Arachnoid cyst: nature of the pathology
An arachnoid cyst is a lesion of the brain in the form of a neoplasm in its membranes, filled with cerebrospinal fluid (medically defined as cerebrospinal fluid). Localization in the shell of the same name gave the name to the disease. The arachnoid membrane at the site of pathology bifurcates and cerebrospinal fluid accumulates between its walls. Basically, these are small-volume cysts, but there is a possibility of an increase in cerebrospinal fluid, which can lead to compression (pressure) on the area of the underlying cortex and the appearance of clinical symptoms.
The formation can be located in different areas of the arachnoid membrane:
- cerebellar angle;
- Sylvian fissure;
- suprassellar (on top) of the sella turcica.
According to medical forecasts, approximately 4% of humanity are carriers of arachnoid cysts, and the majority of them are men.
Causes of cysts
The cyst can be congenital or result from previous diseases.
- The walls of a congenital (primary) cyst consist of cells of the arachnoid membrane, which secrete cerebrospinal fluid. It forms before the birth of the child, as a rule, does not cause any symptoms and turns out to be an accidental finding when an MRI to identify other diseases shows a picture of arachnoid changes of a liquor cystic nature.
- A secondary cyst can have various causes: previous meningitis, brain surgery, inflammatory and autoimmune diseases. Such a cyst may also not manifest itself for a long time; the first symptoms may appear only several years after its occurrence. The walls of such a cyst consist of scar tissue.
Classification by etiology
For reasons of occurrence, the lesion may be:
- Primary (congenital) - as a result of brain abnormalities during formation and development.
- Secondary (acquired) - due to trauma, inflammation, bleeding of the meninges.
According to morphology, arachnoid cysts are divided into two categories:
- simple - brain membrane cells line the internal cavity of the cyst and produce cerebrospinal fluid;
- complex - the structural tissue of the cyst contains cells of other elements (for example, glial).
For practical neurology, the morphological type of pathology is unimportant, while the etiological origin requires mandatory consideration in the diagnostic process.
According to clinical manifestation, arachnoid cysts are classified into two types:
- progressive - with an increase in the volume of formation and severity of symptoms;
- frozen - with preservation of the latent state and size of the cyst.
Accurate determination of the type of cyst according to classification criteria is of utmost importance when prescribing therapeutic tactics.
Causes of formation of cystic brain lesions
The causes of congenital pathology are caused by a violation of intrauterine brain formation, which is caused by:
- infectious diseases (herpes, toxoplasmosis, etc.);
- intoxication intrauterine exposure (against the background of professional characteristics, smoking, taking drugs, alcohol, teratogens, radiation);
- thermal effects (abuse of baths, saunas, solariums, hot baths, etc.);
- the presence of Morphan syndrome, hypogenesis.
Causes of acquired cyst of the arachnoid intracranial membrane:
- TBI (concussions, bruises);
- consequence of neurosurgical intervention;
- infections (meningococcal, meningoencephalitis, arachnoiditis, etc.);
- hemorrhages, meningeal hematomas.
An arachnoid cyst can also become a consequence of hyperformation of the spinal substance and its accumulation in the membrane.
Mental disorders in brain tumors
Brain tumors account for about 6% of organic diseases of the central nervous system. Found in 0.1–5% of patients in psychiatric hospitals. Slightly more common in men. About half of primary tumors are gliomas. In addition, in children, medulloblastomas, astrocytomas, and plexuspapillomas are more often found, and in the elderly, meningiomas, glioblastomas, pituitary adenomas, and acoustic neuromas are more often found. Mental disorders are detected in 25–100% of patients with brain tumors. Sometimes these disorders are the first and for a long time the only symptom complex, especially if the tumor is characterized by slow growth; mental disorders in brain tumors are very diverse. It happens that with tumors of the same localization, different mental disorders develop, and with tumors of different localizations. There are transient and persistent mental disorders, as well as acute postoperative psychoses.
| | Often, symptoms of various mental disorders, such as schizophrenia, also appear with brain tumors. That is why comprehensive diagnostics is necessary to make a diagnosis. |
1. Transient mental disorders
1. Epileptic seizures. Astrocytomas and oligodendrogliomas of frontotemporal localization cause seizures in 90% of patients. Supratentorial slow-growing tumors are accompanied by seizures in more than 40% of cases. Seizures occur much less frequently (4%) with subtentorial tumors. In the structure of seizures, mental, motor and other disorders are not uncommon, which may indicate the topic of the tumor.
2. Hallucinations are observed in the structure of the aura or as part of a partial seizure. Olfactory deceptions are especially often observed with damage to the right temporal region. Usually combined with other disorders, including hallucinations of a different modality. Somewhat later, gustatory deceptions join the olfactory ones. Musical and rhythmic hallucinations are usually characteristic of patients with tumors of the right temporal region; imaginary sounds are heard on the left. Rhythmic auditory deceptions are, for example, the noise of the surf, a running motor, pouring water, the sounds of a bird chirping, repeated calls, etc. With tumors on the left, verbal deceptions of various contents are observed; more often they are combined with anxiety, transient aphasia, memory and thinking disorders. Optical illusions are less common than those mentioned. With tumors on the right, these are elementary hallucinations: dots, flashes of light, sparks, ripples, etc. Photopsia can be accompanied by musical deceptions. With tumors on the left, complex visions are observed - objects, people (often moving); there may be visions “inside the head... eyes”, visions “in the thoughts”. Tactile deceptions are rare and occur with tumors of the right hemisphere. Such deceptions also occur with sleep paralysis. Imaginary sensations related to the sexual sphere are frequent.
3. Affective disorders. With tumors of the right hemisphere, attacks with various disturbances are observed, but with the affects of melancholy and horror in the foreground. Attacks with positive affects also occur. With tumors on the left, anxiety and rage may predominate during an attack.
4. The phenomena of depersonalization and derealization. Characteristic for tumors of the right temporo-parietal-occipital region. At the same time, metamorphopsia and disturbances in the perception of time may occur, and very peculiar phenomena occur. For example, the patient feels that “time is going down.” Relatively rare symptoms such as echonesia, palinopsia (“visual perseveration”, when some visual image is exactly repeated several times in a row) or ignoring the space on the left are also observed.
5. Speech phenomena. Presented with attacks of speech loss. They are especially often observed in tumors of the left hemisphere. These may be attacks of motor aphasia, when instead of verbalizing the patient “moos” or utters other inarticulate sounds; the disorder may indicate a tumor of the left frontal lobe. With tumors in the left temporal region, attacks of sensory aphasia occur, i.e., misunderstanding of speech, the patient hears some kind of incomprehensible noise instead of the speech of others. He may react to the sound of speech and say several incoherent phrases. With a tumor of the temporo-parieto-occipital region on the left, the patient may suddenly lose the ability to select the right words - this is an attack of amnestic aphasia.
6. Disorders of thinking and memory occur with tumors of the left temporo-parietal-occipital region; thinking disturbances are represented by attacks of blockage of thinking (sperrung) and an influx of thoughts (mentism). Mnestic attacks occur both in the form of a “memory lapse” for various information, and in the form of a violent influx of memories of something from the past. There are also attacks during which there is an acute need to remember something, but the patient does not know what exactly.
7. Impaired consciousness and epileptiform states, in particular paroxysms of impaired clarity of consciousness: “fainting,” episodes of obnibulation, somnolence. They probably occur more often with subtentorial tumors. These are also episodes of reduplication (states “with two-track experiences” - Dobrokhotova, 1999). The patient freezes in one position and does not make contact. Without disconnecting from reality, in a few seconds he seems to relive certain situations of his past. Usually these are real, sometimes forgotten situations that seem to last for days and even weeks, compressed into such a small period of time. At the same time, there is a doubling of self-perception: the patient feels what he was like a long time ago and how he realizes his Self now. In such states, only the right side of real space can be realized. Sometimes ecmnestic attacks occur when, completely disconnected from reality, the patient feels himself somewhere in the distant past, living it again. It is possible that patients can sometimes be “transported” to a virtual situation (“memory hallucination” - M.B. Krol, 1936). Such episodes are characteristic of tumors of the right hemisphere. With tumors in the depths of the right hemisphere, near the 3rd ventricle, in the sellar-chiasmatic region, oneiric episodes may occur, often with partial congenital amnesia. Tumors of the left frontotemporal region reveal themselves as absence seizures, psychomotor seizures, and twilight states of consciousness. In terms of brain tumors, postictal confusion should also be a concern.
2. Persistent mental disorders
Productive disorders may be more common in tumors of the temporal and chiasmal-sellar regions, while deficient disorders occur in the frontal, especially convexity, regions of the brain.
1. Sleep and dream disorders. There may be changes in the sleep-wake cycle, increased frequency, decreased frequency of dreams, and nightmares. The feeling of sleep is lost, the boundary between dreams and reality is erased.
2. Memory impairment. In severe cases, Korsakov's syndrome develops, including retrograde amnesia. The disorder is usually combined with paresis and loss of sensitivity on the left, less often with left-sided spatial agnosia. A decrease in symbolic memory is observed with a tumor in the left hemisphere.
3. Affective disorders. Hypothymic states, melancholy depression, and bipolar mood disorders occur in right-hemisphere tumors. With tumors on the left, anxious depression and loss of emotions (combined with lack of spontaneity) are possible. Euphoria as part of the pseudoparalytic syndrome and mori-like states often occurs with frontobasal tumors; At the same time, disturbances of smell, vision (up to blindness unconscious to patients), and hemiparesis can be detected. Euphoria in the structure of Korsakov's syndrome is observed with tumors in the region of the 3rd ventricle. Significant emotional depression, anosognosia and left-sided spatial agnosia develop with tumors of the posterior parts of the right hemisphere and in the region of the 3rd ventricle. At the same time, there may be left-sided hemiparesis with hypoesthesia and hemianopia on the left; the gaze is directed to the right. Similar violations occur after operations to remove tumors of the specified localization.
4. Long-term disturbances of consciousness. Usually these are states of stunned consciousness of varying degrees. May occur in patients with rapidly growing tumors, as well as brain tumors in elderly patients.
3. Acute postoperative psychoses
They appear on the 2nd–3rd day after surgery and can last for several weeks. One of the causes of psychosis is cerebral edema. After removal of tumors of the frontotemporal region on the left, as well as neuritis of the 8th cranial nerve, hallucinatory-delusional psychoses are observed. After intervention in the posterior parts of the right hemisphere, near the 3rd ventricle, in the chiasmatic-sellar region, oneiric states, Korsakoff syndrome with euphoria and confabulations may occur. A state of akinetic mutism with congealing has been described in tumors of the 3rd ventricle (epidermoid cyst). Psychoses with severe euphoria, motor restlessness, disinhibition and foolishness, as well as euphoria and dyspraxia, when one hand did the opposite of the other, have been described. Age-related features of mental disorders in brain tumors are described. Thus, children with “dysontogenetic” tumors (for example, with craniopharyngioma) under the age of 5–10 years may have symptoms of progeria (these are children of the “little old men” type). As they grow older, stunted growth, sexual development, a tendency to be overweight, weakness, fatigue, and thirst become more and more noticeable. In grades 6–7, they compare academically with their peers, and then begin to lag behind them. In adulthood, they are characterized by lethargy, conservatism, and decreased creativity.
In older people, brain tumors are often not detected during life. In psychiatric hospitals, such patients are often considered as vascular patients, especially since every seventh of them has apoplectiform disorders. Focal paroxysmal phenomena are relatively rare; often after a single paroxysm, paresis and paralysis develop. Metastatic tumors of the frontal and frontotemporal region on the left predominate, causing dementia similar to Pick's and Alzheimer's diseases.
In all cases where patients experience paroxysmal headaches, congestion in the fundus, paroxysmal disorders, increasing psychoorganic decline and progressive neurological symptoms, a thorough examination is necessary in order to eliminate doubts about the volumetric process. Tumor failure still occurs on average in almost half of patients, especially the elderly.
Back to contents
Symptoms of arachnoid cystic formations
Most often, the cyst is insignificant in volume and does not show clinical signs. Congenital pathology can be discovered completely by accident during diagnostic procedures (MRI, neurosonography) for other intracranial abnormalities. Initial symptoms may appear due to disorders of the blood vessels of the brain, trauma or infections.
The growing cerebrospinal fluid provokes an increase in the size of the cyst, and the symptoms become pronounced:
- increased pressure inside the skull;
- cephalalgia (headache);
- feeling of a “heavy” head (dizziness, noise and pounding (pulsation) in the ears and skull).
The growing volume of cystic formation provokes an increase in the intensity of permanent symptoms:
- nausea and vomiting;
- increased fundus pressure;
- bifurcation and spots of visual fields;
- hemiparesis (muscle weakness);
- dysarthia;
- numbness of the arms and/or legs;
- convulsions;
- fainting.
Sometimes the patient experiences hallucinations. Children experience mental retardation (mental retardation).
The consequence of a growing arachnoid cyst can be brain degeneration, rupture of the formation, and death.
Symptoms of the disease
If an arachnoid cyst causes any neurological symptoms, they depend on its location. They are due to the fact that a large cyst exerts mechanical pressure on the areas of the brain located next to it.
- Most often it is located in the middle cranial fossa, and the damage to the midbrain caused by it manifests itself in hearing and vision impairment, hallucinations, severe headaches, dizziness and nausea. In more severe cases, coordination disorders, paralysis, paresis and hemiparesis, seizures and mental impairment are possible.
- Pathology in the posterior cranial fossa, if it is located in the brainstem area, causes increased pressure in the spinal canal and inside the skull, which causes intervertebral hernias and secondary hydrocephalus. It can also cause disturbances in the functioning of the digestive, cardiovascular and respiratory systems, and disturbances in thermoregulation. In the cerebellar area, it causes disturbances in gait, coordination, involuntary eye trembling (nystagmus), and decreased muscle tone.
- In the temporal region, pathology, as a rule, does not produce any symptoms. If it manifests itself, then rare hearing and coordination disorders may occur, and disturbances in oral and written speech may occur.
- If it is located in the anterior cranial fossa, then so-called frontal symptoms occur - a decrease in the level of intelligence, motivation, emotional impoverishment, slurred speech. One of the brightest markers of damage to the frontal region is characteristically elongated lips in the shape of a tube.
Regardless of the location, the pathology can cause increased intracranial pressure, headaches, dizziness, loss of coordination, increased fatigue and drowsiness, and the possible development of epileptic syndrome.
Diagnostics
An arachnoid cyst does not have a specific picture; its clinical picture is characteristic of many pathologies associated with brain formations of different etiologies. Diagnostic methods include:
- appointment with a neurologist;
- neurological diagnostics (rheo-, echo-, electroencephalogram);
- Magnetic resonance imaging;
- SCT (CT - computer scan).
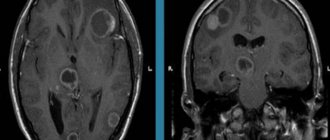
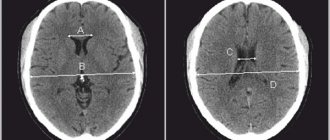
MRI with contrast gives the most complete picture and helps to distinguish a cyst from tumor-like pathologies.
Diagnostic methods
It is impossible to diagnose an arachnoid cyst based on symptoms alone.
The main method of diagnosing it is MRI. In the photographs, arachnoid changes of a liquorocystic nature appear as dark-colored formations, with clearly defined contours, most often round in shape.
Studies are also prescribed to identify signs of impaired blood supply to the brain, infectious or autoimmune diseases. Neurological diagnostics are carried out to identify the depth of neurological disorders.
Treatment
Therapeutic treatment of frozen cysts with no clinical signs is not carried out. The patient is registered with a neurologist and undergoes an MRI annually to monitor the dynamics. With a progressive course complicated by epileptic seizures, the arachnoid cyst is treated surgically:
- complete excision - for hemorrhages in the cyst area. Treatment with a high risk of injury and long-term rehabilitation;
- endoscopy - fenestration of the formation with fluid extraction;
- cystoperitoneal shunting - installation of a shunt to drain fluid into the abdominal cavity.
The choice of surgical intervention is decided by a neurologist and a neurosurgeon.
Consequences, prognosis, prevention
The patient can live his whole life with an arachnoid cyst without any symptoms. A dangerous condition occurs with progressive cystic lesions. Delayed detection of pathology can cause a person’s neurological disability and even death.
Timely diagnosis and correctly performed surgery provide a favorable prognosis for the future and recovery of the patient. Sometimes relapse and formation of new cysts are possible.
If you find yourself with the symptoms described above, then contact your doctor. Our specialists will prescribe the necessary diagnostic and treatment procedures.
Click the "SIGN UP" button and come see us.
How is pathology therapy carried out?
When an MRI picture of arachnoid changes of a liquor cystic nature is revealed, the issue of treating the cyst is decided. Indications for surgical intervention are:
- presence of neurological disorders;
- large or enlarging cyst;
- cyst in the brain stem area.
In the absence of symptoms, there is no need for treatment, since brain surgery can provoke inflammatory diseases of the brain and its membranes.
For arachnoid cysts, several types of surgery are performed:
- Endoscopic or microsurgical bypass of the cyst. The essence of the operation is that a shunt is inserted into the cavity of the cyst, which serves to drain cerebrospinal fluid from the cyst (most often into the internal jugular vein). This method has two significant advantages: the shunt allows you to constantly drain cerebrospinal fluid from the cyst, the walls of which are lined with cerebrospinal fluid-producing epithelium; endoscopic intervention can reduce the invasiveness of the operation to a minimum. The only drawback is that the shunt operates due to a pressure difference, and blood may enter it, clots may form and the shunt will become blocked, which leads to a sharp deterioration in the patient’s condition. Nevertheless, this method of treatment is considered the main one.
- Removal of cerebrospinal fluid. A one-time operation to clean out the cyst cavity. Currently, it is practically not used, since a single removal of cerebrospinal fluid does not provide a permanent effect.
- Cyst excision. The most radical operation to eliminate the cause of the disease. To do this, craniotomy is performed and part of the arachnoid membrane is excised along with the cyst. The advantages of the method are that the cyst is completely removed and cannot recur; the disadvantage is that it is highly traumatic and the risk of developing postoperative complications.
If surgical treatment is not possible (for example, because the position of the cyst does not allow surgery), then drug therapy is performed. This includes drugs that affect the course of the underlying disease, which can cause a cyst: immunomodulators, if necessary, antiviral drugs and antibiotics, drugs that improve blood supply to the brain.