Terminology
There are many synonyms for this pathology, including the terms cavernous hemangioma , cerebral cavernous malformation , or simply cavernoma . This pathology does not relate to neoplastic processes, therefore the terms hemangioma and cavernoma should be avoided. Additionally, it is important to note that according to the latest ISSVA nomenclature for classifying vascular anomalies, these changes correspond to low-velocity venous malformations. cavernous in the description or conclusion is useful, since this term is best known to most clinicians.
Brain stem cavernomas
Treatment of cavernous angiomas of the brain stem has a number of features that justify the classification of this pathology into an independent group. First of all, the anatomy and functional significance of the trunk makes surgical interventions in this area extremely difficult. Due to the compact location of a large number of various, including vitally important, formations in the brain stem, any, even minimal, hemorrhages from the trunk cavernomas cause neurological disorders, which distinguishes the course of the disease from the clinical manifestations of cavernomas of the cerebral hemispheres. The small size of trunk cavernomas often complicates histological verification of the pathology, and therefore the nature of the disease more often than with cavernomas of other localization remains unrecognized. According to MRI and surgical data, three variants of pathological formations can be distinguished, united by the general name “trunk cavernomas”: - subacute and chronic hematomas, when removed only in 15% of cases it is possible to verify the cavernous tissue. It cannot be ruled out that these hematomas are based on malformations other than cavernomas, possibly telangiectasia; - typical cavernomas in combination with acute, subacute or chronic hematoma; - typical cavernomas having a heterogeneous structure and surrounded by a ring of hemosiderin, without signs of hemorrhage. In the clinical course There are two main options for barrel cavity. The stroke-like variant is characterized by the acute development of pronounced brainstem symptoms, often against the background of intense headache. This option occurs, as a rule, with trunk hematomas without MRI signs of cavernoma. The pseudotumorous variant is characterized by a slow increase in stem symptoms, sometimes lasting up to several months. This course is typical for patients with a typical MRI picture of cavernoma. In both variants of the course, clinical symptoms gradually stabilize, and in the future they may completely or partially regress. Analysis of the results of surgical interventions showed that they clearly depend on the type of formation identified. Thus, when subacute and chronic hematomas of the trunk were removed, regression of symptoms occurred in 80% and 60% of cases, respectively. When removing cavernomas with signs of hemorrhage, the clinical outcomes were less satisfactory, and when removing cavernomas without signs of hemorrhage, the outcomes were generally unsatisfactory. The identification of these patterns formed the basis for determining the indications for surgical intervention.
Morophology
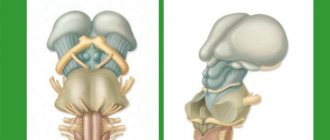
Macroscopically, cavernous venous malformation looks like a mulberry. On histological examination, cavernous venous malformations are thin-walled cavities of irregular shape, the walls of which are formed by endothelium. The cavities may be closely adjacent to each other, or be separated by collagen fibers or fibrous tissue, unlike AVMs, which may have medulla between the loops. In some cases, they are closely associated with developmental venous anomalies (DVA) and in this case it is a mixed vascular malformation.
Origin of cavernous angioma
Cavernous hemangioma is a type of infantile hemangioma. It occurs in the vast majority of cases in children and is congenital, but not hereditary. It is a pathological proliferation of blood vessels that form cavities (cavities) filled with blood. Under a microscope, overgrown vessels are visible, chaotically woven into knots.
The disease is benign in nature, although it grows rapidly and grows into surrounding tissues. It is rare - it accounts for 7% of vascular tumors according to WHO observations. The ICD-10 code is D18.0.
The exact causes of the disease are unknown. It is assumed that in the first trimester of pregnancy there is a disruption in the formation of the fetal vascular system. Predisposing factors: prematurity, pregnancy pathology, multiple pregnancies, viral diseases, bad habits and other factors that negatively affect the condition of the unborn child.
This type of tumor also occurs in adults, but is extremely rare. Reasons: disruption of blood vessels due to diseases of internal organs, toxic effects of certain drugs, radiation, excessive exposure to UV rays, poor ecology.
Liver hemangioma is a mysterious disease; the reasons for the development and growth of tumors have not yet been precisely established. Cavernous hemangioma occurs in approximately 2% of the population, with men affected less frequently than women. The disease can occur at absolutely any age; as a rule, it is diagnosed in patients 30-50 years old.
The disease is characterized by the proliferation of vascular walls with the formation of cavities (cavities). In fact, hemangioma is a benign formation, but it necessarily requires observation and, if necessary, timely and high-quality treatment.
Cavernous hemangioma does not pose a threat to life; if it is formed near physiological openings and on the mucous membranes, it can cause a lot of discomfort. When a hemangioma grows near the external auditory canal or eyes, there is a risk of deafness and blindness.
Cavernous hemangioma is a benign tumor in the liver. Symptoms are absent in most patients, often becoming obvious only when the tumor increases significantly. The incidence of the disease is approximately 7% of the population. More often, the pathological process is found in women.
The liver is an organ that lacks nerve endings.
What then worries people who, when they come to see a doctor, complain of pain under the ribs on the right side? Often one of the causes of pain in the right hypochondrium is cavernous hemangioma of the liver, which poses a serious threat not only to the organ, but also to health in general. Everything about the causes, symptoms and features of therapy is in this material.
There are two types of this disease: hereditary or sporadic.
- The mechanism of the congenital type of the disease is considered to be more studied, but there is also evidence of an autosomal dominant nature of inheritance; characteristic genes of the seventh chromosome have been identified and established, which affect the formation of pathological vascular ligaments
- The causes of sporadic tumors are still unknown. There are three scientific theories: the result of radiation, inflammation of the immune system, infection.
Localization of angiomas:
- 80% of angiomas are located in the upper lobes of the central brain. 65% of their component falls on the frontal, temporal and posterior parts. 15% on vascular occurrences of optical convexity.
- 8% are neocerebellum hemangioma.
- 2.5% vascular configurations in the dorsal medulla.
Detection is determined by the location of the tumor. The first signs are: migraine, not eliminated by medications; convulsions; sounds in the ears; disorganization of coordination; bouts of vomiting and nausea; weakness of the limbs; degradation of hearing and vision; memory distortion; disorder in speech. It happens that the angioma is “silent”. People don't even know about the disease. The tumor is detected when tested for other diseases or when it manifests itself in other family members.
Treatment of cavernoma should begin with a comprehensive diagnosis according to a regimen prescribed by doctors, which is created personally for the patient.
Diagnostics
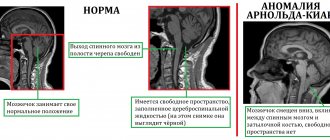
Cavernous venous malformations of the brain are localized supratentorially in ~80% of cases, but in general can be localized in any part of the brain, including the brainstem. Most often they are single, but at the same time, in one third of patients with sporadic formation, more than one malformation may occur.
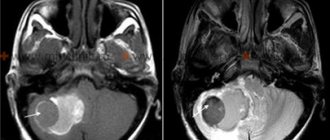
Computed tomography Large malformations are visualized by computed tomography as areas of increased density, in the presence of subacute hemorrhage, surrounded by perifocal edema, which do not enhance with contrast. Small malformations are difficult to distinguish.
Magnetic resonance imaging Magnetic resonance imaging is the method of choice. The classic sign is of popcorn or berries, surrounded on the periphery by a ring-shaped zone of signal loss due to the presence of hemosiderin and characterized by increased magnetic susceptibility.
- T1 and T2 MR signal is variable depending on the stage of breakdown of hemoglobin products in the malformation and fluid-liquid levels may sometimes be visualized.
- Gradient echo or T2* sequences are better at detecting malformations than T1 and T2 weighted images. In patients with a hereditary form of multiple cavernous malformations, they are important for counting the number of lesions that may be missed on spin echo sequences.
- Magnetic susceptibility-weighted images (SWI) have a sensitivity comparable to gradient sequences in detecting capillary telangiectasia, and they are also highly sensitive to detecting calcifications compared with T1- and T2-weighted images.
In the presence of recent hemorrhage, moderate perfiocal edema may be detected. Basically, the T1 MR signal intensity does not change after the administration of a contrast agent, but at the same time this is possible.
Selective angiography Kvernous malformations are not visualized during angiography, and arteriovenous shunts are not detected.
Etiology and pathogenesis
| Multiple cavernomas in a patient with a familial form of the disease |
Cavernomas can be sporadic and hereditary. The etiopathogenesis of the disease is most well studied for the hereditary form of the pathology. To date, an autosomal dominant type of inheritance has been proven and three genes have been identified, mutations of which lead to the formation of cavernomas: CCM1/Krit1 (locus 7q21.2), CCM2/GC4607 (locus 7q13-15), CCM3/PDCD10 (locus q25.2-q27 ). Studies to decipher the molecular mechanisms of the implementation of these genes have shown that the formation of cavernomas is associated with a violation of the formation of endothelial cells. It is believed that the proteins encoded by the three genes work in a single complex complex. The etiology of sporadic cavernomas remains unclear. It has been proven that some cavernomas can be radioinduced. There is also an immune-inflammatory theory of the genesis of the disease. The main mechanism for the development of any clinical symptoms in patients with cavernomas is single or repeated macro- or microbleeds. The criteria for the diagnosis of cavernoma hemorrhage remain the subject of debate. The importance of this issue is due to the fact that the frequency of hemorrhages is one of the main factors in determining the indications for surgery, as well as in assessing the effectiveness of various treatment methods, especially radiosurgery. Depending on the criteria used, the incidence of hemorrhage varies widely, from 20% to 55%. According to various sources, the frequency of hemorrhages ranges from 0.1% to 2.7% per cavernoma per year.
Differential diagnosis
Kvernous venous malformations should be differentiated from numerous other pathologies leading to multiple microhemorrhages, including:
- cerebral amyloid angiopathy
- chronic hypertensive encephalopathy
- diffuse axonal injury
- cerebral vasculitis
- radiation damage to the brain
- hemorrhagic metastases
- Parry-Romberg syndrome
Large malformations can simulate:
- hemorrhage into metastases
- hemorrhage into a primary tumor (eg glioblastoma)
Cavernous hemangioma of the liver
When mucus appears from the anus, it signals various diseases. A similar symptom is typical for infectious diseases of the intestine, with its injury; ulcer or cancer. If you get sick, you should not neglect treatment so as not to provoke a chronic disease; and change your diet.
Often, mucus discharge occurs due to cracks in the intestine. They are provoked by constipation and diarrhea. To normalize stool, you should take bifidumbacterin, bifekol, lactobacterin. After defecation, take a bath with potassium permanganate or do an enema with chamomile.
To heal cracks, suppositories with sea buckthorn oil, ultraproct and posteran forte are inserted. Among the physiotherapeutic methods, laser therapy stimulates the elimination of cracks. To prevent constipation from injuring the anus, its cause is eliminated.