More useful information about other diseases starting with the letter “K” here: Causalgia, Brain cyst, Cluster headache, Tick-borne encephalitis, Kozhevnikov epilepsy, Colloid cyst of the third ventricle, Coma, Compressive myelopathy, Balo concentric sclerosis, Radicular syndrome, Corticobasal degeneration, Craniovertebral anomalies, Craniospinal tumor, Craniopharyngioma, Myasthenia gravis crises, Hemorrhage into the ventricles of the brain.
What does hemorrhage into the ventricles of the brain mean?
Hemorrhage into the ventricles of the brain is a disease that is one of the forms of malfunction of the circulatory system of the brain. The presented disease is most often diagnosed in modern medicine. Neurologists say that the disease is caused by arterial hypertension (the treatment of which has been neglected for a long time), bad habits (smoking, alcoholic beverages, drugs) and the use of pharmacological agents that can lead to poor blood clotting. To establish a conclusion, the doctor conducts a detailed conversation with the patient, finds out existing complaints and problems, and also prescribes a certain list of tests for a final affirmative diagnosis. Therapeutic treatment helps eliminate the formed edema, stabilize lung function and normalize blood pressure.
Consequences of ventricular bleeding
The main complications are caused by an increase in brain volume, necrotic changes in tissue in the area of acute cerebrovascular accident.
Main complications of IVH:
- Psychomotor development disorders;
- Increased intracranial pressure;
- Swelling and compression of the cerebral cortex;
- Intracerebral hematomas;
- Extensive convulsive seizures;
- Periventricular leukomalacia;
- Cortical atrophy;
- Decline in motor activity.
Ultrasound allows us to determine the list of complications in newborns. Computed tomography (CT of the vessels of the head with contrast) is accompanied by tissue irradiation, which does not allow the examination to be used without indications.
Occlusive hydrocephalus and cerebral hydrocephalus are long-term complications of the nosological form with a high probability of death.
Brief information
In neurology, a similar disease of hemorrhagic type is classified as stroke. The anomaly has different names. According to surveys and average statistical information received from practicing doctors, the described deviation from the norm ranks first in the number of deaths of patients around the globe. Based on publicly available information, such a process can cause death within 48 hours of onset in 60% of cases. The risk increases significantly during the recovery period after a stroke. People who survive a critical attack have a 90% chance of bleeding.
Basically, the largest number of recorded pathologies is observed in the population of retirement age, whose age has exceeded the mark of 50 years. However, in addition to this, danger threatens not only people with arterial hypertension, but also any other abnormalities that have absolutely nothing to do with the level of pressure.
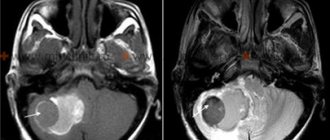
Hemorrhagic stroke diagnosis.
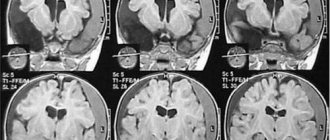
Computed tomography is the “gold standard” for diagnosing acute cerebral hemorrhage.
On MRI, hemorrhage in the acute period may not be visible.
CT scans evaluate the volume of the hematoma, its location, swelling, displacement of the midline structures and relationship to the ventricles, which is very important for choosing treatment tactics.
CT scan of a large mixed hematoma. Putamenal hematoma. Ischemic stroke with hemorrhagic transformation.
Additional diagnostic methods:
- CT angiography allows you to view vessels in 3D mode to exclude aneurysms and malformations.
- Magnetic resonance imaging to determine hematomas in the subacute period (from 3 to 14 days), as well as brain tumors, cavernomas and other formations.
- Selective cerebral angiography is necessary for a more thorough diagnosis of arterial aneurysms and vascular malformations.
As for the need to perform a lumbar puncture, there is no reason for this manipulation if a computed tomography scan is done. It is advisable to puncture only to exclude postoperative meningitis, if such a suspicion exists.
Types of hemorrhage
The compilation of classes of the described disease was created in the late 90s, as a result of which the list was included in international medical documents on the classification of diseases. Based on the source in the form of ICD-10, the presented pathological process is divided into several forms:
- Subependymal (SEC).
- SEC with damage to the extreme parts.
- SEC with progression to areas and substance of the brain.
In addition, there are additional differences between IVH, which differ in location:
- Changes in the lateral structures - begins from nearby soft cavities and manifests itself as a gradual filling of the entire volume with further leakage into other areas. In the case of the formation of a surplus, the size of the main organ begins to increase, as a result of which symptoms of a neurological nature progress (if only one object is filled, the specialists’ prognosis is positive, since this process is similar to a parenchymal disorder).
- Location in the third ventricle - the medial zones of parenchymal disorders become the culprit.
- The focus of inflammation in the 4th lobe originates from the dorsal perimeter of the brainstem or cerebellum.
Hemorrhagic stroke types.
| Primary | Against the background of arterial hypertension, it occurs more often. |
| Secondary | Against the background of blood pathology (thrombocytopenia, coagulopathy), brain tumors, ruptures of arterial aneurysms and vascular malformations, vascular pathology (angiopathy, arteritis). |
According to the mechanism of development, hemorrhage into the brain substance occurs as a hematoma and as an impregnation. Hematomas are more common and are associated with the fact that after a rupture of the vascular wall, spilled blood pushes the brain substance apart, forming blood clots. Impregnation is less common and occurs due to ischemia and increased permeability of the vessel wall to blood.
Depending on their location, intracerebral hematomas are:
- putamenal or lateral – located in the internal capsule or lateral to it, most often (55% of all cases);
- thalamic or medial - located medially from the internal capsule or in the area of the thalamus, found in 10% of cases;
- mixed - cover both the thalamus and the internal capsule;
- subcortical or lobar - located near the cerebral cortex within one lobe, found in 15% of cases;
- brain stem – most often located in the pons (10% of cases);
- cerebellum - occur in 10% of cases.
With medial and mixed hematomas, there is a breakthrough of blood into the ventricles of the brain with the formation of parenchymal-ventricular hemorrhage.
(c) Can Stock Photo Thus, hemorrhage occurs in the area of the internal capsule and thalamus.
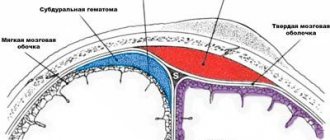
Spontaneous hemorrhage under the membranes of the brain:
- subdural (under the dura mater) - occurs against the background of coagulopathy, uncontrolled use of anticoagulants, for example, Warfarin (with INR <3.0) and rupture of an arterial aneurysm;
- subarachnoid (under the arachnoid membrane) - occurs more often against the background of a ruptured arterial aneurysm.
Intraventricular hemorrhage is distinguished separately. It can occur with all forms of intracranial hemorrhage, but is more common with ruptured aneurysms, especially the anterior communicating artery.
Main factors of appearance and symptoms
There are two stages of bleeding - primary and secondary. PIH is associated with arterial problems in the body or amyloidosis in the cerebral vessels, so they are diagnosed in rare situations. Based on some data, such an anomaly occurs once in 300 patients. The second version of FFM is formed due to the incorrect use of certain medications (for example, antiplatelet substances or fibrinolytic drugs), the presence of a neoplasm capable of breakthrough, or cancerous tumors.
With such an illness, the patient experiences a rapid increase in depression of thinking. Usually, a coma appears after a stroke in the first hours. Only with a gradual progression of the disease and, most importantly, a minimum amount of fluid released, the consciousness of the individual remains stable for a long time and decreases gradually.
Often, bleeding occurs along with:
- meningeal manifestations and gag reflexes.
- Extreme sweating.
- Trembling, similar in nature to chills.
- Change in skin color.
- Abnormal accumulations of blood cells in the vascular ducts, occurring in the face, torso, arms and legs.
- An initial decrease in body temperature, and as a result a rapid jump reaching above 40 degrees.
A typical symptom of such a disorder in the body is a decrease in the tone of muscle tissue, which manifests itself in the form of hormetonic syndrome or an irreversible stage of coma. In the first method, an attack of increased muscle activity in the inflamed area begins. This symptom appears due to external conditions. In the second, deformations develop exclusively in the extensor layers. The patient takes a supine position and arches his back, while tilting his head. The upper limbs are clasped and the forearms are facing inward. Also, it may be accompanied by paresis in the opposite extremities from the pathology, the formation of reflexes in the tendons, the presence of anomalies and lack of action in the abdominal region, disruption of the performance of the pelvic region and its organs.
During the disease, which is localized in the third compartment, difficulties arise in breathing and in the functioning of the circulatory system, and hormetonia syndrome has a bilateral effect. With a deviation located in the fourth ventricle, hiccups and problems with swallowing saliva are caused, uncontrolled movements are not observed, and signs of hormetonia are less noticeable. If the described process continues for a long time in a patient, then an increase in the amount of fluid begins, which provokes an increase in VD, swelling and compression of the nerve areas responsible for the life support of the entire body. The supplement favors disorders of the heart and vascular system.
Intracerebral hematomas
Intracerebral hematomas , in addition to etiology, are divided by location and volume. In the vast majority of cases (up to 90%), hematomas are localized in the supratentorial regions of the brain.
CLINICAL PICTURE
The clinical picture of intracerebral hemorrhage is quite typical. The disease has an acute, sudden onset, often accompanied by high blood pressure. Characterized by severe headache, dizziness, nausea and vomiting, rapid development of focal symptoms, followed by a progressive decrease in the level of wakefulness - from moderate stupor to a coma. Depression of consciousness may be preceded by a short period of psychomotor agitation. Subcortical hemorrhages can begin with an epileptiform seizure.
SYMPTOMS
Focal neurological symptoms depend on the location of the hematoma. Typical focal symptoms, taking into account the most common localization of intracerebral hematomas, are hemiparesis, speech and sensitivity disorders, frontal symptoms in the form of memory impairment, criticism, and behavior. The severity of the patient's condition immediately after the hemorrhage and in the following days depends primarily on the severity of cerebral and dislocation symptoms, in turn determined by the volume of the intracerebral hematoma and its location. With extensive hemorrhages and hemorrhages of deep localization, secondary brain stem symptoms due to brain dislocation appear quite quickly in the clinical picture. Hemorrhages in the brain stem and extensive cerebellar hematomas are characterized by rapid impairment of consciousness and vital functions. The most severe hemorrhages occur with a breakthrough into the ventricular system. They are characterized by the appearance of hormetonic convulsions, hyperthermia, meningeal symptoms, rapid depression of consciousness, and the development of brainstem symptoms.
The severity of focal symptoms in parenchymal hemorrhages depends mainly on the location of the hematoma. Small hematomas in the area of the internal capsule can lead to a much more severe focal syndrome than larger hematomas located in functionally less significant parts of the brain.
TREATMENT
Treatment should be carried out exclusively by a neurologist. Self-medication is unacceptable. Treatment of patients with intracerebral hematoma can be conservative and surgical. The question of treatment tactics must be decided based on the results of a comprehensive clinical and instrumental assessment of the patient and a mandatory consultation with a neurosurgeon.
Diagnostic techniques
To establish a correct conclusion, experts will need to conduct an evaluative check of the person’s medical history, that is, find out the presence of blood diseases, previous hemorrhagic strokes, what medications the patient took that contributed to poor clotting, etc. In addition, doctors conduct a standard examination and prescribe additional tests to create a full picture.
You need to understand that if an anomaly is likely to develop, you should urgently go to the nearest medical center to provide professional clinical care. Also, experts do not exclude the possibility that the patient will have to undergo resuscitation measures on the way to the hospital. In the inpatient building, doctors write out directions for the following procedures:
- MRI scan or computed tomogram, depending on the presence of contraindications.
- Donation of blood cells for analysis, during which there will be a report on the number of platelets in the body.
- Coagulogram examination.
- Electrocardiogram.
- Check blood pressure readings.
If doctors do not have the opportunity to perform magnetic resonance or computer diagnostics on a person due to a coma, then echo-encephalography is prescribed. At certain points, it may be necessary to perform a lumbar puncture in order to distinguish hemorrhage, which provokes the entry of fluid into the spinal substance, from an ischemic stroke.
Causes of cerebral hemorrhage in adults
There are many reasons why blood vessels rupture and blood spills into the brain tissue. Among the most common are:
- arterial aneurysms (thinning of the wall, the formation of a sac with blood that overflows and bursts);
- vascular malformations (birth defects, thinning, tortuosity of the walls);
- ruptures of blood vessels during a hypertensive crisis due to the prohibitive load on the walls;
- head injuries with vascular ruptures;
- tumors that grow and damage arteries;
- taking blood thinning medications (if dosages are not followed);
- the development of certain systemic diseases in which the walls of the arteries are affected (for example, amyloidosis).
At a young age, the leading causes of hemorrhage are injuries and congenital vascular anomalies. In the elderly – damage to blood vessels by atherosclerosis and their rupture due to hypertension, tumor processes.
Treatment Options
The first point for medical staff is the prompt provision of first emergency aid and the immediate implementation of basic level treatment - stabilization of the functions of the heart and lungs, as well as monitoring of blood pressure levels and regulation of the constant flow of internal processes of the body.
In addition, doctors prescribe therapy to get rid of symptoms: intravenous injections that have an anticonvulsant effect, as well as help resolve swelling and normalize blood pressure (in addition, a drug can be used to stop vomiting). To fully stop bleeding, a treatment plan is currently being developed by the most qualified scientists. The pathogenic option involves maintaining optimal blood pressure levels and pumping out excess blood through surgery. Such procedures include:
- The use of agents that have a neurotrophic effect and increase metabolism.
- Taking antioxidants (including vitamin E) and substances that block calcium ducts.
The surgical procedure is selected on an individual basis.
Causes of acute cerebrovascular accidents.
Risk factors:
- high blood pressure;
- alcoholism;
- previously held acute medical complications (of any type);
- liver dysfunction, leading to a decrease in the number of platelets and clotting factors in the blood;
- pathology of cerebral vessels (angiopathy, arteritis);
- poorly controlled use of anticoagulants, such as Warfarin (with INR <3.0).
Smoking is not a risk factor for this disease, but is a risk factor for ischemic stroke.
(c) Can Stock Photo
In addition, acute hemorrhagic stroke can be a complication of thrombolysis during ischemic stroke or after brain surgery.
Separately, it is worth highlighting physical factors:
- heavy physical activity;
- hypothermia;
- overheat.
The literature has documented cases of acute cerebral hemorrhage due to neuroinfection, thrombosis of the venous sinuses, and eclampsia.
In rare cases, hemorrhages into the internal capsule are possible after a migraine attack.