A little anatomy and physiology
Hydrocephalus (dropsy of the brain) (from the gr. “hydro” - water, “cephalon” - head) is a condition accompanied by an increase in the volume of the ventricles of the brain. The human brain has several interconnected cavities filled with cerebrospinal fluid (CSF). These cavities are called ventricles. The ventricular system consists of two lateral ventricles, which connect to the slit-like third ventricle (III ventricle), which, in turn, through a thin canal (Aqueduct of Sylvius) connects to the fourth ventricle (IV ventricle). Liquor is produced in the choroid plexuses of the ventricles and moves freely from the lateral to the fourth ventricle, and from there into the subarachnoid space of the brain and spinal cord (the subarachnoid space is the space between the brain and the dura mater), where it washes the outer surface of the brain. There it is reabsorbed into the bloodstream. Liquor is a clear, colorless liquid, very similar in appearance to water, containing a small amount of cells, protein and salts. In an infant, the amount of cerebrospinal fluid is about 50 ml, in a teenager and an adult - up to 120-150 ml. Liquor is constantly produced and absorbed; up to 500 ml of cerebrospinal fluid are produced per day by the choroid plexuses of the brain.
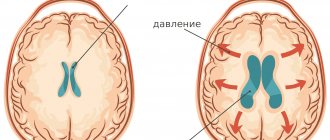
Any disturbance in the system of liquor production, liquor circulation and absorption of liquor leads to its excessive accumulation in the cavities of the brain, which is called hydrocephalus, or dropsy of the brain.
What is hydrocephalus?
The term hydrocephalus is formed from two Greek words: “hydro” - water and “cephalus” - head (“dropsy of the brain”). In hydrocephalus, there is a significant buildup of cerebrospinal fluid (CSF) inside cavities of the brain called ventricles. An increase in the volume of cerebrospinal fluid (CSF) occurs when the balance between the production of cerebrospinal fluid and its absorption and further removal from the body is disturbed. This may be the result of a deficiency in the circulatory system or excessive production of cerebrospinal fluid. Hydrocephalus can be congenital or acquired. The concept of congenital hydrocephalus means that it appears from the moment of birth. The disease can be provoked by various factors: traumatic brain injury, brain tumor, necrosis, meningitis, etc. The frequency of this disease is high throughout the world. According to the literature, hydrocephalus affects 5-15 children out of every thousand newborns. Treatment consists of diverting CSF outside the cerebrospinal fluid system into body cavities where it can be absorbed (absorbed). An effective operation allows a child to live and develop normally, study in a regular school, and an adult to return to a full, active life. However, patients and their loved ones must be able to recognize the signs and symptoms of postoperative complications so that medical care can be provided in a timely manner.
Types of hydrocephalus
In cases where there is an obstacle on the path of the cerebrospinal fluid from the lateral ventricles to the exit from the fourth ventricle and the cerebrospinal fluid cannot freely enter the subarachnoid space, hydrocephalus is called non-communicating (closed, occlusive). In other cases, hydrocephalus is called communicating (open). Hydrocephalus can be primary (as the underlying disease) and secondary, i.e., a complication of other diseases (tumors, malformations of the central nervous system (CNS) and cerebral vessels, etc.). There are many classifications of hydrocephalus, but these are the main ones and are used most often.
Manifestations of hydrocephalus
Impaired circulation and absorption of cerebrospinal fluid leads to its excessive accumulation and increased intracranial pressure. This manifests itself differently in children under 2 years of age and in older children.
The main symptom of the development of hydrocele in children under 2 years of age is accelerated growth of head circumference. The sutures of the skull in babies have not yet healed, and the size of the head increases because the bones of the skull are pushed apart from the inside by the growing brain. In the same way, a balloon increases in volume when we inflate it. There is a graph for head circumference growth. It must be measured every one to two months; this is done by the local pediatrician during preventive examinations. If the baby’s head grows faster than normal, this is an alarming symptom; it most often indicates the development of hydrocephalus, when accelerated head growth occurs due to an excess of cerebrospinal fluid in the ventricles of the brain. This is often the first symptom of the disease. In addition to accelerated head growth in children, an enlarged and bulging large fontanelle can be detected, which should close by approximately 1 year, but with hydrocephalus it can be open until 2 or even 3 years. The bones of the skull become thinner, the forehead becomes disproportionately enlarged and protruding. A venous network appears on the forehead and face. In more advanced cases, the eyes may droop downwards (Graefe's symptom). The tone of the leg muscles increases. Convulsive seizures may occur.
The child begins to lag behind in the rate of psychomotor development. He doesn't hold his head in time, doesn't sit, doesn't get up, doesn't play. A sick child is lethargic, apathetic, and at times unmotivatedly whiny. The baby may be experiencing a headache: he may clutch his head.
Most symptoms of increased intracranial pressure can only be recognized by an experienced pediatrician, neurologist or neurosurgeon, but parents can measure the rate of head growth themselves and check it using special charts. In any case, the accelerated growth of the child’s head circumference, as well as an incomprehensible lag in the pace of its development, should serve as a reason for a serious examination of the baby by a neurologist or neurosurgeon to rule out hydrocephalus.
In children over 2 years of age, the sutures of the skull heal, and the increase in intracranial pressure manifests itself differently. The classic picture is headaches with nausea and vomiting (usually at night or in the morning), changes in the fundus of the eye (the so-called papilledema, which can be detected by an ophthalmologist). Headaches, especially with nausea and vomiting, are symptoms that require evaluation by a neurologist or neurosurgeon. They can be caused by hydrocephalus, brain tumor, or malformations of the brain. Pediatricians often forget about this, and children are treated for a long time and aimlessly for gastritis, pancreatitis, biliary dyskinesia, poisoning and gastrointestinal infections, etc., and are brought to a neurologist and neurosurgeon late in a serious condition. It is necessary to insist on a consultation with a neurologist and examination in case of unclear headaches, regular episodes of nausea and vomiting, decreased vision, and in some cases this will allow an early diagnosis to be made and save the child’s life.
Other symptoms of hydrocephalus are varied and depend on the cause that caused it. These may be epileptic seizures, blurred vision, increased tone in the legs, pelvic disorders (incontinence or urinary retention), endocrine disorders (stunting or gigantism, premature sexual development, hypothyroidism - decreased production of thyroid hormones, obesity), decreased academic performance school, etc.
Shunt System Components
The system consists of two catheters and one one-way valve. The ventricular catheter is located in the ventricle of the brain, and the peripheral (peritoneal or cardiac) catheter is placed in the abdominal cavity or in the right atrium, respectively. Both catheters are connected to a valve that regulates the unidirectional flow of cerebrospinal fluid. The valves are designed to operate in different pressure ranges (high, medium, low and very low). The neurosurgeon, having determined the patient’s intracranial pressure, selects the appropriate valve, depending on the severity of the disease, the patient’s age and clinical nuances.
Almost all valve models have a reservoir that your doctor can use to “bleed” the system to determine if it is working properly. From the reservoir, by inserting a thin needle through the skin, you can take samples of cerebrospinal fluid for laboratory tests or administer medications. Patients and their loved ones are not recommended to test the drainage system by “bleeding” the reservoir. This action can be dangerous unless your doctor has given you specific instructions about it. In patients suffering from non-communicating (obstructive) hydrocephalus, cerebrospinal fluid should be drained from the cerebral ventricle using a ventricular catheter. In patients with communicating hydrocephalus, a CSF drainage system is implanted from the lumbar space of the spine into the abdominal cavity - the lumboperitoneal system.
Causes of hydrocephalus in children
The causes of hydrocephalus are very diverse and largely depend on the age of the child.
- Hydrocephalus in the fetus. Modern types of prenatal diagnostics (for example, ultrasound examination) can detect hydrocephalus in an unborn baby. In most cases, it is caused by various malformations of the central nervous system (CNS). In 20%, dropsy is associated with intrauterine infections (cytomegaly, herpes, toxoplasmosis). When planning a pregnancy, parents should undergo testing for these infections, which often occur hidden, and treat them. This will avoid many problems with the baby's health. In rare cases, hydrocephalus is caused by genetic disorders.
- Hydrocephalus of newborns. Most often (up to 80%) dropsy in newborns is caused by malformations of the brain and spinal cord and the consequences of intrauterine infections. In approximately 20%, hydrocephalus is a consequence of birth trauma, especially in premature infants, which is accompanied by intracerebral or intraventricular hemorrhage and associated meningitis (inflammation of the meninges), which leads to impaired absorption of cerebrospinal fluid. It is extremely rare at this age that tumors and vascular malformations of the brain are detected, which can also cause the development of dropsy.
- Hydrocephalus in babies and older children (1-2 years and older). There are many reasons for the development of hydrocephalus in such children. These include tumors of the brain and spinal cord; consequences of meningitis, encephalitis (inflammation of the brain), various infectious diseases (for example, tuberculosis); malformations of the brain and cerebral vessels; consequences of hemorrhages; consequences of traumatic brain injury; genetic disorders. Sometimes the cause of hydrocephalus cannot be determined.
How is the diagnosis made?
Diagnosis of hydrocephalus is based on the clinical picture, examination of the fundus, as well as additional research methods, such as neurosonography (NSG), ultrasound examination of the brain (in infants under 2 years), computed tomography (CT) or magnetic resonance imaging (MRI) of the brain brain The primary diagnosis can be made by a neonatologist, pediatrician, neurologist or neurosurgeon.
The most common operation is ventriculoperitoneal shunt (VPS).
Neurosonography is an effective method for diagnosing the state of the brain and ventricular system in children under 1.5-2 years of age, until the large fontanelle and other “ultrasound windows” - areas of the skull where the bones are very thin (for example, the temporal bone) and transmit ultrasound. It allows you to detect expansion of the ventricular system, intracranial space-occupying formations (tumors, hematomas, cysts), and some malformations of the brain. However, it should be remembered that NSG is not an entirely accurate method. The image of the brain is obtained with significantly lower resolution (less clear) than with CT and MRI.
If any brain pathology is detected, a CT or MRI is necessary. Without them, it is impossible to make an accurate diagnosis, identify the cause of hydrocephalus, and even more so carry out treatment. This equipment is expensive and is still not installed in all hospitals. In this case, parents should insist on having a CT or MRI scan performed at other centers or perform them themselves on a commercial basis. It should be borne in mind that a clinic that undertakes the treatment of children with hydrocephalus is required to have this equipment. Otherwise, we can recommend that parents choose another, more equipped hospital, at least in another city.
Types of diagnostic tests
- Ultrasound is a simple, inexpensive test that helps evaluate the extent to which the ventricles of the brain are dilated. Currently, it is the simplest and safest method for diagnosing hydrocephalus.
- Computed tomography (CT) - This is a technique of drawing with a thin beam the contours of the skull, brain, ventricles and subarachnoid space. It is carried out to determine the size and shape of the ventricles and identify abnormalities such as tumors, cysts or other pathologies.
- Magnetic resonance (nuclear magnetic resonance NMR) is a non-surgical diagnostic method that uses radio signals and a magnet. MRI data determines the shape and severity of hydrocephalus. These studies are indispensable for clarifying the causes of dropsy.
- Cisternography (radiography of the cisterns at the base of the skull) is a test that requires the injection of a radioactive substance into the CSF. It is used to clarify the type of hydrocephalus: communicating or obstructive, as well as to determine the direction of CSF flow.
- Pneumoencephalography is now used much less frequently than in the past. In some cases, it is necessary to pump air with a needle into the spinal cord.
- Angiography (X-ray of blood vessels) is a special technique for injecting a contrast agent into the arteries that cross the brain. After some time, anomalies are detected at the level of blood vessels and the presence or absence of pathological disorders.
- A neuropsychological examination consists of a series of questions and answers to identify the presence of abnormalities in the functioning of the brain.
Treatment of hydrocephalus
Endoscopic ventriculostomy avoids foreign body implantation.
If a diagnosis of hydrocephalus (of any cause) is made, the child should be examined by a neurosurgeon. Most often, children with hydrocephalus are treated surgically, and the neurosurgeon determines the indications and contraindications for surgery. Observing children with hydrocephalus only by a neurologist or pediatrician without the participation of a neurosurgeon is a mistake and sometimes leads to an unreasonable delay in surgical intervention.
It is not easy for parents to decide whether to undergo surgery. However, a prolonged increase in intracranial pressure causes a delay in psychomotor development, which cannot always be compensated after unreasonably delayed surgical intervention. It should also be noted that the excessively large head of a child suffering from dropsy, even after the operation, will no longer return to its previous size - it will only be possible to stop its further growth. Literally, it will be difficult for the child to carry it on his shoulders, in addition, it will cause many cosmetic problems in the future. Parents of children with hydrocephalus should be aware that even if the neurologist does not refer them to a neurosurgeon, they should take the initiative and organize this consultation themselves.
The purpose of the operation is to divert cerebrospinal fluid from the ventricles of the brain to other cavities of the body. The most common operation is ventriculoperitoneal shunt (VPS). Through a system of silicone catheters, cerebrospinal fluid from the lateral ventricle of the brain flows into the abdominal cavity, where it is absorbed between the intestinal loops. The amount of flowing liquor is regulated by a special valve. Catheters are placed under the skin and are not visible from the outside. More than 200 thousand such operations are performed annually in the world. Bypass systems have saved millions of children's lives.
Less commonly, the cerebrospinal fluid is diverted into the right atrium (ventriculoatrial shunt), into the cistern magna (Torkildsen operation), or the spinal canal at the lumbar level is connected by a catheter to the abdominal cavity (lumbo-peritoneal shunt).
With the development of modern endoscopic technology (an endoscope is inserted into the cavities of the human body through small incisions, allowing them to be examined and manipulated), it has become possible to treat patients without installing a shunt system. Using an endoscope, a bypass path for the outflow of cerebrospinal fluid is created deep in the brain. This is a very effective operation (called endoscopic ventriculostomy), which avoids the implantation of a foreign body, such as a shunt system, and thereby prevents many complications. Unfortunately, this operation can only help a limited number of patients (about 10% of the total number of patients) with some forms of occlusive hydrocephalus. In other cases, it is necessary to install a shunt system, since there will be no improvement from endoscopic surgery.
A successful operation stops the progression of the disease. Most children have the opportunity to return to normal life and attend kindergarten and school along with healthy peers.
In some cases, patients with hydrocephalus are not operated on, but are monitored and take Diacarb (a drug that reduces the production of cerebrospinal fluid) for a more or less long period of time. This is done in cases where there are no obvious signs of disease progression and increased intracranial pressure. Observation is carried out under the strict supervision of a neurologist or neurosurgeon with frequent examinations, measurements of the child’s head circumference, repeated NSG or CT studies.
Advertising
Treatment
Currently, occlusive (obstructive) hydrocephalus is treated surgically. Surgical intervention consists of draining excess cerebrospinal fluid outside the cerebrospinal fluid system: into the abdominal (abdominal) cavity or into the atrium. Sometimes CSF may be drained into the pleural cavity. In these cavities, cerebrospinal fluid is absorbed and excreted along with waste products of the body.
To drain the CSF, the surgeon implants a drainage system (shunt). The system material is silicone and polypropylene. Both of these materials are well tolerated by the body. All elements of the system are implanted under the skin; there are no external areas.
Myths about increased intracranial pressure
The diagnosis of “increased intracranial pressure”, “intracranial hypertension (ICH)” or “hypertensive-hydrocephalic syndrome”, as already mentioned, is often made and in some cases - without reason. How does increased intracranial pressure (ICP) manifest? As already noted, in children under 2 years of age such manifestations are, first of all, accelerated growth of head circumference, bulging and enlarged fontanelle, possible eye movement disorders, and delayed psychomotor development. Most often, all these disorders manifest themselves in a complex. In children over 2 years of age, these are headaches with nausea and vomiting, more often in the morning, changes in the fundus of the eye (detected during examination by an ophthalmologist). Of course, the clinical picture may be different, but without the above symptoms, the diagnosis of “increased intracranial pressure” is doubtful.
This is how pediatrician Evgeniy Komarovsky describes the diagnosis of “increased intracranial pressure.” “Since the main symptom of hydrocephalus is a rapid increase in head size, measuring head circumference is included in the standards of any preventive examination, starting, of course, from the moment of birth. It is very important to emphasize here that it is not the specific size expressed in centimeters that matters, but rather the dynamics of this indicator. That is, stating the fact that the boy Petya at 3 months has a head circumference of as much as 45 cm is not at all a reason to become depressed and urgently save this boy. But the fact that the head circumference has grown by 7 cm over the past month is already alarming and dangerous, and requires both serious attitude and active control. Let me emphasize once again - not immediate treatment, but control. And if the trend continues, then measures should be taken.”
Symptoms such as sleep and behavior disorders, hyperactivity, attention deficit, bad habits, poor academic performance, hypertonicity in the legs, “marble” skin pattern, including on the head, nosebleeds, chin trembling, tiptoe walking, are not in themselves indicate increased intracranial pressure. And yet, some neurologists make a diagnosis of ICH based on these complaints. Neurosonography, having become a huge boon for pediatrics and neurology, has made a significant contribution to the excessive and false diagnosis of “hypertensive-hydrocephalic syndrome.” NSG makes it possible to quickly obtain an image of the brain substance and measure the size of the ventricles. However, to clarify the diagnosis, as we have already said, CT and MRI are mandatory.
Life after hydrocephalus shunt
The shunt remains in the patient's body for life. Brain shunt surgery has some disadvantages and side effects, but it is still widely used for hydrocephalus to treat and prevent the effects of increased intracranial pressure. The quality of life of patients after hydrocephalus shunting is significantly improved.
Neurosurgeons revise the shunt from time to time. This procedure is performed due to the child’s growth or disruption of the functioning of the shunt - its wear and tear, blockage. Modern shunts are designed for a ten-year service life. It is almost impossible to predict when a shunt will require replacement. Parents whose children have hydrocephalus and require shunting receive detailed instructions from the neurosurgeon on caring for the baby, signs of disruption of the normal operation of the shunt, and safety measures. If the shunt is blocked and the outflow of cerebrospinal fluid is disrupted, neurosurgeons provide patients with emergency qualified medical care.