in three out of 100 thousand children.
What symptoms may indicate the development of brain cancer in a child?
This is the most important question in this context due to the great difficulties in diagnosing the disease in children, especially very young ones. In the first years of life, children are understandably not fully in touch with their environment, and therefore cannot accurately tell others how they are feeling. This is where you, parents, come in: recognizing changes in your child's behavior and taking any complaints seriously can make all the difference in such cases.
The main symptoms that may indicate the development of a brain tumor in children:
- Headaches that occur mainly at night and in the early morning and get better during the day (sometimes the pain is so severe that the child wakes up in the middle of the night)
- Headache that gets worse with exercise, sneezing or coughing
- Head tilt to the side
- Long-lasting pain in the back of the head
- Vomiting in the morning
- Severe fatigue and weakness
- Changes in behavior (eg, lethargy)
- Seizures.
There are two important things to point out here: first, sometimes only some of the symptoms appear and not all of them. Secondly, these symptoms are also typical for diseases other than brain cancer, so it is important not to rush to unnecessary conclusions. It is important to immediately conduct diagnostic tests for your child and wait for the doctor’s response.
Diagnostics
Cerebral edema should be suspected if impairment of consciousness increases, meningeal symptoms are observed, and the patient's condition worsens.
Instrumental methods that are used to confirm the diagnosis of cerebral edema:
- computed tomography (CT);
- magnetic resonance imaging (MRI). This is an important diagnostic method - you can detect swelling of the spinal cord on MRI, and not just the brain.
Of the laboratory research methods, general and biochemical blood tests are important.
It is dangerous to perform a lumbar puncture for diagnostic purposes - displacement of brain structures and jamming of the brain stem in the occipital foramen of the skull may occur.
Symptoms of a brain tumor in children
The limited internal space of the skull is reserved only for the brain and there is no room for anything else. Therefore, as brain tumors grow in children, excess intracranial pressure is created in the skull. This pressure can also be created by obstructing the flow of cerebrospinal fluid in the brain.
Associated symptoms include:
- Headache;
- Seizures;
- Nausea and vomiting;
- Irritability;
- Lethargy and drowsiness;
- Changes in the patient’s character and mental activity;
- Macrocephaly (increase in head volume) in children whose skull bones have not yet fully fused;
- Coma and death if untreated.
Other symptoms may also appear, for example, with a tumor in the cerebellum, children may experience difficulty moving, walking, and coordinating. When a tumor arises near the optical pathways, visual changes may occur.
Treatment of cerebral edema
The main principles of treatment for cerebral edema are:
- dehydration;
- improvement of metabolic processes in the brain;
- etiotropic treatment;
- symptomatic therapy.
What consequences of cerebral edema during stroke and other pathologies will accompany the patient depends on the timeliness and competence of the therapy.
Dehydration therapy
Its purpose is to remove excess fluid from brain tissue. Based on the appointments:
- osmotic diuretics (diuretics);
- magnesium sulfate and glucose solution - they enhance the effect of diuretics and also improve brain nutrition;
- L-lysine escinate - the drug is not a diuretic, but removes fluid.
Improving brain processes
For this purpose the following are appointed:
- metabolic drugs;
- glucocorticosteroids;
- oxygen therapy.
Etiotropic therapy
When treating cerebral edema, it is necessary to eliminate the causes of the development of the pathology and “destroy” the mechanism of edema formation. Destination:
- antibiotics;
- removal of tumors and hematomas;
- shunt operations, after which cerebral blood supply improves
This treatment is carried out after the patient’s condition has stabilized.
Symptomatic therapy
It is aimed at eliminating cramps, vomiting, pain, and so on. In addition to conservative therapy, surgical treatment can be used:
- decompression craniotomy;
- Ventricular drainage.
Recommendations from the neurocritical care society for the treatment of cerebral edema (2020).
Recommendations from the neurocritical care society for the treatment of cerebral edema (2020).
Cerebral edema is a nonspecific pathological edema that can result from any focal/diffuse cerebral damage. The simplest description is the accumulation of excess fluid in brain cells and/or extracellular space. Cerebral edema may be secondary to disruption of the blood-brain barrier, local inflammation, vascular lesions, or changes in cellular metabolism. Identification and treatment of cerebral edema is central to the management of critical intracranial pathology.
Treatment of cerebral edema in patients with subarachnoid hemorrhage (SAH).
Recommendations
1. We suggest using a bolus of hypertonic sodium saline (HSS) based on symptoms rather than a sodium target for the treatment of intracranial hypertension (ICH) or cerebral edema in patients with SAH (conditional recommendation, very low-quality evidence).
2. Due to insufficient evidence, we cannot recommend a specific dosing strategy for GRN to improve neurological outcomes in patients with SAH.
Treatment of cerebral edema in patients with traumatic brain injury.
Recommendations
1. We suggest the use of GRN over mannitol for the initial treatment of ICH or cerebral edema in patients with TBI (conditional recommendation, low-quality evidence).
2. We believe that the use of mannitol is an effective alternative for patients with TBI who cannot be prescribed GRN* (conditional recommendation, low-quality evidence). *Especially in cases of hypernatremia and volume overload.
3. In patients with TBI, we do not recommend the use of prehospital GRN to improve neurological outcomes (strong recommendation, moderate-quality evidence) and mannitol (conditional recommendation, very low-quality evidence).
The decision about which drug to use should be based on available resources, individual characteristics and local practice.
Treatment of cerebral edema in patients with acute ischemic stroke.
Recommendations
1. We suggest using GRN or mannitol for the initial treatment of ICH or cerebral edema in patients with acute ischemic stroke (conditional recommendation, low-quality evidence).
2. We suggest that clinicians consider using GRN to treat ICH or cerebral edema in patients with acute ischemic stroke who do not respond adequately to mannitol (conditional recommendation, low-quality evidence).
3. We do not recommend the use of prophylactic routine mannitol for acute ischemic stroke due to the potential for harm (conditional recommendation, low-quality evidence).
Treatment of cerebral edema in patients with intracerebral hemorrhage (ICH).
Recommendations
1. We suggest the use of GRN over mannitol for the initial treatment of ICH or cerebral edema in patients with ICH (conditional recommendation, very low-quality evidence).
2. We suggest bolus GRN based on symptoms or sodium target* for the treatment of ICH or cerebral edema in patients with ICH (conditional recommendation, very low-quality evidence). *target sodium level is 145–155 mmol/L.
3. We do not recommend the use of corticosteroids to improve neurological outcome in patients with ICH due to the potential for increased mortality and infectious complications (strong recommendation, moderate-quality evidence).
Treatment of cerebral edema in patients with bacterial meningitis.
Recommendations
1. We recommend dexamethasone 10 mg IV every 6 hours for 4 days to reduce neurological sequelae (primarily hearing loss) in patients with community-acquired bacterial meningitis (strong recommendation, moderate-quality evidence).
2. We suggest dexamethasone 0.15 mg/kg IV every 6 hours for 4 days as an alternative dose for patients with low body weight or a high risk of side effects from corticosteroids (Good Clinical Practice Statement).
3. We recommend administering dexamethasone before or with the first dose of antibiotic in patients with bacterial meningitis (strong recommendation, moderate-quality evidence).
4. We recommend the use of corticosteroids to reduce mortality in patients with tuberculous meningitis (strong recommendation, moderate-quality evidence).
5. We suggest treatment with corticosteroids for two or more weeks in patients with tuberculous meningitis (conditional recommendation, low-quality evidence).
6. There is insufficient evidence to determine whether GRN or mannitol is more effective in reducing ICH or cerebral edema in patients with community-acquired bacterial meningitis.
Treatment of cerebral edema in patients with hepatic encephalopathy.
Recommendations
1. We suggest using GRN or mannitol for the treatment of ICH or cerebral edema in patients with hepatic encephalopathy (conditional recommendation, very low-quality evidence).
2. There is insufficient evidence to determine whether hyperosmolar therapy or ammonia-lowering therapy improves neurological outcomes in patients with hepatic encephalopathy.
Recommendations for assessing the risk of acute kidney injury (AKI) after use of mannitol and GRN.
1. We suggest using the osmolar gap instead of the serum osmolarity threshold during mannitol treatment to control the risk of AKI (conditional recommendation, very low-quality evidence).
2. Renal function tests should be closely monitored in patients receiving mannitol or GRN due to the risk of AKI with hyperosmolar therapy (Good Clinical Practice Statement).
3. We suggest that severe hypernatremia and hyperchloremia* should be avoided during treatment for GRN due to their association with AKI (conditional recommendation, low-quality evidence). *upper limit of sodium 155–160 mEq/L and serum chloride 110–115 mEq/L may be reasonable to reduce the risk of AKI (conditional recommendation, very low-quality evidence).
Therefore, clinicians should closely monitor renal function, electrolytes, and acid-base balance when using hyperosmolar therapy.
Recommendations for the optimal method of GRN administration
1. There is insufficient evidence to support the use of continuous infusion of GRN directed at a target serum sodium level to improve neurological outcomes.
2. Due to insufficient evidence, we cannot recommend specific dosing strategies for GRN to improve neurological outcomes in patients with cerebral edema.
3. Clinicians should avoid hyponatremia in patients with severe neurological damage due to the risk of exacerbation of cerebral edema (Good Clinical Practice Statement).
Non-drug treatment of cerebral edema and ICH
Recommendations
1. We suggest raising the head of the bed 30 degrees (no more than 45 degrees) as a useful adjunct for reducing intracranial pressure (conditional recommendation, very low-quality evidence).
2. We recommend brief episodes of hyperventilation for patients with acute ICH (strong recommendation, very low-quality evidence).
3. We suggest that CSF drainage be considered as a useful adjunct for reducing ICH (conditional recommendation, very low-quality evidence).
Other nonpharmacologic treatments such as surgical decompression and therapeutic hypothermia were not included in the recommendations because they are adequately discussed in other guidelines.
Source citation: Cook AM, Morgan Jones G, Hawryluk GWJ, et al. Guidelines for the Acute Treatment of Cerebral Edema in Neurocritical Care Patients. Neurocrit Care. 2020; 32(3): 647–666.doi: 10.1007/s12028–020–00959–7
Diagnosis of brain tumors
Children who exhibit symptoms consistent with a brain tumor should be carefully examined by a pediatrician or pediatric neurologist to find the cause of the problems.
The examination usually includes a magnetic resonance scan of the brain and if it shows the presence of a tumor, the patient is sent to a consultation with a pediatric neurosurgeon, whose task is to develop, together with the child’s parents, the most effective treatment method.
Other specialists may also be involved for consultations:
- Pediatric oncologists;
- Ophthalmologists;
- Doctors who specialize in epilepsy (to treat seizures);
- Radiologists;
- Specialists in functional diagnostics.
To develop the right treatment plan for a child with a brain tumor, the surgical team needs information about:
Tumor location
This can be determined using computed tomography or magnetic resonance imaging. Such information is necessary because There are areas of the brain where surgery is impossible. The scan allows you to evaluate the possibility of surgical treatment.
Tumor type
To do this, sections of tumor tissue are examined under a microscope. Not knowing this information allows you to assess how the tumor will develop and spread.
Tumor class
The higher the class, the more aggressive the tumor will behave and spread at a faster rate.