Home → Information about diseases → Hydrocephalus (hypertensive-hydrocephalic syndrome of HHS)
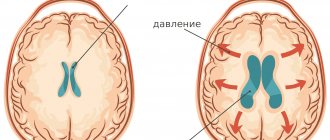
Absolutely all people have a small amount of fluid in the cranial cavity that washes the brain. This liquid is called “liquor”. Liquor is constantly produced and absorbed (renewed). If a person produces more cerebrospinal fluid than is absorbed, it begins to accumulate in the cranial cavity, and intracranial pressure increases. Excess fluid begins to put pressure on the brain, causing various disruptions to its functioning. This is called hydrocephalus (increased intracranial pressure, hypertensive-hydrocephalic syndrome or “dropsy of the brain”).
What is Hypertension-hydrocephalic syndrome (HHS)?
Hypertensive-hydrocephalic syndrome (HHS) is caused by excessive accumulation of cerebrospinal fluid (CSF) in the ventricles of the brain and under the meninges, resulting from obstruction of outflow, excessive formation and impaired reabsorption of cerebrospinal fluid. This is one of the most common syndromic diagnoses in pediatric neurology, especially in young children with perinatal encephalopathy (PEP). It should be noted that the term “hypertensive-hydrocephalic syndrome” is a concept used exclusively in Russia. The causes of HGS can be: unfavorable course of pregnancy and childbirth, hypoxic-ischemic brain damage, deep prematurity, intracranial hemorrhage and intrauterine infections, congenital malformations of the brain, neuroinfections. Research methods to judge the level of cerebrospinal fluid pressure are very limited. Currently, the only reliable and relatively accessible of them is to perform a lumbar puncture of cerebrospinal fluid (CSF) to measure CSF pressure, which is a diagnostic criterion for this pathology. HGS can be either one of the manifestations of hydrocephalus or many other neurological diseases. The diagnostic criteria for HGS include clinical symptoms that indirectly indicate an increase in cerebrospinal fluid pressure and dilation of the ventricles of the brain.
What is the prevalence of hydrocephalus? According to official statistics, up to 70% of newly born children suffer from an obvious (hydrocephalus) or latent form (hypertensive-hydrocephalic syndrome) of this disease.
What is the reason for the widespread incidence of hydrocephalus?
- Weakness of the nervous system of children born from parents who grew up in environmentally unfavorable conditions.
- A large number of “saved” premature babies.
- Frequent use of surgical delivery, which also contributes to the development of hydrocephalus.
- A busy schedule of vaccinations up to 1 year of age contributes to the exacerbation of latent hypertensive-hydrocephalic syndrome.
Early diagnosis (ultrasound, electropuncture) also helps to identify hidden forms of the disease hydrocephalus of the brain. There are many more reasons that can be found. But the fact remains: it is necessary to identify and treat hydrocephalus without waiting for exacerbations of the disease and complications.
What are the manifestations of hydrocephalus? In children under 1 year of age: increased excitability, “unreasonable” crying, sleep disturbance, frequent regurgitation, throwing the head back in sleep, increased muscle tone (hands held in fists, legs resting on toes and crossed), weak support with legs, lack of step reflex, delayed motor and mental development. In preschool children: hypermobility, aggressiveness, hysterical manifestations, stuttering, enuresis, strabismus, frequent colds, delayed psycho-speech development (poor vocabulary, impaired diction, difficulty constructing complex sentences). In schoolchildren: nosebleeds and headaches, memory and concentration are reduced, disinhibition and neuroticism are noted, learning school material is difficult: they complete tasks slowly, make a large number of mistakes, their hands get tired quickly, their handwriting is not even, they read slowly and poorly assimilate the material they read, find it difficult to write a competent story.
What are the worst complications of hydrocephalus? CONVISIONS, CEREBRAL PALSY, MORTONITY.
What factors cause exacerbation of hydrocephalus? Any stress on the body (viral infections, stress, mental and physical fatigue, concussion, vaccinations) can lead to an exacerbation of increased intracranial pressure - especially a combination of these. For example: studying at the gymnasium + flu + stress can lead to exacerbation of hydrocephalus, headaches and a decrease in academic performance and aggressiveness.
What to do if your child has any manifestations of hydrocephalus? Promptly seek advice from the children's department of neurology and reflexology at Reatsentr to clarify whether the child needs to be examined and treated.
Causes
Congenital
- The course of pregnancy and childbirth with complications.
- Hypoxic (bradycardia, intrauterine hypoxia and intrauterine growth retardation) and ischemic (trauma during childbirth) brain damage.
- Premature birth (up to 36-34 weeks).
- Head injuries during childbirth (subarachnoid hemorrhage).
- Intrauterine infections (toxoplasmosis, influenza, cytomegalovirus infection and others).
- Congenital abnormalities of brain development.
- Delayed birth (at 42 weeks and later).
- Long water-free period (more than 12 hours).
- Chronic diseases of the mother (diabetes mellitus and others).
Purchased
- Tumors, abscesses, hematomas, parasitic cysts of the brain.
- Foreign bodies in the brain.
- Fractures of the skull bones.
- Causeless intracranial hypertension.
- Infectious diseases (malaria, tick-borne encephalitis).
- Metabolic disorders.
Treatment methods for hydrocephalus
The surgical method of treating hydrocephalus is used only in extreme cases (decompensated forms of internal hydrocephalus), excess fluid is drained from the cranial cavity into the abdominal cavity using a tube (shunt), this operation, like any other, is quite traumatic; in the future, several more surgical operations may be required interventions to replace and check the operation of the shunt.
A medicinal method of treating hydrocephalus - the use of diuretics, such as Diacarb, is often used by neurologists in outpatient practice. Diakarb removes fluid not only from the cranial cavity, but also from the body as a whole, at the same time a loss of microelements occurs, the effect of this treatment method is temporary, after its cessation, the fluid begins to accumulate again and intracranial pressure increases.
Herbal medicine - the use of diuretic herbs (horsetail, fennel, lingonberry leaf), does not cause addiction and loss of microelements. It is used, as a rule, for preventive purposes: to avoid exacerbation of hydrocephalus during colds, when changing climatic zones, in the autumn-spring period with pronounced changes in weather conditions.
Massage is an effective method for children with motor impairments (increased muscle tone, delayed motor development), and is mainly aimed at relaxing tense muscles. It is advisable to use only in complex treatment, since massage does not affect the main cause of the disease - hydrocephalus and hypoxia of the cerebral cortex.
MICROCURRENT REFLEXOTHERAPY - the method is effective in children with various manifestations of hydrocephalus, it allows you to eliminate not only external manifestations (hysterics, developmental delays, etc.), but also treat hydrocephalus itself, that is, it has a complex therapeutic effect on the body. The effect of treatment is stable and does not stop after the end of treatment.
Symptoms
- Decreased muscle tone (“seal feet” and “heel feet”).
- Weak congenital reflexes (swallowing, grasping).
- The appearance of tremor (shaking) and convulsions.
- Vomiting like a fountain.
- Strabismus.
- Graefe's sign (a white stripe between the pupil and the upper eyelid).
- Rising sun sign (the iris is almost half hidden behind the lower eyelid).
- Opening of the sutures of the skull, bulging and tension of the fontanel.
- Increased head circumference growth (by 1cm every month).
- Swelling of the optic discs.
In order to establish the true cause of hypertensive-hydrocephalic syndrome, it is necessary to conduct a comprehensive clinical examination of the child:
- Echoencephalography (EchoEG); rheoencephalogram (REG); radiography of the skull; computed tomography (CT); electroencephalography (EEG).
- Examinations by such specialists as an ophthalmologist, a neurologist, a psychiatrist (long-term hypertensive-hydrocephalic syndrome can lead to atrophy of the cerebral cortex and, subsequently, to delayed mental development), and a neurosurgeon are necessary.
Hypertension syndrome in children
headache syndrome child meningitis encephalitis hypertension asthenia central nervous system attack
Category: For young and expectant mothers
Hypertension syndrome is a clinical manifestation of increased intracranial pressure. Disturbances in the secretion, resorption and circulation of cerebrospinal fluid, venous congestion in the cranial cavity, and an increase in brain volume play a role in the occurrence and development of intracranial hypertension. These changes occur in various pathological conditions: inflammatory diseases of the brain and its membranes (meningitis, encephalitis, arachnoiditis), viral infections (influenza, measles, chickenpox, mumps, etc.), traumatic brain injuries, brain tumors, anomalies development of the brain and cerebrospinal fluid system (cranial hernia, hydrocephalus, microcephaly, craniostenosis, intracranial aneurysm). Despite the variety of diseases leading to increased intracranial pressure, hypertension syndrome has characteristic neurological features that make it possible to distinguish it in the overall clinical picture of the underlying disease. The main manifestation of hypertension syndrome is headache. Oka occurs as a result of irritation of the branches of the trigeminal and vagus nerves, receptors of the soft membrane, veins, and sinuses of the brain. The headache occurs in paroxysms, often in the morning, sometimes at night, is of a diffuse, bursting nature, and intensifies after physical activity with the head tilted down, jumping, running, or prolonged exposure to the sun. It is usually accompanied by vomiting that occurs suddenly, unrelated to food intake. Pathogenetically, the mechanism of vomiting is explained by irritation of the vomiting center and vestibular analyzer due to a sharp increase in intracranial pressure. Patients cannot tolerate riding, swings, etc. Intracranial hypertension quickly leads to asthenia of the nervous system and emotional disturbances. General lethargy, lack of initiative, decreased memory, attention, performance, and academic performance are often noted. Against this background, children often experience attacks of disinhibition and psychomotor agitation. Many people have trouble sleeping. Noticed; that with hypertension syndrome, children prefer to sleep on a high pillow. In young children, the symptom complex of increased intracranial pressure is manifested by general anxiety, screams, bulging of the large fontanelle, and vomiting. Among the causes leading to the development of hypertension syndrome, the consequences of inflammatory diseases of the brain and its membranes, as well as traumatic brain injury, deserve special attention. Such patients make up 15% of patients seen by pediatric neurologists. Hypertension syndrome usually develops within 1 year after the acute period. Its course is remitting, with periods of deterioration, which are accompanied by hemodynamic (hypertensive) crises. They are characterized by a paroxysmal onset, a combination of headache with nausea, vomiting, and dizziness. After the crisis, patients feel better. The frequency of crises varies - from 2-3 times a year to 1-2 times a month. It has been noted that in preschool children, curves develop less frequently and during the interictal period, most patients do not complain of headaches. In school-age children and during the interictal period, increased fatigue, sleep disturbances, behavior disorders, decreased memory, academic performance, and headache after physical activity are noted. Apparently, these differences are associated with the anatomical and physiological characteristics of the cerebrospinal fluid system and the degree of adaptive mechanisms in children of different ages. Deterioration of the condition in most patients occurs in the autumn and spring periods, as well as after repeated injuries, acute respiratory infections, exacerbations of the underlying disease. In children who have suffered central nervous system lesions during childbirth, hypertension syndrome is often transient (transient) in nature. This is due to the fact that it is often based on functional disorders of liquor dynamics with dysfunction of liquor-producing systems due to hypoxic effects combined with birth stress. As cerebral circulation is restored, the resorbing systems mature, and edema disappears, liquor dynamics normalize, the hypertension syndrome stabilizes, and then reverses. The child’s skull and brain have great compensatory capabilities for increased intracranial pressure. The capacity and size of the skull easily increases due to the softness of the bones, the divergence of the sutures, and the elasticity of the brain. This leads to the fact that the initial period of the tumor process in children is secretive and asymptomatic. The onset of intracranial hypertension in these cases is behavioral changes and hypertension syndrome. The latter in such cases is of a steadily progressive nature with frequent hypertensive crises, repeating first in the morning and night hours, then at any time. The headache becomes constant, the size of the head increases, and symptoms of focal brain damage appear. If a tumor is suspected, especially in children of the first years of life, it is necessary to take into account the possibility of a long absence of focal symptoms and not delay consultation with a neurosurgeon. In the diagnosis of hypertension syndrome, along with general clinical examinations, the leading role is played by otoneurological examination and lumbar puncture. The X-ray picture of the skull in patients with intracranial hypertension can be varied. Craniograms reveal changes in the shape of the skull, an increase in its size, thinning of the bones, smoothing of the vault arches, flattening of the base, changes in the sutures and fontanelles, strengthening of the pattern, “finger indentations,” changes in the internal relief of the skull and sella turcica. However, the listed X-ray changes in the skull are observed in their entirety quite rarely. Identification of a pattern of digital impressions in children, if it is not combined with clinical symptoms, does not necessarily indicate increased intracranial pressure. Fundus examination plays an important role in the diagnosis of hypertension syndrome. In the fundus, initial signs of papilledema are detected (blurred borders, dilatation, tortuosity, congestion of veins) with hemorrhages and prominence, symptoms of secondary optic nerve atrophy. Fundus examination plays a leading role in the dynamic monitoring of patients with hypertension syndrome. It should be noted that in a number of patients, the syndrome of intracranial hypertension in the initial stage occurs latently and its first sign is often swelling of the optic discs, detected during a routine examination. In young children, the cranial transillumination method is widely used in the diagnosis of hypertension syndrome. In recent years, echoencephalographic research has become widespread. Intracranial hypertension is manifested on the echoencephalogram by dilatation of the ventricle and changes in echo signals. To date, the most reliable method for diagnosing intracranial hypertension is direct measurement of cerebrospinal fluid pressure during lumbar puncture. The latter is carried out after performing the study using the described methods, not only for diagnostic, but also for therapeutic purposes. The main thing in the treatment of patients with hypertension syndrome is measures to reduce the production of cerebrospinal fluid, improve cerebrospinal fluid resorption, and accelerate venous outflow. Treatment in the acute period and during the period of exacerbation in most patients is carried out in a hospital setting. Diacarb is used as a means of reducing the production of cerebrospinal fluid and simultaneously causing an increase in diuresis and dehydration. For the same purpose, you can use furosemide (Lasix), a 25% solution of magnesium sulfate, a 50% solution of glycerin, and sorbitol. To improve the outflow of cerebrospinal fluid through the cerebral venous system, aminophylline and rigematin are prescribed. In addition to these therapeutic measures aimed at reducing intracranial pressure, courses of anti-inflammatory, desensitizing and resorption therapy, and physiotherapeutic procedures should be carried out (if a brain tumor is excluded). To improve metabolic processes in nerve cells and reduce cerebrosthenic symptoms, B vitamins, aminalon, glutamic acid, lipocerebrin, nootropil, and courses of sedative therapy are indicated. Preventive courses of dehydration, anti-inflammatory, restorative therapy in the autumn and spring periods are very effective. Patients with hypertension syndrome should consult a pediatric neurologist at least 2 times a year. A fundus examination (at least 1–2 times a year) and an X-ray examination of the skull (once every 2–3 years) are required. For frequent exacerbations, training in sanatorium-forest schools is recommended. Children who have suffered inflammatory diseases of the brain, its membranes, as well as traumatic brain injury, are subject to dispensary observation. The appearance of frequent headaches, combined with vomiting and dizziness, should alert healthcare workers. Hypertension syndrome is a serious complication and manifestation of serious diseases, therefore, when its first signs appear, an urgent examination of the child is necessary to determine the cause of hypertension and carry out the necessary treatment measures in a hospital.
Please like if you liked the article/was useful
www.38i.ru