External hydrocephalus of the brain is considered a disease of newborns, but the disease also occurs in adult patients. The development of hydrocephalus is caused by impaired absorption or outflow of cerebrospinal fluid. At the Yusupov Hospital, neurologists use modern diagnostic methods that make it possible to establish the causes, form of the disease and severity.
For mild hydrocephalus, conservative therapy is carried out aimed at reducing intracranial pressure and improving the function of nerve cells in the brain. Neurosurgeons at partner clinics perform surgical interventions that eliminate the cause of the disease. After surgery, patients’ quality of life improves and impaired nerve functions are restored.
Reasons for development
Acquired hydrocephalus can develop due to pathological processes that result in adhesions in the vessels of the brain and destruction of arachnoid villi. The disease is provoked by the following factors:
- Infectious diseases of the brain (encephalitis, meningitis, tuberculosis);
- Sepsis;
- Previous hemorrhagic stroke;
- Head, neck injury;
- Traumatic brain injuries;
- Traumatic spinal injuries;
- Malignant neoplasms of the brain stem.
Atrophic hydrocephalus occurs due to age-related changes in cerebral vessels, metabolic disorders, diabetes mellitus, and arterial hypertension. With external hydrocephalus, zones with reduced density of brain matter are formed. They atrophy, and the vacated space is filled with cerebrospinal fluid. The cause of the development of external hydrocephalus can be constant alcohol intoxication.
Hydrocephalus
Hydrocephalus in adults
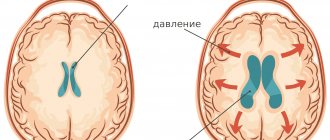
The accumulation of excess cerebrospinal fluid in a limited space of the cranium leads to increased intracranial pressure, which causes the most typical symptoms of hydrocephalus.
In adults and older children, these include: intense headache that cannot be relieved by analgesics, nausea, vomiting, and a feeling of pressure on the eyeballs. These symptoms may occur acutely or increase gradually, being transient at the onset of the disease. Atrophic hydrocephalus often occurs without signs of increased intracranial pressure and is detected only with additional examination of the patient. In most cases, hydrocephalus is accompanied by neurological symptoms, which are caused both by compression of brain structures by expanded cerebrospinal fluid spaces and by the underlying disease that causes the development of hydrocephalus. The most common symptoms of hydrocephalus are vestibular and visual disturbances. The first includes vestibular ataxia, manifested by dizziness, unsteady gait, noise in the ears and head, and nystagmus. On the visual side, there may be a significant decrease in visual acuity, loss of certain areas of the visual fields, congestive optic discs; with prolonged hydrocephalus, atrophy of the optic nerves may develop.
Hydrocephalus can occur with disturbances in the motor and sensory sphere: paresis and paralysis, increased tendon reflexes and muscle tone, decreased or complete loss of all types of sensitivity, and the formation of spastic contractures of the limbs. Occlusive hydrocephalus, caused by impaired circulation of cerebrospinal fluid in the posterior cranial fossa, is characterized by symptoms of cerebellar ataxia: impaired coordination and gait, large-scale disproportionate movements, changes in handwriting, etc.
In some cases, hydrocephalus is accompanied by mental disorders, which in adults are more often manifested by disorders of the emotional-volitional sphere: emotional instability, neurasthenia, causeless euphoria with a rapid transition to a state of indifference and apathy. With a sharp increase in intracranial pressure, aggressive behavior is possible.
Hydrocephalus in children
In children, due to the great flexibility of the skull bones, there is no increase in intracranial pressure; hydrocephalus in them is accompanied by an increase in the size of the skull. In newborns and young children, hydrocephalus is characterized by an overly large head size, bulging scalp veins, tension and lack of pulsation of the large fontanel, and swelling of the optic discs.
The symptom of “setting sun” is often noted - restriction of upward movements of the eyeballs. There may be dehiscence of the sutures of the skull. Tapping on the skull is accompanied by a characteristic sound (the “cracked pot” symptom). In children in the first year of life, hydrocephalus leads to developmental delays. They later begin to hold their head up, roll over, sit up and walk.
Children who have severe hydrocephalus are distinguished by a spherical shape of the head, its too large size, deep-set eyes, protruding ears, and thinning of the scalp. There may be decreased vision, increased muscle tone in the lower extremities, and disorders of the cranial nerves. Unlike adults, in childhood hydrocephalus is often accompanied not by emotional-volitional disorders, but by intellectual deficiency.
Children with hydrocephalus are usually sedentary and obese. They are apathetic, lack initiative, and do not have the attachment to relatives characteristic of their peers. A decrease in the degree of hydrocephalus often leads to an increase in the child’s intellectual abilities and activity.
In adolescence, hydrocephalus often occurs acutely against the background of an infectious disease, mental or physical trauma. At the same time, it is accompanied by intense headache, repeated vomiting, and bradycardia. There may be attacks of loss of consciousness, sometimes convulsive attacks. In some cases, episodic psychoses with hallucinatory or delusional syndrome are observed.
Development mechanism
With external hydrocephalus, cerebrospinal fluid accumulates outside the cerebral hemispheres, in the subarachnoid spaces. Excessive amounts of cerebrospinal fluid compress the cerebral cortex. External non-occlusive hydrocephalus of the brain occurs as a result of hypersecretion or malabsorption of cerebrospinal fluid. Closed (occlusive) hydrocephalus is a form of the disease in which the exit of cerebrospinal fluid from the ventricles is blocked by a tumor or adhesions.
Internal hydrocephalus can be congenital or acquired. Congenital hydrocephalus develops during intrauterine exposure to the fetus, acquired hydrocephalus develops during life. Mixed hydrocephalus is a separate form of the disease in which cerebrospinal fluid accumulates both in the ventricles and under the meninges.
Make an appointment
Causes of the disease
Hydrocephalus of the brain in adults and children is accompanied by obstructed outflow of cerebrospinal fluid, which serves to protect the brain and spinal cord, normalize blood pressure and metabolic processes. Causes of hydrocephalus include:
- mechanical damage to the skull;
- spread of acute and chronic infections;
- the occurrence of inflammatory processes in different parts of the brain;
- the presence of intracerebral tumor neoplasms;
- problems with the vascular system;
- hypertension;
- encephalopathy, etc.
Hydrocephalus syndrome can appear as a result of meningitis, stroke, diabetes, or tuberculosis. Disruption of cerebrospinal fluid circulation can be complete or partial, and problems with the movement of cerebrospinal fluid arise due to blockage of the lumens or adhesions.
Symptoms and severity
According to clinical manifestations, external hydrocephalus in an adult is divided into 3 degrees: mild, moderate and severe. With mild hydrocephalus, the body can independently restore the circulation of cerebrospinal fluid. The patient complains of slight malaise, headache, dizziness, and short-term darkening of the eyes. The average degree of hydrocephalus is manifested by intense signs of brain damage. Patients experience the following symptoms:
- Severe pain in the head, aggravated by physical activity;
- Pressing pain in the eyeballs, the appearance of colored circles of flashes when closing the eyes;
- Feeling of heaviness in the skull;
- Nausea independent of food intake;
- Vomiting without relief.
Sweating occurs periodically. An ophthalmological examination reveals swelling of the optic nerve head. Patients note swelling of the face, weakness, lethargy, and increased fatigue. They are worried about feeling tired in the morning, aggressiveness, increased nervousness, and tearfulness. A depressive state develops. Blood pressure is unstable. Unpleasant sensations intensify when coughing, sneezing, turning or tilting the head.
External hydrocephalus of the brain in an adult is accompanied by neurological symptoms:
- Decreased visual acuity;
- Strabismus;
- Impaired visual perception: double vision, blurred images;
- Paralysis or paresis of the limbs;
- Numbness of the face;
- Decreased sensitivity;
- Impaired coordination.
Patients have speech impairment, difficulty pronouncing sounds and perceiving spoken speech. With severe external hydrocephalus, epileptic and convulsive seizures, frequent fainting, and coma occur. The patient loses memory, intellectual abilities, and his self-care skills decrease.
Patients with occlusive hydrocephalus experience severe headache, nausea and vomiting in the morning. Congestion of the optic discs and signs of axial dislocation of the brain develop. An unfavorable prognostic sign is drowsiness. It intensifies on the eve of a sharp disruption of neurological symptoms. When brain structures are dislocated, cardiac activity and breathing are disrupted.
The clinical picture of chronic hydrocephalus consists of three pathognomonic symptoms: dementia, gait disturbance and urinary incontinence. Dementia is manifested by a decrease in the level of wakefulness, rapid exhaustion of the patient, disorientation in time, the development of severe intellectual disorders, and decreased criticism. Patients become unsure when walking and develop paresis of both lower extremities. The most recent symptom of hydrocephalus is urinary incontinence. This symptom of the disease is more common in men after 50-60 years of age.
Based on the intensity of the manifestation of hydrocephalus, a distinction is made between a moderate form of the disease, which occurs with minor symptoms, and a severe form - the accumulation of a large volume of cerebrospinal fluid provokes the manifestation of acute neurological symptoms.
Depending on the degree of impact on brain structures, external hydrocephalus can be compensated or decompensated. In the presence of compensated hydrocephalus, excessive secretion of cerebrospinal fluid does not affect the brain, but in the decompensated form of the pathological process, regardless of the amount of cerebrospinal fluid, brain function is disrupted and the functional activity of the central nervous system is reduced.
External non-occlusive hydrocephalus occurs when the process of cerebrospinal fluid absorption is disrupted. Atrophic (replacement) hydrocephalus develops most often in older people and is accompanied by the death of brain cells.
Symptoms of hydrocephalus of the brain
- attacks of intense headache;
- surges in blood pressure against the background of complete well-being;
- attacks of nausea, vomiting;
- episodes of urinary incontinence at night or during the day;
- changes in mental state (development of dementia);
- unsteady, shaky gait.
In children in infancy, there is a rapid increase in head size and bilateral paralysis of the extraocular muscles.
At the beginning of the disease, there are no neurological symptoms, although pathological changes in the brain are already occurring. Observed:
- cerebrovascular disorders;
- reduction of certain parts of the brain;
- organic changes in the cerebral substance.
Hydrocephalus of idiopathic origin is extremely rare.
To find out the causes and nature of the disease, detailed diagnostics using hardware technologies is necessary. Magnetic resonance imaging provides the most complete information about the state of the brain. The diagnosis of hydrocephalus is most often made in children under 3 months of age. Among the adult population, pathology is registered in patients over 60 years of age.
A list of the most common causes of hydrocephalus has been determined:
- tumors of various origins;
- traumatic brain injuries;
- diseases of the vascular system;
- conditions after neurosurgical interventions;
- acute cerebrovascular accidents - strokes;
- hematomas;
- congenital pathologies of the central nervous system.
The treatment program is drawn up by the doctor. It depends on the type of disease and severity. Uncomplicated forms of cerebral hydrocele can be treated with medication. If conservative therapy has shown its failure, and the disease causes a number of severe complications, neurosurgical treatment is performed. As a rule, operations are performed on an emergency basis.
Diagnostics
When a patient enters the neurology clinic, the doctor conducts an examination, checks motor reflexes, muscle and joint reactions. To clarify the diagnosis, additional examinations are carried out:
- Ultrasound examination of the head and neck for a preliminary assessment of the condition of the vascular bed;
- Computed tomography, which helps to establish the degree of damage to brain tissue, assess the degree of expansion of the subarachnoid fissures, determine the presence of neoplasms in the skull that impede the outflow of cerebrospinal fluid;
- Magnetic resonance imaging, which allows you to see changes in brain tissue with maximum accuracy;
- X-ray of the skull to determine changes characteristic of liquor hypertension and space-occupying formations;
- An ophthalmological examination to determine the presence of congestion, swelling of the optic nerve, and atrophy of eye tissue.
Patients undergo a lumbar puncture, which is used to determine the level of cerebrospinal fluid pressure. Improvement in the condition of a patient with hydrocephalus after removal of 40 ml of cerebrospinal fluid indicates a good prognosis after surgery.
Make an appointment
Causes of the disease
Any disturbances in the normal functioning of brain structures can lead to the development of the disease.
Causes of external hydrocephalus:
- Brain injuries;
- Consequences of injuries and spinal fractures;
- Tumors of any etiology;
- Stroke, hematoma, cerebral hemorrhage;
- Consequences of inflammatory processes or neuroinfections (meningitis, menigoencephalitis, tuberculosis, herpes, toxoplasmosis);
- Pathologies of the cervical vertebrae;
- Diseases of the circulatory system;
- Age-related changes in brain structures;
- Congenital anatomical changes of the central nervous system.
Signs
Moderate replacement hydrocephalus does not manifest itself with pronounced clinical symptoms. Neurologists at the Yusupov Hospital identify the disease using additional research methods. As the disease progresses, the pressure of excess cerebrospinal fluid on the brain substance increases, which leads to the following symptoms:
- intense headache developing into migraine;
- numbness of the upper or lower extremities;
- darkening of the eyes;
- impaired coordination of movements and gait;
- nausea and vomiting.
Patients develop a shuffling gait. They complain that their legs feel like they are stuck to the floor. An unfavorable prognostic symptom of replacement hydrocephalus is drowsiness. It increases on the eve of increased neurological symptoms and the development of a coma. Timely surgical intervention can stabilize the patient's condition.
Doctors at the Yusupov Hospital use modern methods for diagnosing hydrocephalus:
- ultrasound examination of cerebral vessels;
- computed or magnetic resonance imaging;
- craniography;
- cisternography;
- angiography.
After analyzing the examination results, doctors at the neurology clinic make a final diagnosis and treat the patient.