Causes
The disease is hereditary, linked to the X chromosome, so boys are almost always affected. Girls are carriers of a pathological gene (boys rarely survive to adulthood, and, moreover, are usually sterile). A change in the structure of the gene responsible for the synthesis of the dystrophin protein occurs on the chromosome.
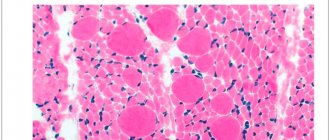
Although the content of dystrophin in skeletal muscles is extremely small (thousandths of a percent), without it necrosis of muscle tissue quickly develops and progressive muscle dystrophy develops. If the gene is damaged in a site that completely destroys the synthesis of the dystrophin protein, Duchenne dystrophy develops. When insignificant parts of the protein are involved in the process, the disease takes the form of Becker's dystrophy.
Forms of muscular dystrophy in adults
All figurative forms of the disease in question in adults differ:
- types of inheritance;
- the speed and nature of its flow;
- the presence or absence of tendon retractions and pseudohypertrophies;
- the timing of the start of the process;
- the unique topography of muscle pain;
- other signs of progressive muscular dystrophy.
Issues of classification of myopathy (chronic and progressive hereditary muscle diseases) are being developed in different directions. Muscular dystrophy in adults is classified according to the type of inheritance:
- Autosomal dominant.
- Autosomal recessive.
- Dominant and recessive.
- Linked to the X chromosome.
Symptoms
The onset of symptoms begins in early childhood, usually between 1 and 3 years. Initially, there is a delay in motor development, the child begins to walk late, often stumbles when walking, and gets tired quickly. Later, constant pathological muscle fatigue develops. The child practically cannot climb stairs. The gait begins to resemble a “duck” gait.
A characteristic symptom is the “ladder” symptom: an attempt to get up from a sitting position occurs using the hands, gradually, slowly, in several stages.
Gradually, muscle atrophy begins to be noted, first in the proximal parts of the lower, then upper extremities. Later, the muscles of the pelvic girdle, hips, back, and shoulder girdle atrophy. A “wasp” waist, curvature of the spine, and protruding shoulder blades (pterygoid blades) almost always develop.
Almost always there is a characteristic symptom of progressive Duchenne muscular dystrophy - pseudohypertrophy of the leg muscles. The muscles, although increased in volume, do not have sufficient strength and are very painful to the touch.
Three stages of the disease can be distinguished: - Stage I - weakness manifests itself only with significant physical activity (usually the first year of the disease). — Stage II – difficulty climbing stairs, weakness when walking quickly develops. — Stage III – represents paralysis, muscle contractures with the inability to move independently.
According to the type of course, it is divided into: Rapid progression. The ability to move is lost quickly, within the first 4-5 years from the onset of the disease. Average rate of progression: the patient cannot move after 10 years. Slow progression: there are no pronounced motor disorders 10 years after the onset of the disease. Typically, this option is characteristic of other types of muscular dystrophies than Duchenne dystrophy.
Congenital muscular dystrophies and structural myopathies
Congenital (congenital) myopathies are a group of genetically determined myopathies characterized by early onset (usually from birth to 1 year), a characteristic symptom complex (floppy child syndrome) and a non-progressive or slowly progressive course. Among congenital myopathies, congenital muscular dystrophies and congenital myopathies (structural myopathies) are distinguished.
CLINICAL PICTURE
Most congenital myopathies and dystrophies are manifested by the “flaccid child” syndrome. Clinical manifestations of the “floppy child” syndrome are reduced to severe muscle hypotonia, weak muscle resistance during passive movements, head incontinence, delayed motor development, and joint hypermobility. “Floppy child” syndrome is also observed in spinal muscular atrophy and other congenital diseases of the central nervous system, metabolic diseases (glycogenosis, aminoaciduria), etc. Approximately 80% of cases of “floppy child” syndrome are caused by primary damage to the central nervous system. The main method for diagnosing congenital myopathies is a morphological study of muscles; EMG only confirms the primary muscular nature of the lesion at the initial stage of differential diagnosis. Along with the “flaccid child” syndrome, weakness of the facial muscles, trunk muscles and respiratory muscles is noted. The majority develop contractures of the hip, knee and elbow joints, neck extensor muscles, scoliosis, and later external ophthalmoplegia may develop. Despite delayed motor development, most children are able to sit independently, some can walk independently (with partial merosin deficiency). EMG reveals the primary muscle type of changes, while the spontaneous activity of muscle fibers is either absent or insignificant.
SYMPTOMS
For Fukuyama congenital muscular dystrophy, severe muscle weakness is typical (children are either not able to walk independently at all, or begin to walk only at the age of 2-8 years), symptomatic epilepsy (in 50%), mental retardation, ophthalmological pathology (microphthalmia, retinal hypoplasia, cataracts). , myopia, strabismus). Multiple and varied changes on MRI are characteristic (dysplasia, agyria, ventricular dilatation, cysts). Ullrich congenital muscular dystrophy, in addition to the “floppy child” syndrome, is characterized by kyphosis, hypermobility of the distal joints, hip dysplasia, and hyperkeratosis. The ability to walk independently depends on the severity of the disease, but by the age of 2-10 years, as a rule, it is lost due to severe contractures. Walker-Warburg syndrome is one of the most severe congenital neuromuscular diseases (average life expectancy is 9 months). Numerous congenital anomalies are observed: meningocele, agyria, agenesis of the corpus callosum, pyramidal tract hypoplasia, ventricular enlargement, microcephaly, microphthalmia, optic nerve hypoplasia, cataracts, glaucoma and other changes leading to blindness, “floppy child” syndrome and bulbar disorders.
TREATMENT
Treatment should be carried out exclusively by a neurologist. Self-medication is unacceptable. There is no specific therapy; the goal of treatment is the correction of orthopedic disorders (hip dysplasia, scoliosis), prevention of contractures, maintenance of muscle strength, treatment of cardiomyopathy and symptomatic epilepsy.
Diagnostics
The clinical picture is very bright. Often the disease is diagnosed after clarifying a genetic history (presence of cases in the family) and a neurological examination. In the neurological status, the disappearance of knee reflexes is noted, a little later reflexes from the biceps and triceps disappear. Achilles reflexes are preserved for a long time.
Externally, deformation of the joints of the foot may be revealed, there are signs of cardiomyopathy: irregular pulse, dullness of heart sounds, dilation of the heart cavities according to EchoCG, changes in the electrocardiogram.
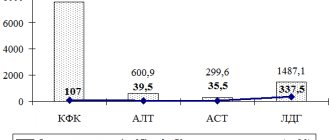
An important factor is the increase in the biochemical parameters of creatine phosphokinase (an enzyme indicator of muscle breakdown). The activity of this enzyme increases tens of times. There is a direct correlation between the degree of increase in enzyme activity and the severity of manifestations of Duchenne dystrophy. [!] In difficult diagnostic situations, a cytological examination is performed.
Causes of childhood dystrophy
Medicine names various causes of dystrophy in children, the most common of which are:
- congenital genetic metabolic disorders;
- chromosomal and somatic diseases;
- stress;
- external unfavorable conditions and factors: unbalanced nutrition (overeating or prolonged fasting), insufficient attention, negative emotional impact on the child, violations of the daily routine, neglect of hygiene procedures (changing diapers, bathing, walks in the fresh air), physical inactivity;
- poor nutrition;
- digestive problems;
- weak immunity;
- infectious diseases;
- unfavorable course of pregnancy: a woman’s full-time employment during maternity leave, harmful working conditions, stressful situations, alcoholism, smoking, severe toxicosis.
It is a mistaken opinion that one of the causes of childhood dystrophy is prematurity of the child, premature birth. But too young or old age of the mother can cause a congenital disease.
Treatment and life prognosis
Treatment is symptomatic. Hormonal drugs are used to stop the destruction of muscle fiber, phospholipids to protect muscle cells from destruction, and elements of therapeutic exercises. Various orthopedic devices are being introduced into practice to facilitate movement. Massage is strictly contraindicated in most cases, as it can lead to accelerated muscle breakdown. Treatment of hereditary diseases is a matter of the future.
The life prognosis for patients is unfavorable. The course of the disease is progressive. Death is inevitable. As a rule, by the age of seven, severe symptoms develop, leading to complete immobility by the age of 13-14. Patients rarely live to 18-20 years of age.
Prevention and treatment of dystrophy
Complex treatment of dystrophy in children depends on the type of disease and its severity. Hypotrophy of the I degree is treated at home, II and III - in a hospital setting until the child is placed in a box. The main treatment methods include:
- treatment of the disease that caused dystrophy;
- diet therapy: breastfeeding, fermented milk mixtures, fractional nutrition;
- prevention of secondary infections;
- prescription of vitamins, enzymes, stimulants and dietary supplements.
Prevention of dystrophy in children suggests that already during pregnancy the mother must follow a daily routine, give up bad habits, and monitor her health. After the birth of the baby, it is necessary to adhere to feeding rules, recommendations for caring for him, promptly identify and treat any diseases, visit the pediatrician monthly, and monitor the child’s height and weight.
Your child's health is in the capable hands of our doctors. Make an appointment with the medical pediatricians in Alexandrov by calling 8 (49244) 9-32-49.
Diagnosis of congenital myopathy
Diagnosis of congenital myopathies is a complex process, since the doctor needs to differentiate and determine the specific type of myopathy in order to prescribe adequate treatment and make the correct diagnosis. A neuropathologist identifies neurological symptoms, conducts electrophysiological and biochemical studies to establish heterozygous carriage of the myopathic gene. Electromyographic examination using cutaneous electrodes often shows a decrease in the voltage of the EMG curve. When performing a biochemical blood test, an increased concentration of aldolase and creatine kinase is observed in the serum.
Common types of disease
- Duchenne muscular dystrophy.
- Becker muscular dystrophy.
The disease develops in children aged 3–5 years. It begins with damage to the lower extremities and gradually rises higher. This is a rapidly progressive form that leads to muscle atrophy after 5 years. It is characterized by heart damage and the development of mental disorders.
The process also begins from the lower extremities. Weakness in the legs and fatigue first appear at the age of 15–20 years. The transition of the disease to the upper limbs due to muscular dystrophy is observed in adults after 50 years.
Classification and symptoms
There are several types of classical pathologies. The most common forms2:
- "central core" disease;
- multicore myopathy;
- centnuclear;
- non-raspberry.
Symptoms of pathologies can be different. One of the main signs is muscle weakness, which appears from birth. However, there are cases where weakness appears in adulthood, although this is uncommon.2
Muscle weakness can occur in utero, causing the fetus to be less active. The greatest muscle hypotonia is usually observed in the pelvic girdle and legs. The muscles of the arms and shoulder girdle suffer less.2
With myopathy in children, skeletal abnormalities can be detected - hip dislocation, cavus foot, kyphoscoliosis, contractures of large joints and others. Sometimes muscle pain may occur during or after physical activity and even at rest.2
The severity of symptoms can be very minor, so much so that sometimes a person does not even suspect that he is sick. But some pathologies manifest themselves with specific signs. For example, with nemaline myopathy, scoliosis develops, a keeled chest develops, and the face takes on an elongated, oblong shape.2