Photo from the site nedugamnet.ru – We need to change our worldview. Cerebral palsy is an incurable disease; it cannot be cured. But it is possible and necessary to teach the child and his parents to live with this illness, says Vera Zmanovskaya.
Vera Anatolyevna is a pediatric neurologist, chief freelance pediatric rehabilitation specialist at the Department of Health of the Tyumen Region, and chief specialist in pediatric rehabilitation at the Ministry of Health of the Russian Federation in the Ural Federal District.
For the fourth year under her leadership, something unusual has been happening in Tyumen: the state is building a proper, advanced system of helping children with cerebral palsy at the regional level. With the development of a route of long-term care for each child, with training for parents, with the use of evidence-based methods, and even with a mobile application that calculates a plan of medical action depending on the degree and dynamics of the child’s disorders. This is not the case either in Moscow or in St. Petersburg. For capitals this is still an unattainable dream.
Evidence-based rehabilitation
Photo from the site /ilizarov.ru
– Vera Anatolyevna, tell us what exactly are you changing in the model of helping children with cerebral palsy in Tyumen?
– Over the past 4 years, we have been trying to promote the European model of helping children with cerebral palsy. There are many models - there is an American one, there is an Australian one. But we took the European model as a basis, translated it and are trying to follow the principles of monitoring children with cerebral palsy.
According to this model, any rehabilitation of a child with cerebral palsy should be based on clearly evidence-based principles. These must be proven and effective methods of treatment - Europe will not spend money any other way.
We found this model very interesting. In all children, before taking them for rehabilitation, we must definitely assess their rehabilitation potential. The potential of a child today is greatly appreciated. According to the classification system that exists everywhere in the world, and which we are trying very hard, with difficulty, to understand in Russia.
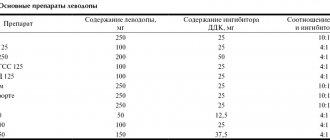
– What kind of classification is this?
– Cerebral palsy has different degrees of severity. Since 1997, all European doctors have followed the classification system for global motor functions. Unfortunately, in Russia it was officially adopted only in 2014. This is a very serious scale.
In this classification, the potential of children with cerebral palsy is divided into V levels of motor functions, and each level is further divided into age periods: 1.5-2 years; 2-4 years; 4-6 years; 6-12 years old and 12-18 years old.
The European classification system – the potential of children with cerebral palsy is divided into V levels. Photo: cerebralpalsy.org.au
Using this scale, we can determine the level of motor impairment as early as one and a half years. And when we set the level of motor functions, the classification system prescribes all stages of child development up to 18 years of age.
The movement develops according to its own laws. If a child has level I movement, established at one and a half years old, he has a 100% chance of mastering independent walking by the age of 2 years. If a child is assigned level II, it means he has a chance to go independently before the age of 4.
If a child has a level III-V impairment of motor functions, then such a child will not walk independently, but children of level III can go with additional means of rehabilitation, children of level IV will be able to sit with support. Level V is only for bedridden children who can only hold their head up.
Children of level IV-V everywhere in the world today are transferred to the status of palliative patients. And, seeing a child at 1.5-2 years old, we can already predict his rehabilitation potential and understand what rehabilitation methods can be applied. If we are talking about children of levels IV-V, then rehabilitation is also carried out, but according to different principles.
Using a large group of patients, our Canadian colleagues showed that children of different levels of movement reach the maximum of their motor development at a certain time. For example, level I are well-walking children who reach the ceiling of their level of movement at approximately 4.5-5 years, like healthy children. Maybe they place their feet incorrectly or have some problems with coordination, but these are children who will run, jump, and play sports.
Children of III-IV levels of movement reach the maximum of their development already at 3.5-4 years, and we are not even talking about any activation of movement or some kind of stimulation of the musculoskeletal system, because the laws limit us to this period. Children of movement level V reach the motor ceiling by 2.5-3 years.
This classification system helps us, doctors, when we argue to parents that the rehabilitation potential has been exhausted. After all, to say: “Your child will never walk” and put nothing into it other than emotions is wrong, parents will simply be offended and leave.
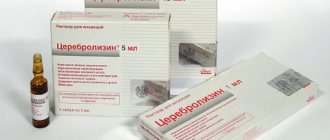
Quota stumbling block
In the West, such operations have been performed for more than 20 years. For us, quite recently. One of the pioneers was the Research Clinical Institute of Pediatrics named after Academician Yu. E. Veltishchev. Local surgeons have already installed more than 100 baclofen pumps and performed more than a dozen operations to stimulate deep brain structures and selective dorsal rhizotomy.
Doctors admit: there would be much more such operations if more quotas were allocated for them. It all comes down to expensive devices, which doctors receive in very limited quantities. Experts hope that over time the situation will change for the better. After all, the effect of such operations more than pays for all government expenses: children spend less time in the hospital and need less rehabilitation support. And most importantly, their quality of life improves. What could be more important?
By the way
Abroad, operations to install baclofen pumps are performed on children from 5 years of age. At the Research Institute of Pediatrics, this operation was the first in the world to be performed on very young children – 1.5–2 years old. After all, the sooner a child gets rid of spasticity, the greater success can be achieved in preventing complications of the disease. Patients are taken for selective dorsal rhizotomy from the age of three, and for stimulation of deep brain structures – from the age of eight.
“I’ll pay any money, just get me back on my feet!”
- Mom comes from afar. The child is 8 years old and is bedridden. Mom is ready to pay money to any private structures that convince her: “Just give us two or three years, and the child will definitely walk on his own.” And the mother, clutching at this straw, blindly believes in these promises and puts the entire family fortune on the line, sells the apartment and car, anything, takes out loans, they go to these centers and get treatment, but in the end they don’t receive nothing, because there is no way to bypass the patterns of movement.
They come to us, and the mother says: “Teach your child to at least sit.” But if he has level V of global motor functions (the most severe), even this cannot be promised. The only thing that can help is to improve head control, maybe improve hand grip, and increase some of the child’s communicative functions. In such a child, it is necessary to deal with secondary orthopedic problems (scoliosis, hip dislocation, contractures).
When we talk about palliative children, we must understand that the main principle of rehabilitation for them is to feed them, so that they do not starve, so that they gain normal weight, and give the correct position to the body during the day in order to prevent the formation of secondary complications. All rehabilitation should consist of only this.
Forms of cerebral palsy, depending on the affected areas of the brain. Photo neurodoc.ru
The main thing we recommend for such a child is to relieve pain, relieve spasticity, we recommend good technical means and advise good nutrition for the child (in severe cerebral palsy this is a problem). You know, the situation changes immediately in the family, because the child’s mood improves, he stops getting sick, he is fed, he stops breaking down, because we are preventing the usual pathological fractures. And the mother no longer wants to move around the country and the world in search of magical rehabilitation, because she sees a normal, good quality of life for the child.
We try to talk about this classification system with parents, we have schools for parents where we explain it in great detail. Of course, not everyone wants to accept this information, because somewhere inside every parent there is a glimmer of hope that the child will go. And when we determine the level of motor development, and the mother understands what we are talking about, not everyone can immediately accept this information. But they still agree. At the very least, we have clearly reasoned, definite words about what is indicated for this child and what can prevent complications that can lead to suffering and death of the child.
– The question that any mother who has learned about the diagnosis of cerebral palsy in her child probably asks you: can it be cured?
– This is an incurable disease. If you dig deeper, where does cerebral palsy even come from? This is a violation of motion control, primarily a violation of the anti-gravity system. We, living on planet Earth, cannot live without this system. We resist the forces of gravity. There are entire floors in our brain that help us fight the forces of gravity. These are the midbrain, subcortical nuclei, cerebellum, cortex. If all this is intact, then the connections work well, then we are fighting well against the forces of gravity, everything is normal. But as soon as some damage to the brain structures occurs - due to hypoxia, infection, etc., destruction mechanisms can start.
A premature baby developed leukomalacia of the brain, that is, destruction of the brain around the ventricles - this is the white matter, the part of the brain where the paths go, for example, from the cerebral cortex to motor neurons, muscles, and if this path is atrophied, destroyed or even partially collapsed, then high-quality performance of this function can no longer be achieved. That is, cerebral palsy is not a muscle problem, it is a brain problem. If we see serious structural damage in the brain, the first thing that will suffer is the quality of movement.
Cerebral palsy
Cerebral palsy is a polyetiological disease of the brain that can occur during the period of its intrauterine formation, during childbirth and newborns, as well as in the postnatal period.
Delayed brain development can be caused by infectious, toxic-allergic, radiation, ischemic and traumatic factors. The severity of the consequences of their influence on the brain depends not only on the nature of the damaging factor, but also on the duration of its action.
Mothers who gave birth to children with cerebral palsy often experience abnormalities during this and previous pregnancies (fetal asphyxia, miscarriage, prematurity, stillbirth, bleeding, entanglement of the child’s neck with the umbilical cord, leading to brain hypoxia).
Children with cerebral palsy are often born premature, with a low birth weight (700-900 g). All this indicates the leading importance of intrauterine factors in the development of cerebral palsy .
The term “ cerebral palsy ,” proposed by Freud in 1893, implies residual conditions of paralysis that are very different in origin and heterogeneous in clinical manifestations.
Depending on the nature of the paresis, spastic (pyramidal), hyperkinetic (subcortical), ataxic (cerebellar) and mixed forms are distinguished: spastic-hyperkinetic with a predominance of the spastic or hyperkinetic component, spastic-atactic and ataxic-hyperkinetic paresis. Based on the prevalence of motor disorders, they distinguish between monoparesis, paraparesis, hemiparesis (right-sided, left-sided), tetraparesis, etc. Based on severity, they distinguish between mild, moderate and severe cerebral palsy .
Spastic paresis is accompanied by varying degrees of intellectual impairment (from mental retardation to mental retardation).
The degree of intellectual disability can be roughly assessed by the child's ability to learn in a general or specialized school, by his academic performance, age and grade level, or complete learning disability.
Speech disorders include pseudobulbar, hyperkinetic, cerebellar and mixed dysarthria.
Children with cerebral palsy often have hydrocephalus, microcephaly, epilepsy, optic nerve atrophy, hearing loss, diencephalic syndrome, and congenital heart disease (tetralogy of Fallot), which aggravate the severity of cerebral damage.
In newborns, cerebrovascular accident syndrome, hydrocephalic-hypertensive or convulsive syndrome, and inhibition of congenital motor reflexes are often observed.
Therefore, children with cerebral palsy in the postpartum period often require resuscitation measures under the supervision of a neurologist or pediatrician. Postpartum syndromes in children can persist for up to 6 months or more.
Orthopedic treatment for such children can begin only after the elimination of these syndromes.
When choosing a conservative or surgical method for treating joint contractures and deformities of the feet and hands, one should distinguish between contractures and deformities that persist at rest and flexion patterns that occur in the patient’s upright position.
Contractures in joints and deformities are formed by contracted spastic-paretic muscles. Therefore, when determining indications for surgical treatment, it is necessary to identify the muscle that most determines joint contracture and deformity; she is the object of surgical intervention.
The severity of muscle paresis is determined using a 5-point scoring system.
Children with cerebral palsy may develop scoliosis, hip dislocation, and limb shortening, which aggravate the severity of motor disorders and impair their ability to actively move.
Taking into account motor and mental disorders accompanying cerebral syndromes, deformities of the spine and lower extremities, the patient’s ability to move is determined (independently, on crutches, with a stick, with outside help, unable to move and for self-care), on the basis of which the severity of paresis and prognosis are determined treatment.
Treatment methods, especially surgical ones, are most determined by the localization of areas of brain damage, and therefore it is necessary to take into account the clinical characteristics.
- Treatment of cerebral palsy
The rehabilitation center should teach parents
– A child was born, different from the usual one. How to make sure that mom is not left alone with the problem? She doesn't know who to contact. How to make it have a clear action plan?
– I will tell you from the experience of our region. Our mother alone will never be left with this problem, thanks to the fact that there are certain administrative and organizational steps in the work of our medical community.
For example, a child is born with a problem, but how do you know whether this child will have cerebral palsy or a child who simply has some problems?
Before the age of one to one and a half years, a specialist has no right to talk about such a diagnosis, because there is a certain resource for restoring nervous tissue.
We cannot even imagine what level of movement this will be. There may be a problem, but no one can say at what level.
But there is a risk group: if the child was born premature, or full-term, but with a lower body weight than expected, if the child suffered some kind of infection in utero, or after birth he suffered some kind of infection that seriously affects the structure of the brain, for example, meningitis, it can also be a hemolytic disease, according to the A0 system, according to the Rh factor.
We will immediately learn about such children in Tyumen. Having discharged children at risk home, we determine their route; these children must come to us at the state rehabilitation center. Moreover, any mother, if she sees that something is wrong, can contact our center, absolutely free of charge, with a referral.
A commission of doctors at the center, including neurologists, determines whether the child has a problem or whether there is no need to worry. Sometimes we ourselves cannot immediately say whether there will be further problems to some extent, so these children are invited again - in three months. So we observe a risk group from birth.
It happens, of course, that a mother comes for the first time when the child is already a year old. The child has a motor delay, and she says: “Well, maybe it will go away on its own, but the neighbor had the same thing, everything was fine afterwards.” Looking for excuses for himself.
– What is the role of parents in the process of rehabilitation of a child with cerebral palsy?
– It is believed that the most important thing on which the rehabilitation of cerebral palsy is based is movement therapy. It is clear that movement occupies a very important place in life, and a child who has motor problems must engage in movement every day.
But no amount of healthcare will ever be enough to keep children physically active 365 days a year. Parents correctly understand that they need to work with their child constantly, but they think that this should be done by some kind of instructor or physiotherapist. They are looking for more and more rehabilitation courses. Public health care can offer therapy only 1-2 times a year, and parents turn to everyone, including deputies and foundations: “We need a course here, a course here.”
We must change this worldview. The specialist must show how to do this, teach the parents, and the parent must continue the lessons. When a child masters some more advanced movement, the specialist gives new tasks. This is why there is a rehabilitation center, where a specialist tells parents what and how to do.
– Was this the original setting of yours?
- No. And we had a period when we sent children for “treatment,” for example, to Israel. But we understood perfectly well that there was not enough money to send all the children somewhere from the regions. Over time, we came to the conclusion that we need to create something here. Now there is such a trend - the money of the region should remain in the region. This is right.
I have been working at (the official name is the State Autonomous Institution "Children's Psychoneurological Treatment and Rehabilitation Center" - editor's note) since 1992, as a deputy chief physician since 2001. All my scientific activities were devoted to methods of working with cerebral palsy, so here we were able to organize a medical selection committee, when three times a week we see, and children of Tyumen and the region come to us with any problems - orthopedic, neurological, psychopathology, and we select the optimal one rehabilitation route for this child, taking into account the factors that we talked about earlier.
Gold standard in the treatment of cerebral palsy and mental retardation
Author: Luksha Larisa Vasilievna, Ph.D., Chief Physician of CORTEX MC, neurologist of the highest category
The analysis of childhood morbidity and disability shows that the number of children with neurological pathologies is currently increasing. Doctors, psychologists, and teachers note a catastrophic increase in a number of pathophenomena in the child population: an abundance of vascular and musculoskeletal problems; decreased immunity and desynchronosis of various body systems (kidneys, pancreas, biliary systems, brain rhythms, etc.) of the child. A lot of children demonstrate delays and distortions in psycho-speech development and various psychopathological phenomena. The proportion of young patients with cerebral palsy and mental retardation is steadily growing. Therefore, the relevance of rehabilitation of these categories of patients cannot be overestimated.
Cerebral palsy combines a group of motor disorders that occur when the motor systems of the brain are damaged and are manifested in the lack or absence of control by the central nervous system over the functioning of muscles. Cerebral palsy (CP) occurs as a result of damage to the immature brain, which is in a state of maturation in the prenatal period or during early childhood. In cerebral palsy, the interaction between the motor and sensory systems, parts of the motor system itself, and the processes of regulation of voluntary and involuntary movements is severely disrupted. Cerebral palsy is characterized by a violation of higher cortical functions, signs of damage to the pyramidal tracts and subcortical (basal) nuclei, and early organic damage to the motor and speech-motor systems of the brain. Factors leading to structural and functional changes in the brain act in 80% of cases during the intrauterine development of the fetus, in 20% - postnatally: intrauterine infections - influenza, rubella, toxoplasmosis and others, maternal diseases (congenital heart defects, diabetes mellitus, etc. ), immunological incompatibility of the blood of mother and fetus (Rh-conflict), asphyxia of newborns, birth trauma, neuroinfections of the postnatal period (meningitis, meningoencephalitis of various etiologies).
The occurrence of delays in psycho-speech development is also associated with the action of a variety of unfavorable factors in the social environment, as well as with various hereditary influences: constitutional factors, chronic, somatic diseases, organic failure of the nervous system, often of a residual nature, organic causes that delay normal functioning central nervous system (neuroinfections, their complications, brain injuries).
Regardless of the cause that led to brain damage in cerebral palsy or mental retardation , the outcome is the same - different areas of the brain begin to work incorrectly or are not active enough. With cerebral palsy , the motor sphere is more affected - hemiparesis, tetraparesis, but speech and mental development delays are often manifested. With mental retardation , cognitive, behavioral and speech problems come to the fore, but motor clumsiness and underdevelopment of fine motor skills often occur. The pathogenetic basis in both cases is damage to nerve cells (neurons) and pathways of various representations in the brain and spinal cord, which is an important postulate in the creation of therapeutic techniques.
Currently, there are many different areas in the treatment of cerebral palsy : various types of massage and physical therapy, surgical treatment methods, injection with various pharmacological drugs, the use of orthopedic devices, physiotherapeutic procedures, various methods of speech therapy and psychological correction.
What treatment methods exist for delayed psycho-speech development? Drug therapy, reflexology, speech therapy correction, classes with a child psychologist, speech therapy massage, music therapy, occupational therapy, etc. There is no doubt that almost all existing methods make a certain contribution to the treatment of cerebral palsy or mental retardation, but it must be borne in mind that all of them are not radical, but symptomatic (auxiliary), since they do not act on the main pathogenetic link of diseases. All existing approaches to the treatment of mental retardation and cerebral palsy are disjointed and unsystematized, that is, there is no specific standard of treatment that is mandatory and ensures increased efficiency and quality of therapy.
CORTEX Medical Center was founded in 2001 in Moscow and specializes in the treatment of children suffering from various forms of mental retardation and cerebral palsy.
Specialists of the center under the leadership of academicians of the Russian Academy of Natural Sciences Vasilenko F.I. and Razumov A.N. A unique pathogenetic method for the treatment of cerebral palsy and mental retardation - autoneuritotherapy. The method is based on stimulation of the pyramidal motor pathway using a neurophysiological device. For the development of highly effective medical technologies, the activities of CORTEX MC have been awarded diplomas and certificates from Russia and Europe.
In 2014, the methods of pathogenetic therapy were improved and developed into a separate type of treatment - biophysical activation of neuromotor structures. The impact on the motor centers of the brain and spinal cord causes a decrease in the excitability of spinal cord motor neurons that control the activity of the corresponding muscle groups, and pathways that have connections with the thalamus, reticular formation, cerebellum and cerebral cortex are activated. As a result, muscle tone is normalized and body balance is regulated, the center of gravity is stabilized, and the coordinated activity of antagonist muscles is improved. Clinically, this is expressed in the fact that the child begins to sit, stand, and walk. In patients with delays in psycho-speech development, treatment is carried out to activate speech zones (Broca's area, Wernicke's area), areas involved in the control of higher cognitive functions and associative systems of the brain. The child’s speech and memory improve, attention increases, fine motor skills develop, and thinking is activated.
In 2015, the CORTEX MC carried out standardization and unification of treatment processes. in order to improve the efficiency and quality of treatment for patients with cerebral palsy and cerebral palsy . Standards and treatment parameters were developed and approved, which differentiated from the patient’s age and the presence of concomitant pathology. This approach allowed us to develop the Gold Standard for the treatment of cerebral palsy and cerebral palsy, which includes:
— diagnostics — basic neurospecific treatment — complex of auxiliary treatment.
Each patient must undergo a comprehensive, comprehensive examination: examination by a pediatric neurologist, pediatrician, and, if necessary, consultation with a speech therapist; neurophysiological examination of the brain and spinal cord using the latest diagnostic complex for recording EEG and evoked potentials with assessment of the functional maturity of the cerebral cortex; neuroimmunological examination of blood for the presence of antibodies to viruses, specific proteins of the central nervous system, immunogram, which is taken into account when drawing up a treatment program and further prognosis.
The main neurospecific treatment is differentiated depending on the disease, leading complaints and characteristics of clinical manifestations, the patient’s age and his condition at the time of treatment. Therapeutic complexes are developed using scientifically based standards for the intensity and time of exposure to therapeutic factors. The main pathogenetic treatment is always combined with a complex of auxiliary treatment, which includes the most advanced technologies of rehabilitation treatment: anti-gravity kinesitherapy in Atlant suits, differentiated massage, neuroprotective therapy, incl. lymphotropic therapy and endonasal electrophoresis, cerebellar stimulation on a support load simulator “Corvit”, etc. New medical technology for the complex treatment of cerebral palsy and cerebral palsy has a positive therapeutic effect in combination with climatic treatment of the resort city of Anapa.
Standardization of treatment processes at the Cortex MC has made it possible to increase the efficiency and quality of rehabilitation of patients with cerebral palsy and cerebral palsy; the developed treatment complexes make it possible to individualize the treatment process for each patient while maintaining and implementing the Gold Standard of treatment.
The secret of hippotherapy: there is meaning in movement
Photo from the site zdravotvet.ru
– Today, in particular, we are developing hippotherapy. No one will recover from this therapy, but it is a certain type of movement stimulation. If a child, even with a severe level of cerebral palsy, is placed in the saddle of a horse or even without a saddle is placed on a horse, then due to the temperature effect (the horse is hotter than a person), the muscles relax and the child can feel better. Keeping yourself on a horse is always more difficult than just lying on a couch, so anti-gravity mechanisms are activated, these are more shocking inclusions that we cannot achieve in gymnastics, and communication with animals is a positive thing.
Even if a child goes to hippotherapy twice a week, he will have the motivation to move, because without motivation there is no movement.
No movement for the sake of movement! You can extend the elbow joint a thousand times, but the child will never understand why he needs it. And if he reaches for a toy or tries to feed himself, that is, moves for something, this will definitely be fixed in his head and have some practical significance.
– Do mothers always follow your recommendations? And how do you ensure that your mother trusts you, because it is important to trust the doctor.
– First of all, human relationships play a role. Tell me, who would you believe? Why do you choose a person to be your friend? Probably a person should be open, honest and truthful, right?
A patient comes in for an appointment, you must convince the person that what you said is correct. This is difficult to do for a person who does not make eye contact, who is only interested in pieces of paper, and is not interested in people.
If a child with level V is brought in, he lies motionless, and the doctor begins to talk about him in the third person, then he will not be treated as a normal doctor. And we must understand that the child can understand what they are saying.
This is the most important thing - to win over. And if you don’t know your mother’s name, then talking and contacting you is completely useless.
Our relationship with our parents is like that of very good friends. They can call me at any time, I can even talk familiarly somewhere, the process of persuasion is how it should be with your children. But to do this, you need to be very competent, very literate in professional matters.
You must be able to honestly say that the child will not go because of a problem in the hip joint, and when your opinion coincides with what the mother reads in competent sources, it will be worth a lot.
Doctors: good or bad?
– Why do we have “good” and “bad” doctors in Russia? Because there are no standards. For example, the mother of a child with cerebral palsy comes to the doctor for an appointment, and he says, looking at the photo of the hip joint: “Well, everything is fine here, you don’t need to operate.” He comes to another doctor, and he says: “We definitely need to operate!”
Naturally, what is closer to mom, what she wants more, she will choose. But it's not right! There is a certain standard evidence-based criterion that clearly states when surgical treatment is needed. But in Russia such criteria are not used. We have it offhand, because the doctor “thinks like this,” and when mom goes to check with another doctor, he will say that he “thinks like this.” But there cannot be this “I think.” There must be clearly standardized systemic surveillance.
If the index of migration of the femoral head from the acetabulum is more than 40%, then this is a 100% indication for surgical treatment. This has been worked out everywhere in the world. If we see that there is already 40% migration, we honestly tell my mother that after 40% there can be no self-recovery, the whole world has proven this. And when this is not “my opinion,” when this opinion has long been proven by the medical community, the mother has much more confidence.
In our region, every doctor has a mobile application - a Swedish program into which we upload data.
For example, a child of level IV according to the system of global functions, the neck-shaft angle is 150 degrees, the migration index is 35% and he is 8 years old, the computer calculates and gives the result - the situation is stable. You can change any input, for example, enter a different age, the result will immediately change, the risk of dislocation will become 30%. The program will immediately show you what to do with your child.
I give my mom instructions and exercises. Mom comes six months later, shows a new photo and there the migration index is already 40%, I say: “You had 35, and today it’s already 40, did you do what I said?” And the mother answers - no, the child cried and did not give in. I will honestly tell such a mother that this is weakness, her pity harmed the child.
Therefore, the next time mom, having received recommendations, will do everything - write out a daily plan for herself and do it, strictly following the doctor’s instructions. But all this will work when there is evidence, clearly supported by numbers!
And when it’s just “I think,” it will never convince anyone. You like one color, I like another. “I will go to China because the treatment is better there.” There is no better treatment, they do the same thing, only intensively, what a mother, in principle, should do at home herself, that is, 4-6 hours of gymnastics, stretching. This must be prescribed every day, this is a great job for the mother, and there the instructor does it for money. It’s easier to go and do it for money than to do it at home. That's the problem.