Neurologist
SEMENOVA
Olga
5 years experience
neurologist, head of the office for diagnostics and treatment of cognitive disorders
Make an appointment
A pathology characterized by an increase in the volume of fluid in the patient’s brain is called hydrocephalus. This condition increases the pressure inside the skull, causing a person to develop numerous brain disorders. The disease affects all age groups, from prenatal children to the elderly.
Basic information about pathology
A special cerebrospinal fluid, or cerebrospinal fluid, is produced in the choroid plexuses of the brain, called the ventricles, and fills the subarachnoid space. Excess cerebrospinal fluid is released into the bloodstream through the arachnoid membrane. When problems with absorption, circulation occur, or excessive secretion of cerebrospinal fluid occurs, hydrocephalus develops. It can be congenital or acquired as a result of certain diseases. In addition, the following forms of the disease are distinguished:
- internal hydrocephalus - overflow of one or more ventricles inside the brain with cerebrospinal fluid;
- external hydrocephalus - fluid injection between the brain and the enveloping subarachnoid membrane.
In its acute form, the disease develops over several days. Subacute course involves the development of decompensation within a month from the onset of the first symptoms, chronic - longer than six months. In addition, the classification of hydrocephalus includes stable and progressive forms of pathology, characterized, respectively, by stability or a gradual increase in pressure inside the skull.
Signs of the disease in adults
As a rule, hydrocephalus of the brain in an adult or a teenager is directly related to increased intracranial pressure, which causes the patient to feel:
- severe headache that does not improve with analgesics;
- feeling of internal pressure on the eyeballs;
- nausea, sometimes leading to vomiting;
- impaired coordination, due to which the gait becomes unstable, hand movements become sharp and sweeping, handwriting changes, etc.;
- tinnitus, impaired visual acuity, loss of certain areas of space from the field of vision.
Sometimes changes affect the patient’s emotional sphere, causing rapid changes in mood for no apparent reason, neurasthenic manifestations and unmotivated aggression.
Symptoms of a tumor of the IV ventricle
The clinical picture of tumors of the 4th ventricle consists of hydrocephalic-hypertensive syndrome and signs of damage to the cerebellum and brain stem. As the tumor grows, it closes the lumen of the 4th ventricle, which leads to the development of intracranial hypertension, which is manifested by a clinically pronounced headache accompanied by nausea or vomiting. Bruns syndrome is specific for tumors of the 4th ventricle. The development of this syndrome is due to the fact that the tumor disrupts the normal flow of cerebrospinal fluid. Clinically, the syndrome is manifested by severe headaches and dizziness that occur when the head or body is sharply turned, accompanied by rapid heartbeat, a feeling of fear and sweating of the skin. Often, at the height of the attack, patients experience loss of consciousness. During the non-attack period, the forced position of the head in patients attracts attention. Usually they tilt it slightly to the side or back, thus facilitating the outflow of cerebrospinal fluid. If the tumor affects the brain stem structures, then corresponding symptoms appear (asymmetry of the facial muscles, various speech disorders, swallowing disorders, weakness in the limbs, hearing impairment, vision impairment, strabismus, etc.). If the tumor begins to compress the cerebellum, the patient experiences various clinical symptoms of impaired coordination of movement and balance. These include a shaky gait, trembling limbs, and decreased accuracy of movements.
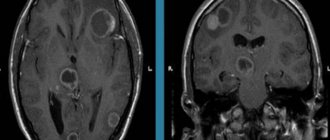
Diagnostics
To diagnose tumors of the 4th ventricle of the brain, various hardware techniques are used, most often MRI, CT and PET of brain structures. Using MRI or CT of the brain, the size of the tumor is determined, its location and the relationship of the tumor with other structures of the brain are clarified. These diagnostic methods also make it possible to identify the presence of hydrocephalus in a patient and assess its severity. When performing a PET scan, the doctor can assess the degree of metabolic processes occurring in the tumor, which allows one to determine the degree of its malignancy.
Treatment
Tumors of the 4th ventricle can only be treated surgically. The choice of surgical method depends on the characteristics of the disease. Thus, with severe hydrocephalus, sometimes a shunt operation is initially performed, which leads to a decrease in the severity of hydrocephalus. In some patients, even after complete removal of the fourth ventricle tumor, signs of hydrocephalus remain, which requires additional surgical intervention. For malignant tumors of the 4th ventricle, surgical treatment is supplemented with radiation or chemotherapy.
Ependymoma is a neuroepithelial tumor belonging to the subgroup of ependymal gliomas. This type of tumor develops from ependymal cells lining the ventricular system of the brain and the central canal of the spinal cord. Most often these are tumors of the lateral and fourth ventricles. There are benign and malignant ependymomas. Benign ones include subependymoma (GRADE I WHO), myxopapillary ependymoma (GRADE I WHO), ependymoma (GRADE II WHO). Malignant ependymomas include anaplastic ependymoma (GRADE III WHO). In some cases, with an increase in tumor volume, a blockage of the brain ventricles and liquor pathways occurs, which leads to the development of hydrocephalus. Ependymomas can metastasize within the central nervous system along the cerebrospinal fluid pathways of the brain and spinal cord.
Signs in children
Thanks to the mobility of the cranial bones, children, especially newborns and toddlers in the first years of life, do not experience an excessive increase in pressure inside the skull. Manifestations of hydrocephalus of the brain in a child are:
- enlarged head;
- bulging fontanelle without pulsation (in children in the first months of life);
- bulging veins on the head;
- limited mobility of the eyeballs when moving upward;
- expansion of cranial sutures.
With the congenital development of the disease or the appearance of pathology in newborns, the child almost always lags behind his peers in his development: later he begins to hold his head up, sit up, and reacts poorly to attempts to communicate.
In children with severe pathology, characteristic external signs of hydrocephalus develop: a large spherical head with thin skin, deep-set eyes, protruding ears. Such children are characterized by inactivity, which is why they often suffer from obesity. Almost always, the disease leads to intellectual and emotional deficiency: children grow up lethargic, lack initiative, and do not experience attachment to relatives.
Are you experiencing symptoms of hydrocephalus?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
MORPHOLOGY OF TUMORS OF THE III VENTRICLE
The morphology of tumors of the third ventricle is different. In the anterior parts of the ventricle, colloid cysts are more often observed, which are classified as dysembryogenetic neoplasms. Previously it was believed that they are derivatives of the neuroectoderm (paraphysis - an embryonic structure that is a pocket between the telencephalon and the anterior parts of the midbrain), but more data indicate their endodermal origin. They have an epithelial lining and characteristic mucous contents and are more common in adults. Macroscopically, colloid cysts are round or oval-shaped formations, the diameter of which ranges from 0.3 to 4 cm. The cyst has a dense capsule with a smooth wall and viscous contents of a greenish-gray color. Recently, their endodermal origin has been established.
Ependymomas arise from the inner lining of the ventricles of the brain and account for 5–10% of all tumors of the central nervous system. Of these, 2/3 arise in the posterior cranial fossa, 10% in the spinal canal and the rest supratentorially in the lateral and third ventricles. Within the third ventricle, ependymal tumors are predominantly localized in its posterior sections; macroscopically they have the appearance of a node with a predominant localization in the ventricular cavity. They are well demarcated from the brain, but in some areas they grow into the medulla. The depth of germination depends on the malignancy. Ependymomas have well-visualized borders, and therefore their complete removal is possible. Implantation metastases of malignant ependymomas are rare. According to RI Ernestus (1996), in children the frequency of ependymomas is 18.6%, less than astrocytomas and medulloblastomas (sex ratio 6:5 with a predominance of men).
In the pineal region there are: germ cell tumors - germinoma, teratoma (or epidermoid, dermoid), teratoma with malignant transformation, embryonal carcinoma, endodermal sinus tumor, choroid carcinoma and mixed germ cell tumors; tumors from the pineal parenchyma - pinealoma, pineocytoma, pineoblastoma; gliomas and tumors from the velum interpositum - meningiomas, hemangiopericytomas, angiomas, cysts, less often - pineocytomas.
Pinealomas and germinomas, according to the same author, could be located in the suprasellar-hypothalamic region and in other sections. Pineoblastomas have an invasive growth pattern, often metastasize and are close to medulloblastomas in their histological structure and degree of malignancy. Pinealocytomas are well-circumscribed benign tumors that often have a capsule and cysts. Choroid carcinomas and yolk sac tumors look like large infiltrating formations that early disseminate along the spinal canal and in 10% of cases metastasize beyond the central nervous system (to bones, lungs, lymph nodes).
Meningioma is a very rare neoplasm of this area, especially in childhood. Their frequency is 1.5 – 2.5%.
Craniopharyngiomas localized in this area are often cystic, located in the cavity of the third ventricle, penetrate into the lateral ventricles, extraventricularly and often reach gigantic sizes. In the world literature, there is one report on the diagnosis of craniopharyngioma of the pineal region, accidentally discovered at autopsy in a 58-year-old woman who died in a fire, and a second observation in our clinic. Germinomas originate from embryonic cells, 20% of them are located in the suprasellar region, involve the floor and walls of the third ventricle, and may primarily originate from the basal ganglia. Germinomas can metastasize to the walls of the ventricles and basal cisterns.
According to the histological structure of the tumor of the bottom of the third ventricle, almost all are astrocytomas, most often low-grade juvenile pilocytic and sometimes fibrillary astrocytomas. Our data support this statement. Astrocytomas of this localization are benign neuroectodermal tumors, the histological structure of which does not change in most cases over many years of growth before and after surgical interventions. Macroscopically, astrocytomas in most cases are poorly demarcated from the surrounding tissue and are homogeneous. Pilocytic astrocytomas have the appearance of a grayish nodule. The boundaries of the tumor are quite clear, and cysts are often found. Pilocytic astrocytomas have many papillae, and tumors with severe angiomatosis are sometimes found.
Hypothalamic hamartomas are rightfully classified as developmental defects, located between the pituitary infundibulum and the mamillary bodies, and histologically consist of tissue similar to the hypothalamus. There are hormonally active and hormonally inactive forms.
Choroid papillomas make up less than 1% (0.65% according to our data) of all intracranial tumors, and only less than 10% of them are localized in the third ventricle. Most often, these tumors arise as functioning intraventricular papillomas of the roof of the third ventricle, secreting cerebrospinal fluid. Tumors of the choroid plexus have a fairly slow growth rate and reach a large size. Macroscopically, they have the appearance of a node with a finely granular lobulated surface (cauliflower-like appearance), dark red in color, dense consistency, with a predominant localization in the lumen of the ventricle. Choroid plexus carcinoma is a more aggressive tumor, accounting for 10–20% of all choroid plexus tumors. It is rightly believed that choroid carcinomas can invade the medulla over a large area. This tumor is characterized by features characteristic of anaplastic tumors and has a tendency to diffuse extracranial spread. Although choroid plexus papillomas can spread beyond the skull, their deposits are benign and, as a rule, asymptomatic. Choroid carcinomas tend to form implantation metastases, which usually become clinically apparent during the first months after surgery.
There are reports in the literature of 23 cavernous malformations of the third ventricle.
Hemangioblastomas, metastatic medulloblastomas, glioblastomas, and epidermoid cysts can also be found in the third ventricle.
What causes the disease?
There are many factors that influence the mechanism of cerebrospinal fluid circulation, and they are different for intrauterine development and for acquired forms of pathology.
The causes of congenital hydrocephalus include:
- deviations in the formation of the brain’s liquor system;
- structural defects of the subarachnoid space;
- anomalies of the craniovertebral region;
- influence of intrauterine infections;
- birth injuries.
In cases of acquired hydrocephalus, the causes of impaired circulation of cerebrospinal fluid differ sharply. This:
- infectious inflammation of the tissue and membranes of the brain;
- traumatic brain injury;
- pathological processes in the vessels of the brain (strokes, hemorrhages, hematomas);
- intracerebral tumors, ventricular cysts.
Sometimes there is an atrophic form of the disease, which develops as a result of age-related or traumatic atrophy of brain tissue due to cerebrovascular accidents.
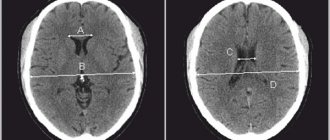
How is it diagnosed?
As a rule, diagnosing hydrocephalus is not difficult: the doctor determines the presence of pathology during the first examination. However, to identify the causes of the development of the disease, the nature and extent of the damage, instrumental studies may be needed:
- X-ray of the skull;
- tomography (computer or magnetic resonance imaging);
- echography;
- lumbar puncture and subsequent examination of the cerebrospinal fluid.
In addition, ophthalmic examinations may be necessary to evaluate visual impairment.
How are they treated?
Depending on the etiology and severity of the disease, conservative or surgical treatment of hydrocephalus may be chosen. Conservative therapy is most effective in cases of development of disorders due to inflammation, injury or minor hemorrhage and consists in eliminating the cause of the disease. To reduce intracranial pressure and alleviate the patient's condition, diuretic drugs are prescribed.
Surgical intervention is indicated for congenital pathologies to correct developmental defects, as well as in the presence of volumetric processes - large intracranial hematomas, tumors, abscesses, etc. In cases where the cause cannot be eliminated either by conservative treatment or surgical removal, the neurosurgeon prescribes shunt surgery and creates additional pathways for the outflow of excess cerebrospinal fluid.
CLINICAL MANIFESTATIONS OF TUMORS OF THE III VENTRICLE
Clinical diagnosis of tumors of the third ventricle is extremely difficult due to the presence in the clinical picture of the disease of very sparse focal symptoms and the development of almost only general cerebral symptoms (hydrocephalic-hypertensive phenomena, headaches, congestive optic discs).
In 1910, the first generalized work on tumors of the third ventricle appeared, in which Weisenburg analyzed 30 observations (27 from the literature and 3 of his own, of which 5 were children). And he comes to the conclusion that there are no specific symptoms for tumors of the third ventricle, and the diagnosis in all cases was established at autopsy. The most significant work on this problem was the monograph by W. Dandy, published in 1933, in which the author, based on 68 observations (21 his own and 47 literary ones), analyzes the clinical course and methods of surgical removal of tumors of the third ventricle.
It is generally accepted that tumors of the third ventricle are asymptomatic for a long time and only as they grow and fill the cavity of the third ventricle, compression of paraventricular formations creates occlusion of the cerebrospinal fluid pathways and manifests characteristic clinical symptoms. Although the clinical picture of tumors of the third ventricle depends on the localization of the tumor within the ventricle, the leading clinical picture of the disease is the syndrome of intracranial hypertension. And the onset of the disease in most cases is characterized by the appearance of general cerebral symptoms (paroxysmal headaches, vomiting, congestion in the fundus), which in most cases remain leading in the clinical picture of the disease.
Features of the clinical course depend on the starting point of tumor growth, its direction, the degree of occlusion of the cerebrospinal fluid pathways and the effect of the tumor on the formations of the third ventricle, as well as on the paraventricular and stem parts of the brain. Craniobasal symptoms of damage to the cranial nerves are caused by hydrocephalic stretching of the lateral and third ventricles with pressing of the cranial nerves to the bones of the base of the skull and large vessels of the base of the brain. Chronic basal arachnoiditis, often accompanying tumors of the third ventricle, is also sometimes the cause of damage to individual cranial nerves.
To a certain extent, the clinical picture of tumors of the third ventricle depends on the location of the tumor within the ventricle; however, many similarities can be noted for the entire group of these neoplasms. They are characterized by intracranial hypertension syndrome. The onset of the disease with tumors of the third ventricle is largely characterized by the appearance of general cerebral symptoms (headaches, vomiting, congestive optic discs), which in most cases remain leading in the clinical picture of the disease. Meningeal symptoms caused by tonic reflexes are observed quite often. Characteristic is the dissociation between constant and severe Kernig's sign with weak neck rigidity. Some authors note a forced position of the head or torso, which appears later in the disease, especially during attacks of headaches. We did not encounter any manifestations of a disease of this nature in our material.
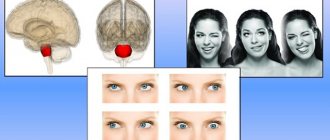
Characteristic of tumors of the posterior sections of the third ventricle is a combination of hypertensive and quadrigeminal syndromes. The first and leading symptoms in this category of patients are symptoms of intracranial hypertension with the early development of occlusive hydrocephalus. Pathognomonic for tumors of the posterior sections of the third stomach and pineal region is the quadrigeminal syndrome, observed in 50–87% of cases. Often these tumors present with cerebellar symptoms, indicating caudal spread of the tumor. There are also endocrine disorders, which are most often represented by the syndrome of premature sexual development.
The clinical picture of tumors of the third ventricle bottom consists of endocrine hypothalamic disorders, chiasm lesions, hypertension syndrome and sella turcica lesions. The first signs of the disease can be either these symptoms alone or in combination, or they can vary significantly. With craniopharyngiomas of the third ventricle, there is a decrease in visual acuity, hypothalamic-pituitary disorders, adiposogenital syndrome, growth retardation, diabetes insipidus, sleep disturbance, etc. With gliomas of the visual pathways, ophthalmological symptoms come to the fore (decreased visual acuity, nystagmus, exophthalmos 43 – 88 %), endocrine and metabolic disorders (growth retardation, premature sexual development, diabetes insipidus, 20 - 26%), hypertensive headaches (15 - 28%), even less often - convulsive syndrome, mental disorders, paresis, (5 - 10% ), and association with neurofibromatosis (13 – 29%). Hypthalamic hamartomas, divided into two types according to MRI (parahypothalamic and intrahypothalamic), are characterized by symptoms of precocious puberty in parahypothalamic and difficult to treat seizures with mental retardation and behavioral disorders in intrahypothalamic hamartoma.
The main manifestations of the disease in tumors of the anterior sections of the third ventricle are symptoms characteristic of occlusion of the cerebrospinal fluid tract (symptoms of intracranial hypertension), in the form of increasing intensity headaches, vomiting, congestion in the fundus, and in some patients - hypertensive crises, which can be extremely difficult and even cause death. Colloid cysts are characterized by a long course of the disease and a slow increase in their volume.
All the variety of clinical symptoms in primary tumors of the third ventricle V.A. Legkonogov (1973) reduced it to the following syndromes: hydrocephalic-hypertensive, paroxysmal, periventricular, mesos- and rhombencephalic and the syndrome of mental disorders.
The dynamics of the development of clinical symptoms may indicate the initial location of tumor growth. If, for example, the disease begins with the appearance of quadrigeminal syndrome, then we can assume that the tumor comes from the pineal region, if from ophthalmological symptoms, then we can assume that the site of initial growth of the tumor was the chiasm itself. In cases where the disease manifests itself as diencephalic and endocrine metabolic disorders, it can be assumed that the tumor primarily arose in the bottom of the third ventricle.
As the tumor grows and fills the cavity of the third ventricle, the clinical picture of the disease may reveal motor and sensory disturbances, cerebellar and brainstem symptoms. With tumors of the third ventricle, certain mental disorders associated with increased intracranial pressure and tumor localization may be observed. Although typical epileptic seizures do not occur with tumors of the third ventricle. Occasionally, epileptic seizures develop, which are more often observed with neoplasms arising from the bottom of the third ventricle. They are manifested by loss of consciousness or accompanied by tonic convulsions (diencephalic seizures). W. Dandy (1933) calls these seizures “intermittent seizures.” Characteristic components of the attacks were phenomena of sensory irritation or vasomotor disturbances (chill-like tremors in the form of short-term paroxysms, profuse sweating, increased body temperature to 38 - 390 degrees).
The duration of the disease from the appearance of the first symptoms to admission to the clinic ranges from several days to 15 years.
Y. Sawamura et. al. (1995) reports on asymptomatic cysts of the pineal region in women with a peak at the age of 21 - 30 years, measuring >5 mm, accidentally detected during MRI of the brain, and at autopsy the frequency of such cysts reached 25 - 40%.