When several or all eye muscles are paralyzed, ophthalmoplegia occurs. This condition may occur due to damage to the optic nerves. In this case, one or both eyeballs may be damaged. Their motor ability is limited or lost in some types of disease. Let's look at the causes of ophthalmoplegia and methods of treatment.
In this article
- Causes of ophthalmoplegia
- Types and symptoms of ophthalmoplegia
- Diagnosis of the disease
- Treatment methods for ophthalmoplegia
- Complications of ophthalmoplegia
- Prevention
Causes of ophthalmoplegia
Various factors can serve as prerequisites for the development of this pathology. It can be either congenital or acquired as a result of certain diseases. At the same time, ophthalmoplegia occurs with equal frequency in men and women. Here are the most common causes of optic nerve palsy:
- severe infectious diseases, for example, tetanus, diphtheria, botulism;
- eye tumors and neoplasms;
- muscle dysfunction (myasthenia gravis, etc.);
- traumatic brain injuries;
- pathologies of the endocrine system - diabetes, problems with the thyroid gland;
- encephalitis;
- severe intoxication of the body;
- food or alcohol poisoning;
- chronic sinusitis;
- multiple sclerosis;
- brain diseases;
- trigeminal neuralgia;
- CNS diseases and other factors.
If any of these cases occurs, disruption of the activity of the nerves responsible for muscle contraction may occur. There are three in total:
- oculomotor, with the help of which we are able to turn the eyeball in different directions: up, down, towards the nose;
- block-shaped, providing the ability to rotate to the lower temporal angle;
- abducens - this nerve is responsible for turning the eyeball towards the temple.
Violation of the innervation of the muscles leads to a loss of their tone and the inability to move the eyes - paralysis occurs. Ophthalmoplegia has different forms.
Treatment of chronic progressive external ophthalmoplegia
There is no treatment that addresses the cause of chronic progressive external ophthalmoplegia. There is evidence of clinical improvement in overall neurological function in patients treated with CoQ10 (coenzyme Q10) who are deficient in this enzyme, but large-scale studies have not been conducted. To eliminate ptosis, it may be recommended to wear special glasses that prevent drooping of the upper eyelid (ptosis crutch glasses), or surgery (individually, due to the threat of keratopathy).
Features and advantages of treatment of chronic progressive external ophthalmoplegia at the Rassvet clinic
Chronic progressive external ophthalmoplegia can develop as an isolated disease or occur against the background of other typical or rare pathologies. In this regard, CPEO can have a variety of clinical manifestations, and the main task of the doctor becomes to accurately establish its nature and conduct a differential diagnosis. Not only the selection of effective treatment tactics, but also the patient’s prognosis depends on this.
The prognosis of patients with an isolated form of CPEO is usually favorable, and their life expectancy tends to be normal. Although the clinical manifestations of the disease tend to worsen over time, the prognosis depends on the specific symptoms and severity of the disease, which can vary greatly from person to person. In the syndromic form of CPEO, the prognosis depends not only on its symptoms, but also on the symptoms of the underlying disease.
In the first and second cases, it is very important to make an accurate diagnosis, not treat what does not exist and use effective methods of symptomatic or supportive therapy. All doctors at our clinic, including ophthalmologists, are fully aware of this specific knowledge and skills, which are necessary in the treatment of any rare pathology. They work closely with neurologists and doctors from other fields, specializing in complex diagnoses and rare diseases. Dawn doctors do not prescribe unnecessary tests and drug therapy with unproven effectiveness, and do not perform unnecessary surgical interventions.
Types and symptoms of ophthalmoplegia
In modern medicine, the disease is divided into several main types:
- Internal ophthalmoplegia. It is characterized by weakening or paralysis of the muscles of the iris and ciliary body. In this case, the mobility of the eye is not impaired, but the pupil is permanently dilated, and a spasm of accommodation may also be observed.
- External ophthalmoplegia. With this type of pathology, the muscles on the outside of the eyeball are affected. At the same time, it can hardly move or is completely paralyzed. The external type of ophthalmoplegia is characterized by diplopia - double vision, but the pupil's reaction to light is preserved. Due to the uneven distribution of the tear film, the dryness of the mucous membrane of the eyes increases. Patients also complain of increased lacrimation. Internal and external ophthalmoplegia can also be partial or complete. In complete ophthalmoplegia, both the external and internal muscles of the visual organs are affected.
Total ophthalmoplegia is also characterized by immobility of the eyeballs and drooping (ptosis) of the upper eyelids - this condition is called Hutchinson's face. The patient has to tilt his head back to be able to see normally from under drooping eyelids. Partial ophthalmoplegia is a condition during which paresis of only the external or only the internal muscles of the eye develops.
- Internuclear ophthalmoplegia. This type of disease is characterized by damage to the muscles that are responsible for the simultaneous movement of the eyeballs. With unilateral internuclear ophthalmoplegia, one of them can be fixed in some position, and on the second, nystagmus occurs - frequent involuntary twitching. Most often, internuclear ophthalmoplegia is a consequence of multiple sclerosis, as well as stroke, head injuries, drug intoxication and some other risk factors. Patients complain that they cannot look in the same direction with both eyes at the same time.
- Supranuclear ophthalmoplegia. Its other name is Steele-Richardson-Olszewski syndrome. This is a rare brain disorder that causes problems with motor function and eye movements. It is also characterized by gaze paralysis - there is no simultaneous eye movement up and down or left and right. Many people complain that they are not able to direct their gaze in the right direction at will.
Treatment of ophthalmoplegia
The main task in the treatment of ophthalmopelgia is the elimination or correction of the causes that caused it. Therefore, a narrow specialist, a neurologist, deals with the disease together with an ophthalmologist. Complex therapy of the disease is carried out in three areas, including:
- Drug treatment - prescribing drugs to improve blood circulation, vitamin therapy.
- Physiotherapeutic treatment - the appointment of electrophoresis with drugs, galvanization, acupuncture and acupuncture.
- Surgical treatment – surgical elimination of the causes of damage to the oculomotor nerves, then surgical treatment of damage to the eye muscles (their plasticity and return of function).
Diagnosis of the disease
Ophthalmoplegia has characteristic external signs. But in order to distinguish it, for example, from paralytic strabismus, and also to identify the exact type, a number of diagnostic hardware tests are carried out:
- Ultrasound of the eye allows you to detect the features of the eyeballs and study the condition of the orbital cavity;
- X-ray of the skull - the image will show internal damage, if this is the cause, as well as the condition of the sinuses;
- computed tomography of the head and neck makes it possible to detect neoplasms, which are one of the causes of ophthalmoplegia;
- proserine test for the diagnosis of myasthenia gravis;
- angiographic examination of cerebral vessels;
- perimetry to determine the boundaries of the field of view.
Depending on what is the cause of the disease, consultation and examination by highly specialized specialists is also required: in case of a neoplasm - an oncologist, in case of suspected pathology of the central nervous system - a neurologist.
How does the disease manifest itself?
Internuclear ophthalmoplegia is a disorder of synchronous movement of the eyeballs. Muscles and nerves control movement and normally perform their work in harmony.
In this article
- How does the disease manifest itself?
- Etiology of the disease
- Symptoms of internuclear ophthalmoplegia
- Diagnostics
- Treatment
- Forecast
Several external eye muscles are involved in the process. In practice, it looks like this: when you turn your gaze to the right, the right rectus lateral muscle and the left rectus medialis muscle contract. Control is exercised by the oculomotor nerve, which contains motor and autonomic fibers, and the overall control of the entire mechanism is performed by the pontine center.
Treatment methods for ophthalmoplegia
Treatment consists of eliminating the disease that caused the paralysis, as well as restoring the functionality of the muscles and nerves. Therapeutic interventions include several aspects.
Drug treatment. The patient may be prescribed various medications depending on the etiology:
- anti-inflammatory drugs;
- topical corticosteroids;
- vitamins B and C;
- nootropics to improve nervous activity;
- drugs that eliminate muscle weakness.
Hardware therapy. Along with taking medications, treatment using hardware procedures - electrophoresis, phonophoresis, acupuncture - also produces effective results. This helps strengthen the eye muscles and eliminate spasm.
Surgical intervention. It is prescribed if it is necessary to eliminate the tumor that is the cause of paralysis, as well as restore muscle activity of the eyes, and raise the upper eyelid with ptosis.
Three methods are used to influence muscles:
- myotomy (dissection);
- recession (pushing back);
- tenomyoplasty (lengthening).
Surgeries for ophthalmoplegia are aimed at restoring the correct balance between the eye muscles. The doctor decides what type of intervention is necessary, taking into account the existing form of pathology and its severity, the patient’s age and other characteristics. As a rule, several muscles are operated on at once. There are cases when a strengthening operation is performed on one eye and a weakening operation on the other.
The success of treating ophthalmoplegia depends on timely contact with specialists, as with many other diseases, and not only eye ones.
Ophthalmoplegia - causes and treatment
Ophthalmoplegia is a pathological condition of the organ of vision caused by damage to the oculomotor nerves. It develops against the background of complications of brain diseases, severe infectious lesions, and intoxications of the body. Ophthalmoplegia is manifested by paralysis of all or individual groups of the eye muscles, which leads to decreased mobility of the eyeball or its complete immobility. The disease can be detected in one eye or in both eyes at once.
Complications of ophthalmoplegia
The consequences of advanced ophthalmoplegia can have a very negative impact on the condition of the visual organs. Paralysis of the internal muscles leads to impaired accommodation and decreased visual acuity. Internuclear ophthalmoplegia can cause the development of persistent nystagmus.
Inflammatory diseases such as conjunctivitis, keratitis, blepharitis are often present; the patient’s normal functioning of the lacrimal and meibomian glands is disrupted. Paralysis of the eye muscles is accompanied by facial asymmetry. With supranuclear ophthalmoplegia, difficulties with orientation in space and imbalance also arise. Another common complication of ophthalmoplegia is xerophthalmia, drying of the conjunctiva and cornea.
Symptoms of internuclear ophthalmoplegia
The first and main sign that you should pay attention to is difficulty when trying to move your eyes. One (the healthy eye) moves normally, while the affected neighboring eyeball does not turn with it. An additional symptom is uncontrollable twitching that periodically occurs in the healthy eye. The general picture of the pathology is crowned by the deviation of the eyes from a single horizontal axis (that is, one is higher than the other).
A similar situation is observed with damage to the lower part of the bundle of nerve fibers in the region of the brain (medial longitudinal fasciculus), on which the implementation of motor, sensory, integrative and conduction functions—the pons—depends.
If there is a violation of the integrity of the fibers of the upper part, then the pathology spreads to the medial rectus muscles of each eye. A typical symptom in this case is convergence disorder, where the muscles lose the ability to converge on the observed object. The eyeballs diverge in opposite directions; this process can occur both horizontally and vertically. Additionally, an involuntary and uncontrollable oscillation is felt in each eyelid with periodic changes in direction.
Internuclear ophthalmoplegia affecting one eye may be aggravated by horizontal paresis of the neighboring eye, making it impossible to move the gaze in the horizontal direction. In this case, they speak of the onset of one and a half syndrome.
Prevention
There are no special preventive measures in this case. To reduce the risk of pathology, you need to adhere to general recommendations:
- after eye injuries, head bruises, you should monitor the condition of the visual organs; if discomfort occurs, you should visit an ophthalmologist for diagnostic purposes;
- engage in timely treatment of infections, preventing transition to the chronic stage;
- Observe precautions when frequently working with toxic substances;
- If there are factors that can lead to ophthalmoplegia, such as diseases of the nervous and endocrine systems, you should also undergo regular examinations by a specialist so as not to miss the development of pathology.
A careful and careful attitude to eye health will help to detect negative symptoms in time and begin appropriate therapy.
Causes
CPEO is caused by mutations in mitochondrial DNA (inherited or sporadic). The disease can be inherited in an autosomal recessive, autosomal dominant, or mitochondrial manner. The TWNK and SLC25A4 genes are involved in the autosomal dominant type of inheritance, POLG and RRM2B are involved in the autosomal dominant and autosomal recessive type of inheritance, the MTTL1 gene is most often associated with the mitochondrial type of inheritance, along with other mtRNA and mtDNA genes.
CPEO can occur against the background of other diseases: neuromuscular (POLG-associated ataxias), mitochondrial myopathies (Cairns-Sayre syndrome).
The prevalence of chronic progressive external ophthalmoplegia is unknown.
Prevention of ophthalmoplegia
No special preventive measures for ophthalmoplegia have been developed. Tips for preventing the disease boil down to increasing the body's resistance and reducing contact with substances that can cause intoxication. In addition, it is necessary to undergo timely treatment for diseases of an infectious nature, without letting them progress to severe stages. At the first unpleasant symptoms in the visual area, you should visit a doctor. Neglect of this rule leads to the development of serious complications.
Prices
| Disease | Approximate price, $ |
| Prices for diagnosing migraine | 7 060 — 8 260 |
| Prices for diagnosing childhood epilepsy | 3 100 — 4 900 |
| Prices for brain shunting for hydrocephalus | 33 180 |
| Prices for treatment of Parkinson's disease | 58 600 |
| Prices for migraine treatment | 9 680 |
| Prices for the diagnosis of amyotrophic lateral sclerosis | 6 550 |
| Prices for diagnosing epilepsy | 3 520 |
| Prices for rehabilitation after a stroke | 78 300 — 82 170 |
| Prices for treatment of childhood epilepsy | 3 750 — 5 450 |
| Prices for treatment of multiple sclerosis | 4 990 — 17 300 |
| Disease | Approximate price, $ |
| Prices for strabismus treatment | 14 190 |
| Prices for treatment of eye melanoma | 8 000 |
| Prices for treatment of keratoconus | 27 610 — 59 950 |
| Prices for cataract treatment | 8 690 |
| Prices for glaucoma treatment | 7 260 — 8 360 |
Diagnostics
The examination is urgent, the ability to see is at stake. The problem is solved by an ophthalmologist.
When complications develop, real or suspected, more specialized doctors are involved: a vitreosurgeon (a specialist in the internal parts of the organ of vision), others.
List of events:
Oral survey. What complaints do you have and when did they arise? Anamnesis collection. Briefly to understand the origin of the pathological process. Measuring intraocular pressure. As a rule, it is increased. How much depends on the type and location of the disorder. Assessment of visual acuity using standard methods. Using a table. On the side affected by uveitis, the indicators are significantly lower. Perimetry. Evaluation of visibility fields. Some scotomas and defects are invisible to either doctors or the patient until an assessment is carried out. Ophthalmoscopy. Fundus examinations using a special apparatus. It is possible to use a Goldmann lens to visually determine changes in the far periphery of the retina
An important condition is the dilation of the pupil, which is carried out using drops. Ultrasound. Shown relatively rarely. Goniospokia
Inspection of the anterior chamber of the organ. Ophthalmography. Used as part of assessing the quality of blood flow in the eye. Tomography. In order to differentiate various diseases.
It is possible to conduct laboratory tests:
- General and biochemical blood tests with determination of the concentration of C-reactive protein.
- Specific tests like the Wasserman reaction and a more modern analogue - the anticardiolipin test. Mainly as part of the diagnosis of syphilis, if there is suspicion.
- PCR. Identification of viral agents.
Neurogenic ptosis of the upper eyelid. What happens?
Neurogenic ptosis of the eyelid also has its own classification. Based on the level of damage to the nervous system, ophthalmologists distinguish the following types of ptosis of the upper eyelid:
- nuclear;
- supranuclear;
- hemispheric.
The appearance of each of these three types is influenced by different reasons. Let's tell you more about them.
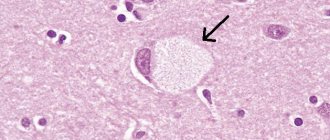
The nuclear type of ptosis of the upper eyelid can be unilateral or bilateral. The cause of the first is damage to the fibers of the central caudal region, and the cause of the second is damage to the entire central caudal region. It can also be asymmetrical, when both the central caudal region and its nerve fibers are affected on one side.
Ophthalmologists also say that bilateral ptosis is diagnosed more often with cerebral infarction and inflammatory changes, which, in turn, affect the border of the nucleus.
The cause of the second type of ptosis of the upper eyelid (supranuclear) may be damage to the pathways that pass in the middle part of the brain.
The third type of ptosis of the upper eyelid is a symptom of pathologies such as hemispheric infarction with extensive frontal lesions. In this case, the pathology is usually bilateral, but in practice a unilateral form has also been encountered.
It is interesting to know that when the oculomotor nerve is damaged, ptosis of the upper eyelid is most often associated with pupil dilation, as well as impaired eye mobility in all directions except the outer one. Neurologists note that ptosis of the upper eyelid, unilateral or bilateral, may also be due to the presence of myopathy or diabetic polyneuropathy. From all of the above, we can conclude that the work of the eye muscles directly depends on the functioning of the brain. And any, even seemingly minor damage can lead to a pathology called neurological ptosis of the upper eyelid. Only a highly specialized specialist can establish the true cause and understand what specific type of neurological form you are dealing with.