Cerebral angioma is a vascular tumor that can develop in any part of the brain, including the cerebral cortex, brainstem and cerebellum, but is more often found in the hemispheres. This is a benign tumor, which nevertheless can pose a serious health hazard and increase the risk of developing cerebral hemorrhages. If you are diagnosed with cerebral angioma, treatment in Germany allows you to get rid of the problem using the latest medical technologies.
The most common are cavernous angiomas (cavernomas). These are neoplasms, inside of which there are cavities separated from each other by partitions and filled with blood. As a rule, angiomas arise as a developmental defect, but they can appear later. There are also venous angiomas, which are less dangerous.
Symptoms of cavernous angioma
The patient may have no symptoms, although headaches, seizures, or other focal symptoms, such as motor or sensory disturbances, are common. Most often, the occurrence of symptoms is associated with hemorrhages, which can occur both inside the cavernous angioma and in the surrounding brain tissue. Depending on the severity of the hemorrhage, conservative treatment or surgical intervention is used, which will be discussed below.
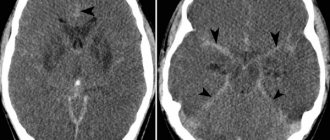
Cavernous angioma of the right frontal lobe. A CT scan without contrast enhancement shows a large heterogeneous mass in the right frontal lobe. The formation is characterized by high X-ray density in its central part and diffusely increased density in the periphery due to the presence of calcifications and small hemorrhages in the formation.
Brain angioma treatment in Germany: radiosurgery
Radiation as a treatment method is used if the tumor is located in hard-to-reach areas or when removing it there is a risk of affecting important areas of the brain. As a rule, the radiosurgical method is used for formations up to 1 centimeter.
A gamma knife is used for radiosurgical treatment. The required effect of treatment may occur in 4-5 months or several years.
The doctor must determine which treatment method is optimal. A qualified neurosurgeon will select a technique based on the situation and health status.
Vascular malformations of the brain
Types of vascular malformations differ based on their macroscopic and microscopic characteristics. Typically, intracranial vascular malformations are divided into the following 4 groups:
- Capillary malformations (or telangiectasias)
- Cavernous malformations (cavernous angiomas/hemangiomas)
- Venous malformations
- Malformations with arteriovenous shunts
According to the newer classification, 2 more categories have been added: arterial malformations (without the formation of an arteriovenous shunt) and mixed malformations.
Cavernomas can be found in any area of the brain because they can arise anywhere along the vascular bed. Intracranial extracerebral cavernous angiomas sometimes occur, but they are quite rare. Cavernous angiomas are also sometimes found in the spinal cord, most often in association with multiple vascular lesions of the brain.
Main causes of the disease
The exact reasons for the development of pathology have not been established. Medical experts are inclined to believe that cavernoma is a congenital disease caused by a viral infection in the womb during the formation of the embryo’s circulatory system. Factors that can also provoke vascular malforation in a child include:
- late pregnancy;
- chronic diseases in the mother's body;
- injuries during childbirth;
- mother's bad habits.
It is possible that a cavernoma may form at another period of life. The causes of the tumor may be:
- traumatic brain injuries;
- radiation therapy;
- infections;
- weak immunity;
- brain inflammation;
- heredity.
In some cases, cerebellar cavernoma occurs due to angiomas, hemangiomas, and other tumors of the brain or spinal cord.
Detection of cavernous angiomas
Despite the fact that cavernous angiomas are visualized using computed tomography (CT), this method is not the method of choice: the fact is that the identified signs in a CT study may correspond not only to cavernous angioma, but also, among other possible options, poorly differentiated tumor.
The sensitivity of magnetic resonance imaging (MRI) is much higher, due to its higher contrast resolution, as well as its greater ability to image flowing blood and its breakdown products. The combination of different MRI pulse sequences has largely solved the problem of misdiagnosis or under-detection of cavernous angiomas, since these lesions have quite specific features on MRI.
Get an MRI of the brain in St. Petersburg
CT and MRI can be used for follow-up of patients with already diagnosed cavernous angiomas, especially in cases where there is a risk of hemorrhage. Although the MR image of cavernous angiomas does not predict the occurrence of bleeding, MRI is the method of choice for long-term follow-up of patients with cavernous angiomas, as well as for the evaluation of family members of the patient who are at risk of having such malformations. In addition, MRI is extremely useful in planning surgical intervention, as it allows you to assess the size of the formation, its boundaries, and thus determine the type of operation and surgical approach.
With classical angiography, most cavernous malformations are not visualized, and even when signs are detected, they are extremely nonspecific. If the lesion develops in combination with other vascular malformations, which occurs in approximately 30% of patients with venous malformations, then its MR characteristics become much more complex and less specific. In such patients, angiography may be useful to further clarify the diagnosis.
Brain angioma treatment in Germany: surgery
If the angioma does not manifest itself in any way, it is permissible to simply observe it without using any treatment. However, quite often there is a need to remove it. The operation is prescribed for epileptic seizures, as well as in cases where bleeding has been detected and there is a risk of repeated hemorrhage. Statistics show that on average the risk of hemorrhage with cerebral angiomas is 1-15%, but if one hemorrhage has already occurred, then it can occur again in 35% of cases.
This is a rather complex operation that requires high skill of surgeons and the use of special equipment.
If a brain angioma is diagnosed, surgical treatment in Germany is carried out in the best medical centers by leading German neurosurgeons. This allows us to demonstrate high efficiency and minimal possibility of complications. Today, in standard world practice, microsurgical resection is used to remove brain angiomas, which produces complications in an average of 15% of cases. But in specialized clinics in Germany this percentage is much lower, since the problem is dealt with by top-class specialists.
Cavernous angioma or tumor?
Brain scanning using CT and MRI in most cases allows one to clearly distinguish a cavernoma from other brain formations, including tumors of varying degrees of malignancy. However, in some cases, differentiation of these formations represents a diagnostic problem, the solution of which requires extensive experience. In this regard, the ability to attract a highly qualified diagnostician is critical. In addition, high-quality interpretation of CT and MRI images provides a solution to other diagnostic problems: exclusion of surrounding cerebral edema, identification of the severity of hemorrhage, description of details affecting the operability of the cavernoma. If you are in doubt about the diagnosis, you should consult a radiologist from a leading center specializing in brain pathology. A second opinion from such a diagnostician can be very valuable in the differential diagnosis of angiomas and other pathological conditions.
Cavernous angiomas on CT
When using visualization methods, it is useful to separate the cavity into 3 components. These include (1) a peripheral pseudocapsule, consisting of glial tissue impregnated with hemosiderin, (2) an irregularly structured intermediate connective tissue separating the cavities, and (3) a central vascular part, consisting of vascular cavities with slow blood flow.
On CT images without contrast enhancement, a cavernoma appears as a focal formation of an oval or nodular shape, characterized by slightly or moderately increased X-ray density and does not have a volumetric effect on the surrounding parenchyma. Areas of calcification and hemosiderin deposition in the walls of fibrous septa, along with stagnation of blood in the cavities, contribute to increased x-ray density on non-contrast-enhanced images. On CT images, calcifications are detected in approximately 33% of all cavernomas. If the formation is old, then it may contain central non-contrasting areas of reduced density, which corresponds to cysts from resorbed hematomas.
Contrast enhancement can be minimal or maximal, although 70-94% of cavernous malformations are weakly or moderately enhanced after intravenous contrast. In most cases, good contrast is the result of increased blood flow in the vascular component of the mass. The heterogeneous “speckled” enhancement is caused by intravascular fibrous septa, and the low-density rim along the periphery is caused by a pseudocapsule of glial tissue surrounding the formation.
Mass effect is not typical for cavernomas, unless they are associated with recent hemorrhage. On CT images without contrast enhancement, cavernomas may not be detected at all. In hemorrhages and the formation of intracerebral hematoma, cavernomas are visualized as areas of focal signal enhancement in the area adjacent to the hematoma.
Any hemorrhage detected on CT in a relatively young patient should be carefully investigated, and cavernous angioma should always be considered as a possible cause. When evaluating a patient with a seizure disorder, cavernous angioma should also be considered as a likely etiological factor, especially if the patient is between 20 and 40 years of age.
Cavernous malformations identified by CT may also include other rare vascular malformations (thrombosis of arteriovenous malformation, capillary telangiectasia), glioma (poorly differentiated astrocytoma or oligodendroglioma), and metastatic melanoma.
Recommendations
Association of Neurosurgeons of Russia
CLINICAL GUIDELINES
TREATMENT OF PATIENTS WITH CAVERNOUS MALFORMATIONS OF THE CENTRAL NERVOUS SYSTEM.
Clinical recommendations were approved at the Plenum of the Board of the Association of Neurosurgeons of Russia Kazan November 27, 2014
Authors' team
Konovalov Alexander Nikolaevich Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Sciences, Scientific Director of the Research Institute of Neurosurgery named after. acad. N.N. Burdenko
Belousova Olga Benuanovna Doctor of Medical Sciences, leading researcher at the Department of Vascular Neurosurgery of the Research Institute of Neurosurgery named after. acad. N.N. Burdenko
Okishev Dmitry Nikolaevich Candidate of Medical Sciences, researcher at the Department of Vascular Neurosurgery of the Research Institute of Neurosurgery named after. acad. N.N. Burdenko
Gavryushin Andrey Vladimirovich Candidate of Medical Sciences, senior researcher at the Department of Neuro-Oncology, Research Institute of Neurosurgery named after. acad. N.N. Burdenko
Khukhlaeva Elena Anatolyevna Candidate of Medical Sciences, senior researcher at the Department of Pediatric Neurosurgery of the Research Institute of Neurosurgery named after. acad. N.N. Burdenko
Kornienko Valery Nikolaevich Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Sciences, Head of the Department of X-ray Surgical Methods of Diagnostics and Treatment of the Research Institute of Neurosurgery named after. acad. N.N. Burdenko
Pronin Igor Nikolaevich Doctor of Medical Sciences, Professor Corresponding Member of the Russian Academy of Sciences, Chief Researcher of the Department of X-ray Surgical Methods of Diagnostics and Treatment of the Research Institute of Neurosurgery named after. acad. N.N. Burdenko
Shishkina Lyudmila Valentinovna Candidate of Medical Sciences, Head of the Laboratory of Pathomorphology of the Research Institute of Neurosurgery named after. acad. N.N. Burdenko
Sazonova Olga Borisovna Candidate of Medical Sciences, leading scientist of the laboratory of clinical neurophysiology of the Research Institute of Neurosurgery named after. acad. N.N. Burdenko
Golanov Andrey Vladimirovich Doctor of Medical Sciences, Professor
1. METHODOLOGY FOR EVALUATING CLINICAL GUIDELINES.
Standard. Generally accepted principles of diagnosis and treatment, which can be considered as mandatory treatment tactics (efficacy confirmed by several randomized studies, meta-analyses or cohort clinical studies).
Recommendation. Therapeutic and diagnostic measures recommended for use by most experts on these issues. May be considered as treatment options in specific clinical situations (efficacy confirmed by individual randomized trials or cohort clinical studies).
Option. Therapeutic or diagnostic measures that may be useful (the effectiveness is confirmed by the opinion of individual experts, in individual clinical cases).
Not recommended. Therapeutic and diagnostic measures that do not have a positive effect or may cause harm (any level of confirmation).
According to our data, as well as information from other sources, there are no randomized trials on the problem of cavernomas in the published literature (1).
2. GENERAL QUESTIONS.
Cavernous malformations (CM) belong to a group of malformations of the vascular system of the brain and spinal cord. The prevalence of the pathology in the population is about 0.5% (2, 3), however, judging by the number of requests, only a small part of CM manifests itself clinically. There is no information on the ratio of asymptomatic and clinically manifested forms. Among clinically manifested vascular malformations, CMs account for about 15%, occupying three times the place after AVMs. CMs occur in sporadic and hereditary (familial) forms (4, 7). According to average data, sporadic cavernomas make up about 80% of cases, hereditary ones - about 20%. CMs can be single or multiple. Single CMs occur predominantly in sporadic forms of pathology, and multiple ones in hereditary ones. The number of multiple cavernomas in one person can range from two to several dozen. CMs can form in any part of the central nervous system. The most common CMs are the cerebral hemispheres (70%), with a significant predominance of CMs in the frontal and temporal lobes. Deep CMs of the cerebral hemispheres (basal ganglia, diencephalon) make up about 10% of all cavernomas. About 28% are CMs of the posterior cranial fossa. Cavernomas of the spinal cord are rare (2 - 5%) (5). Clinical manifestations of CM can occur at any age, from infancy to the elderly. Most often, the first clinical symptoms appear between the ages of 20 and 40 years. In approximately 25% of cases, the first manifestations of the disease occur in childhood (up to 18 years). In the hereditary form, CM may appear at an earlier age. CMs, as a rule, have a benign course. The disease rarely leads to severe disability, and cases of death are rare and occur mainly in CM of the brain stem and diencephalic region (4).
3. ORGANIZATION OF MEDICAL CARE.
Patients with clinically manifested CM of the central nervous system make up about 5% of patients who consult a neurosurgeon. It is unknown how often neurologists and general practitioners encounter this pathology, but it can be assumed that such cases are rare. These data justify the need for consultation, observation and, if necessary, treatment of patients with CNS CM in specialized neurosurgical institutions with specialists experienced in managing patients with this pathology, or with neurologists specializing in the treatment of cerebrovascular pathology (recommendation). The benign course of the disease and the absence in most cases of symptoms that threaten the patient’s life allow patients to be referred to a specialized institution for an outpatient consultation as planned (recommendation). The exception is cases of CM of the brain stem and deep parts of the cerebral hemispheres, manifested by severe neurological symptoms. These patients should be quickly hospitalized in a neurosurgical hospital, as they may require urgent neurosurgical care (recommendation). To provide qualified care to patients with CNS CM, the hospital must be equipped with MRI and have an operating room for microsurgical interventions (standard). To remove deep cavities and cavities of functionally significant areas, the operating room must be equipped with neuronavigation, and it must be possible to carry out neurophysiological monitoring (recommendation). Patients who have undergone neurosurgical surgery, as well as patients who do not require neurosurgical assistance, should be under the supervision of a neurologist for a long time. Due to the fact that the overwhelming majority of patients suffer from epileptic seizures, the provision of out-of-hospital care requires the participation of a specialist epileptologist or neurologist with experience in prescribing anticonvulsants (recommendation).
4. DIAGNOSTICS.
The main mechanism for the development of any clinical symptoms in cavernomas is micro- or macro-hemorrhages. It is also possible that symptoms may develop due to thrombosis and impaired venous outflow; occlusion of the cerebrospinal fluid pathways; epileptogenic effects of blood breakdown products. The clinical picture of CM is represented by epileptic seizures, acute or subacute development of focal neurological symptoms, occurring either against the background of general cerebral symptoms or in its absence (typical or atypical hemorrhage). Epileptic seizures tend to become more frequent and more complex (6). In rare cases, drug-resistant epilepsy may develop. Rare manifestations include the development of a disease such as subarachnoid hemorrhage, hypertensive-hydrocephalic syndrome, in the form of symptoms of damage to individual cranial nerves. CM can be detected in people being examined for headaches, as well as during examination for any other diseases (incidental findings). Primary diagnosis is carried out mainly on an outpatient basis (recommendation). The exception is patients with severe neurological symptoms requiring hospitalization. The main diagnostic method for detecting cavities is MRI. The sensitivity of the method for this pathology reaches 100%, specificity - 98%. MRI should be performed on a device with a magnetic field strength of at least 1.5 Tesla in T and T2 modes and modes weighted by magnetic field inhomogeneity (SWI: T2*GRE, SWAN) (recommendation). Variants of the type of cavernoma on MRI when examined in various modes are classified by J. Zabramski et al (7). There are four types of cavernomas: type I cavernoma is a cavernoma with signs of hematoma inside or outside the main formation; Type II cavernoma has a heterogeneous signal in both modes and a hypointense perifocal rim-type signal in T2 mode (“classic” cavernoma); type III cavernoma is represented by a clearly defined round formation in the form of an iso- or hypointense homogeneous signal in the T1 mode, a hypointense signal in the T2 mode; Type IV formations are represented by a pointy rounded homogeneous hypointense signal, visualized only in modes weighted by magnetic field inhomogeneity. They are usually combined with one or more typical cavernomas. Due to insufficient knowledge of morphology, type IV formations are conditionally classified as cavernomas. Cavernomas must be differentiated from intracerebral tumors, large and giant aneurysms, thrombosed AVMs. For differential diagnosis with a tumor, it is possible to perform an MRI with contrast enhancement—cavities are not characterized by accumulation of contrast (optional). In the differential diagnosis of AVM and aneurysm, it is advisable to perform cerebral angiography (optional). A false-positive diagnosis of cavernoma is more dangerous than a false-negative one, since there is a possibility of “missing” a disease with a life-threatening course. If multiple cavernomas are identified, as well as in the presence of blood relatives with a history of epileptic seizure(s), intracranial hemorrhage or focal neurological deficit, it is necessary to recommend an MRI study to blood relatives to identify hereditary forms of the disease (recommendation). The final diagnosis of cavernoma can only be made based on the results of histological examination. CT and AG are not methods for making the diagnosis of cavernoma. They can be used as auxiliary: CT to confirm the fact of acute or subacute hemorrhage; AG (SCT-AG) - to identify venous angiomas, often accompanying cavernous malformations. An electroencephalographic examination (EEG) is performed on patients with cavernomas in cases where they suffer from epileptic seizures, as well as to confirm the epileptic nature of the paroxysms (optional). Patients with multiple cavernomas suffering from epileptic seizures require an EEG, as well as video-EEG monitoring or 24-hour EEG monitoring to identify an epileptogenic cavernoma (recommendation).
5. TREATMENT OF THE DISEASE.
The management tactics and choice of treatment method for patients with cavernous malformations depend, first of all, on the localization and clinical manifestations of the pathology. The size of the cavernoma, the age of the patient, and the presence of concomitant diseases are also of certain importance. The following options for management and treatment of the patient are possible: observation, conservative therapy, removal of cavernoma, radiosurgical treatment. The disease generally has a benign course, and therefore in most cases the indications for surgery are relative. The patient and/or his relatives must be fully informed about the options for the course of the disease, the features and complications of various types of treatment, and must make an independent decision on the proposed treatment methods. 5.1. Surgical treatment of cavernomas should be carried out in a hospital equipped with the necessary equipment: neuronavigation to remove deep and small cavernomas, neurophysiological monitoring to remove cavernomas from functionally significant locations. Removal of deep cavities and trunk cavities should be performed only in clinics with extensive experience in performing such operations. The operation is indicated in the following cases (recommendation): • cortical and subcortical cavernomas of the cerebral hemispheres, manifested by hemorrhage or epileptic seizures, and located outside functionally significant areas; cavernomas of the lateral parts of the cerebellar hemispheres, manifested by hemorrhage; • cortical and subcortical cavernomas of the cerebral hemispheres, located in functionally significant areas, deep cavernomas of the cerebral hemispheres, cavernomas of the brain stem, cavernomas of the medial parts of the cerebellar hemispheres, manifested by repeated hemorrhages with the formation of persistent neurological disorders (or with severe epileptic syndrome). The operation is not indicated in the following cases (recommendation): • clinically asymptomatic cavernomas in the absence of signs of previous hemorrhages on MRI; • cortical and subcortical cavernomas of the cerebral hemispheres, located in functionally significant areas, and occurring with rare epileptic seizures that respond well to treatment with anticonvulsants, in the absence of focal neurological symptoms; • cortical and subcortical cavernomas of the cerebral hemispheres, located in functionally significant areas, deep cavernomas of the cerebral hemispheres, cavernomas of the brain stem, cavernomas of the medial parts of the cerebellar hemispheres, manifested by a single hemorrhage with complete regression of focal neurological symptoms. In difficult cases, the decision about surgery should be made on an individual basis by a council of doctors. When removing cavernomas, it is necessary to strive for complete removal of the formation, since partial removal is associated with a high risk of re-hemorrhage from the remains of the cavernoma (recommendation) (4, 8). When removing deep cavernomas and cavernomas located in functionally significant areas of the brain, in order to minimize trauma to adjacent structures, it is preferable to remove the cavernoma by fragmentation (recommendation) (9). In the presence of acute or subacute hematoma, surgical trauma can be reduced by evacuation of the hematoma (internal decompression) (4). When removing cavernomas from the sensorimotor cortex, preliminary neurophysiological mapping using electrical stimulation with assessment of M-responses is necessary (recommendation). When removing deep and small cavernomas in a situation where there are no clear anatomical landmarks, it is necessary to use intraoperative stereotactic navigation (recommendation). When removing a cavernous brainstem, in some cases, electrical stimulation of the brainstem nuclei with registration of M-responses from the corresponding muscles of the face and head is required (recommendation). To improve the effectiveness of control of epileptic seizures, removal of cavernomas outside functionally significant areas can be combined with resection of the altered perifocal medulla (optional). When removing cavernomas manifested by episyndrome, it is possible to use intraoperative ECoG to control the degree of excision of the perifocal epileptogenic zone and to search for distant foci of epileptic activity (optional). For cavernomas of the temporal lobe in patients with epileptic seizures resistant to anticonvulsant therapy and/or a long history of seizures, the possibility of performing a simultaneous amygdalohippocampectomy (optional) should be considered. 5.2. Patient management in the postoperative period. In the immediate postoperative period, the patient must undergo a control CT or MRI study. The final MRI control of the completeness of cavernoma removal should be carried out 4 - 6 months after surgery. To do this, it is necessary to perform a control MRI according to the same principles as before the operation. Management of patients with epileptic syndrome is carried out according to the rules for the treatment of patients with epilepsy (10) (recommendation). In case of development of drug-resistant epilepsy, the possibility of antiepileptic surgical interventions should be considered. 5.3. Radiosurgical treatment. The experience of radiosurgical treatment of fairly large groups of patients with cavernous malformations (more than 50 cases) is presented in several clinical studies. Most of them indicate a 3- to 10-fold reduction in the risk of recurrent hemorrhages more than 2 years after the first manifestation of the disease (11). Data are also provided on a decrease in the frequency of epileptic seizures, however, this information is unreliable (12). The risk of developing clinical post-radiation complications ranges from 2.45 to 16% (13, 14). Thus, radiosurgical treatment of cavernomas is recommended in cases of repeated hemorrhages with the development of severe neurological deficits, if direct surgical intervention is associated with a high risk of significant worsening of neurological deficits (cavernoma of the diencephalic region, thalamus opticus, brainstem cavernoma). 5.4. Conservative treatment. If there are no indications for surgery or refusal, patients with cavernous malformations should remain under the supervision of a neurologist or neurosurgeon. Epileptic syndrome is treated with anticonvulsants in accordance with the general principles of treatment of epilepsy (10) (standard). The drug should be taken in a therapeutic dose based on the patient’s body weight (recommendation). Monitoring the sufficiency of the dose is carried out clinically (standard), by determining the concentration of the drug in plasma (recommendation) and according to EEG data (optional). 5.5. Medina rehabilitation. Rehabilitation measures are carried out according to indications in accordance with the general principles of rehabilitation of neurological and neurosurgical patients.
1. Guidelines for the management of cerebral cavernous malformations in adults. Samarasekera N, Poorthuis M, Kontoh K, Stuart I, Respinger C, Berg J, Kitchen N, Salman R. 2. Robinson JR, Awad IA, Masaryk TJ, Ester ML “Pathological heterogeneity of angiographically occult vascular malformations of the brain” Neurosurgery , 1993, 33, 547 -554. 3. Washington CW, McCoy KE, Zipfel GJ. Update on the natural history of cavernous malformations and factors predicting aggressive clinical presentation. Neurosurg Focus. 2010 Sep;29(3):E7. 4. Belousova O.B., Konovalov A.H., Okishev D.N. and others. “Hereditary brain cavernomas: analysis of 12 families” J. Vopr. Neurosurgery, 2011, 4, 34 - 45. 5. Lanzino G., Spetzler RF (eds). Cavernous Malformations of the Brain and Spinal Cord. NY: Thieme, 2008. 6. Moran NF, Fish DR, Kitchen N, Shorvon S, Kendall BE, Stevens JM. Supratentorial cavernous haemangiomas and epilepsy: a review of the literature and case series. J Neurol Neurosurg Psychiatry. 1999 May;66(5):561-8. 7. Zabramski JM, Wascher TM, Spetzler RF, Johnson B, Golfinos J, Drayer BP, Brown B, Rigamonti D, Brown G. The natural history of familial cavernous malformations: results of an ongoing study. J Neurosurg 80:422–432, 1994. 8. Mathiesen T, Edner G, Kihlstrom L. Deep and brainstem cavernomas: a consecutive 8-year series. J Neurosurg. July 2003; 99(1): 31-7. 9. Gross BA1, Batjer HH, Awad IA, Bendok BR. Cavernous malformations of the basal ganglia and thalamus. Neurosurgery. 2009 Jul;65(1):7-18; discussion 18-9. 10. Zenkov L.R. “Clinical epileptology” Moscow, Med Inform Agency, 2010. 11. Kondzilolka D, Flickinger JC, Lunsford LD “Radiosurgery for cavernous malformations” In: Lanzino G, ed., Spetzler RF, ed. Cavernous Malformations of the Brain and Spinal Cord. Thieme, 2008, 124 - 129. 12. Pham M, Gross BA, Bendok BR, et al “Radiosurgery for angiographically occult vascular malformations” Neurosurcical Focus, 2009, 26, E16. 13. Amin-Hajani S, Ogilvy CS, Candia GJ et al, “Stereotactic radiosurgery for cavernous malformations: Kjellberg's experience with proton beam therapy in 98 cases at the Harvard cyclotron” Neurosurg, 1998, 42, 1229-1238. 14. Liu AL, Wang CC, Dai K “Gamma knife radiosurgery for cavernous malformations.” Zhongguo Yi Xue Ke Xue Yuan Xue Bao, 2005, 27, 18 - 21.
Cavernous angiomas on MRI
Cavernous angiomas represent about 1% of all intracranial vascular lesions and 15% of cerebrovascular malformations. With the development and introduction of MRI, cavernous angiomas have become the most commonly detected vascular malformations of the brain. In early studies on autopsy material, the frequency of their occurrence was 0.02-0.53%. Using MRI, the incidence of formations similar to cavernous hemangiomas was 0.39-0.9%, and the detection of previously unidentified asymptomatic formations using MRI increased their incidence to 0.45-0.9%.
Get an MRI of the brain in St. Petersburg
On MRI, parenchymal cavernous angiomas are represented by a characteristic “popcorn”-type formation, clearly defined, with a smooth border. The internal part is represented by multiple foci of signal of varying intensity, which correspond to hemorrhages at different stages of resolution.
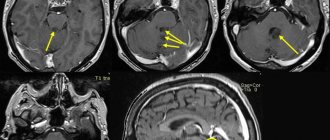
MRI signs of cavernous angioma. Large cavernous angiomas of the right frontal lobe and left occipital lobe on T1-weighted axial section. These two heterogeneous space-occupying lesions have a central mesh structure with alternating areas of high and low signal intensity, surrounded by a hypointense rim of hemosiderin.
A fresh hematoma containing deoxyhemoglobin is isointense on T1-weighted images and significantly hypointense on T2-weighted images. A subacute hematoma containing extracellular methemoglobin is hyperintense on both T1- and T2-weighted images due to the paramagnetic effect exerted by methemoglobin.
Intermediate fibrous elements are characterized by a weakly hypointense signal on T1- and T2-weighted images, since they contain calcifications and hemosiderin. The heterogeneous interior of the mass is surrounded by a hemosiderin rim, which has low intensity on T1-weighted images. The hypointensity of this rim becomes more pronounced, resembling a halo, on T2-weighted and gradient-echo images due to the higher sensitivity of these sequences to changes in the magnetic field.
Axial gradient-echo MR images provide better visualization of large cavernous angiomas in the right frontal and left occipital lobes. The hemosiderin rim appears as a halo due to the increased magnetic susceptibility of hemosiderin.
Smaller cavernomas appear as low-intensity nodules on T1- and T2-weighted images.
Small lesions are better visualized on gradient echo images due to the increased sensitivity to changes in the magnetic field that is inherent in such pulse sequences. It has also been shown that in sequential gradient echo images, small punctate formations are better visualized with longer echo times; these data suggest that such formations contain paramagnetic substances.
Gradient-echo MR imaging shows multiple bilateral small, punctate and round, low-intensity lesions in the periventricular and subcortical white matter. The largest lesion is visualized in the periventricular white matter of the frontal lobe anterior to the anterior (frontal) horn of the left lateral ventricle near the genu of the corpus callosum. Multiple smaller lesions are visible anterior and posterior to it.
On time-of-flight angiography images, methemoglobin in the center of a cavernous malformation may resemble moving blood. However, on a subsequent phase-contrast MR angiogram obtained with a low blood flow speed setting during encoding (10-20 cm/s), blood flow or pathological vascularization is not visualized, which makes it possible to exclude vascular lesions.
Typically, cavernous angiomas do not have a bulking effect on adjacent tissue or cause edema, and they do not have a feeding artery or draining vein unless they are associated with other similar vascular malformations. Cavernous angiomas are often associated with venous malformations, which are characterized by the presence of a draining vein. In such mixed cases, standard angiography may be useful.
T2-weighted image of a cavernoma of the pons.
Cavernous malformations detected on MRI include other occult vascular malformations (AVM/aneurysm thrombosis, capillary telangiectasia), hemorrhage in a primary or secondary tumor (metastasis of melanoma, choriocarcinoma, thyroid or kidney cancer), amyloid angiopathy, treated or primary infection (toxoplasmosis or cysticercosis), multiple hemorrhages associated with damage to the blood system (disseminated intravascular coagulation, leukemia), as well as the consequences of diffuse axonal damage.
Varieties of the disease
Types of pathology are distinguished depending on where the benign formation is located in the frontal (right frontal) or parietal region, left temporal part, cerebellum, as well as thrombotic angioma.
According to histology, there are three types of cavernomas:
1. Classic
- the most common. The formation, in the form of a capsule with caverns, without vessels, fibers and without layers of brain tissue, clearly borders the brain.
2. Mixed
– in addition to caverns, the tumor consists of various vessels with layers of brain tissue.
3. Proliferative
– with the presence of areas of endothelial proliferation.
In addition, cavernomas are divided into subacute and chronic, with and without symptoms indicating hemorrhage. The clinical picture depends on the type of disease. Treatment for different types of cavernoma may also vary. The modern diagnostic complex in our clinic allows us to make the most accurate diagnosis and prescribe the correct treatment for such dangerous ailments as cavernoma, cervical osteochondrosis, intervertebral hernia, etc.