3 January 2021
22648
0
3.7 out of 5
Some diseases of the spine, vascular disorders and even endocrine pathologies can provoke the occurrence of such an unpleasant and very detrimental condition as cervical myelopathy. It is accompanied by disturbances in sensitivity and mobility, and can also lead to serious complications. Therefore, it is important to diagnose it in the early stages of development, establish the cause of its occurrence and effectively influence it in order to avoid worsening the condition.
Myelopathy concept
Myelopathy is a comprehensive definition of spinal cord disorders of a dystopic nature and any etiology. It can be a complication against the background of diseases of the spine and joints, vascular degenerative processes, injuries, metabolic or infectious processes, and therefore the final diagnosis should be clarified by explaining the nature of the origin of the disease - ischemic, compression, etc.
The vast majority of myelopathies have an onset outside the spinal substance, as developed against the background of:
- osteochondrosis;
- vertebral fractures;
- spondylosis;
- intoxication (toxins, radiation, etc.);
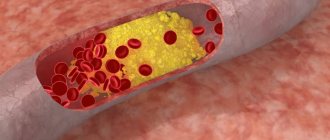
- atherosclerosis;
- diabetes mellitus and other pathologies of the spine, blood vessels and endocrine system.
The following most common cases of myelopathy are caused by direct damage to the spinal substance:
- injuries;
- infections;
- tumor;
- heredity.
As an exception, the disease may develop after a lumbar puncture. The compression type (with compression of the spinal cord) predominates over all others.
Risk factors
Myelopathy due to injury or disease can occur at any age in both men and women. The degree of dysfunction depends on the level of spinal cord damage. Most often, primary spinal cord tumors occur in people aged 30 to 50 years. Spinal cord injuries are more common in men aged 15 to 35 years. Cervical spondylogenic myelopathy is the most common spinal cord injury in individuals aged 55 years and older. People who are exposed to repetitive trauma such as heavy lifting or sports such as gymnastics are at increased risk of developing cervical spondylogenic myelopathy. Patients with existing vascular disease are at greater risk of spinal artery blockages. Patients with multiple sclerosis may also develop symptoms of myelopathy. Incidence: There is currently no accurate information on the incidence of myelopathy. However, information does exist about some common causes of myelopathy. For example, in the United States, between 12 and 15,000 spinal cord injuries occur annually. It is estimated that 5% to 10% of patients with cancer are likely to have tumors growing into the epidural space, resulting in more than 25,000 cases of myelopathy per year, of which 60% will occur in the thoracic spine and 30% in the lumbosacral spine . The prevalence of cervical spondylogenic myelopathy is 50% among men and 33% of women over the age of 60 years. Various tumors can cause compression of the spinal cord, but primary spinal cord tumors are quite rare.
Classification by type
In neurological practice, myelopathy is divided according to etiology:
- spondylogenic – on the spine;
- ischemic – disruption of blood supply to blood vessels;
- post-traumatic – a consequence of mechanical impact with the occurrence of compression on the tissue;
- infectious – for severe bacterial infections (AIDS, syphilis, enterovirus, etc.);
- carcinomatous – against the background of oncology and lesions of the central nervous system;
- toxic – due to intoxication of central nervous system cells or diphtheria;
- radiation – after exposure to radiation (including during the treatment of cancer tumors);
- demyelinating – hereditary or newly acquired demyelization of the central nervous system;
- metabolic - a rare disorder of the metabolism or endocrine system.
Depending on the cause of occurrence, the symptoms of myelopathy may give a different clinical picture.
Treatment
Treatment depends on the cause of the myelopathy. For a fracture or dislocation of the vertebrae - painkillers (analgesics), traction, immobilization for several weeks, and rehabilitation therapy (physiotherapy, exercise therapy, massage). Surgical treatment to correct spinal deformities may involve removing part of the broken vertebra and/or fixing vertebral fragments. Analgesics, NSAIDs, (steroids), and possibly physical therapy may be used to treat arthritis-related problems. Medicines to treat multiple sclerosis may be helpful, including new drugs or steroids. Infections require medications to clear the infection (antibiotics), to reduce fever (antipyretics), and possibly anti-inflammatory drugs (steroids) to minimize inflammation. To treat myelopathy resulting from spinal cord compression, surgery to remove a tumor or herniated disc (laminectomy) may be required.
Forecast
The prognosis depends on the cause of the myelopathy and the presence of permanent damage to the nerve structures. Traction and immobilization can lead to complete recovery if there is no spinal cord injury. Complete cure is also possible for infections. For chronic diseases such as arthritis or osteoporosis, the effect of treatment may be temporary, or if the disease progresses, permanent disability may be possible, including wheelchair use. Spinal cord injury or compression can lead to permanent changes in the spinal cord, including loss of sensation in various parts body, as well as loss of voluntary movements in the limbs. Recovery after tumor removal depends on the residual damage and, if it is a cancerous tumor, on metastasis. Recovery after removal of a herniated disc (discectomy) gives a good result, but only if the spinal cord has not undergone irreversible changes as a result of compression. Complications of myelopathy may include dependence on painkillers, permanent loss of sensation and/or voluntary movement, spinal deformities, and impaired bladder and bowel function.
Symptoms of myelopathic processes
Symptoms of the disease are a series of nonspecific neurological manifestations that poorly reflect the etiological picture. Signs directly depend on the severity of damage to the spinal substance. General symptoms for all types of myelopathies:
- paresis, paralysis, muscle hypertonicity;
- hyporeflexia;
- hypoesthesia;
- paresthesia;
- dysfunction of the pelvic region.
Specific symptoms depend on the type of pathology, the presence of factors inherent in the underlying disease (tumors, infections, fractures, intoxication, etc.) and complications associated with this.
Symptoms of myelopathy
- Pain in the spine in the affected area
- Painful muscle weakness up to paresis and even paralysis (if the cervical and thoracic region is affected, the arms are affected, and the legs are affected in the lumbar region)
- Loss of skin sensation, numbness, paresthesia, or hypersensitivity
- Myalgia (muscle pain)
- Muscle spasms in those limbs that are located below the lesion
- When the cervical spine is affected, in addition to limiting the motor function of the arms, headaches and pain are recorded in the neck, back of the head, shoulder girdles and along the entire length of the arms
- If there is a lesion in the thoracic region, in addition to pain and weakness in the arms, severe pain in the chest is noted, which can even imitate a heart attack
- When the lumbar region is affected, the functions of the pelvic organs (bladder and large intestine, reproductive system) are disrupted.
Diagnosis of the disease
The diagnostic series involves the identification (exclusion) of processes that are symptomatically similar to myelopathy and the detection of factors that provoked dystrophic spinal changes.
Laboratory diagnostics:
- CBC – general blood test;
- BAC – biochemical blood test.
Instrumental examination of the spinal column:
- X-ray;
- MRI;
- EMG – electromyography;
- ENG – electroneurography;
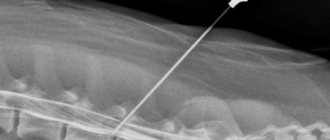
- lumbar puncture;
- angiography (computer or magnetic).
If it is not possible to do magnetic resonance imaging, then it is replaced by discography and/or myelography. The presumed infectious origin of the disease requires additional clinical studies of the biomaterial:
- blood sterility test;
- RPR sample;
- PCR diagnostics;
- culture of a spinal cord fluid sample.
Based on indications, the patient's neurologist can refer him for a consultation with specialized specialists - a vertebrologist, geneticist, oncologist, etc.
Treatment of myelopathy
Therapy is usually conservative, involving long-term drug treatment. If the disease develops rapidly or there is a threat to life, then surgical intervention is resorted to.
The following groups of drugs are used for treatment:
| Analgesics | to eliminate pain syndrome |
| Diuretics | to relieve swelling |
| Antispasmodics and muscle relaxants | to relieve muscle spasms |
If necessary, vasodilators are also used.
Each type of myelopathy requires its own course of therapy, but it is imperative to eliminate the negative impact of the main disease on the spinal cord.
Vascular disorders require:
- Use of vasoactive drugs.
- Application of neuroprotectors and nootropics.
- Compression release.
Collateral circulation is normalized by Papaverine, Euphyllin and nicotinic acid. To improve microcirculation, Flexital and Trental are prescribed. Antiplatelet agents (Dipyridamole-Ferein) are often included in the treatment regimen. Furosemide effectively relieves swelling.
For hematomyelia, anticoagulants (Heparin) are used. Mildronate will help eliminate hypoxia. Be sure to use drugs that improve cognitive function (Galantamine).
For infectious myelopathy, antibiotics must be used. In case of spinal cord intoxication, blood purification is carried out.
Complex treatment of myelopathy can be supplemented with physiotherapy. Many people are prescribed physiotherapy:
- Paraffin therapy.
- UHF.
- Diathermy.
- Electrophoresis.
- Mud therapy.
- Reflexology.
- Electrostimulation.
These procedures, as well as exercise therapy and massage, are recommended only for chronic myelopathy.
Despite proven treatment methods, it is not always possible to get rid of the disease.
Treatment of the disease and consequences
Therapeutic tactics are determined by the etiological and clinical picture. It represents a complex of therapeutic measures to eliminate the causative pathology and symptoms.
The most important goal of treatment of compression type pathology is the elimination of compression pressure. For this purpose, the following activities are carried out:
- removal of tumors, hematomas, Urban wedge;
- cystic drainage;
- laminectomy;
- spinal disc puncture;
- Fasectomy;
- micro- or discectomy (for intervertebral hernia).
The ischemic type of myelopathy is based on the exclusion of compressive conditions of the vessels. Since vascular abnormalities are the cause of most myelopathic conditions, the treatment package for almost all patients includes their therapy with special drugs:
- antispasmodics;
- vasodilators;
- supporting blood supply.
The toxic type requires detoxification procedures, and the infectious type requires effective antibacterial treatment. The greatest difficulty is in the fight against the hereditary type of demyelinating pathology and the carcinomatous type with the presence of hemoblastosis. Most often, treatment measures are aimed at relieving symptoms.
The therapeutic course necessarily includes drugs to increase metabolic processes in cells and reduce the risk of hypoxia - neuroprotective, vitamin, and metabolic agents. The treatment course includes physical procedures recommended by a physiotherapist to increase physical activity, prevent bedsores, etc.
Myelopathy and its classification
Myelopathy is the general name for a complex of diseases that are associated with impaired functioning of the spinal cord.
This important organ is the main axis of the nervous system, through which the brain communicates with other parts of the body. Therefore, this pathology can lead to serious consequences, even disability.
It is not possible to identify a risk group; anyone can get sick, since there are many reasons for the development of the disease.
But you can note the age categories:
- Children who have had enterovirus infection.
- Young people (15-30 years old) who have suffered a back injury.
- Middle-aged people (30-50 years old) with a primary tumor.
- Elderly people (over 50 years old) who have noticed dystrophic changes in the spine.
The development of pathology is preceded by reasons, depending on which the form of myelopathy is diagnosed.
Classification
Spinal myelopathy is divided into separate types. Each pathological process has its own causes, signs and other conventions.
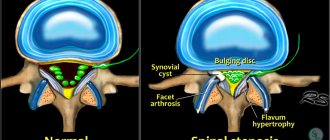
Vertebrogenic. Usually the affected area is the cervical or thoracic region, since they bear increased load. This type of myelopathy causes :
Vertebrogenic myelopathy develops due to the presence of degenerative diseases of the spine
- Presence of osteochondrosis.
- Protrusions and hernias.
- Mechanical damage after bruises or fractures.
- Vascular ischemia.
- Disc displacement, which causes pinched nerve endings.
In the acute form, when the damage is severe, the disease develops rapidly. If the process is sluggish, then myelopathy develops rather slowly.
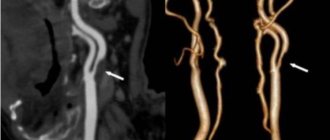
Vascular myelopathy. Pathology occurs due to poor blood circulation in the spinal cord area. The disease affects the spinal arteries and is divided into two types :
Vascular myelopathy occurs if the blood circulation of the spine is impaired
- Ischemic. Blood flow in a separate area of the spinal cord is disrupted, as there is vascular obstruction. The cause is diseases that cause compression of blood vessels.
- Hemorrhagic. Hemorrhage occurs because the integrity of the vessel is compromised.
Spinal cord infarction. The danger is that severe damage can occur in any area of the spine. The consequences are almost impossible to predict. The main cause is a blood clot. This damages the nerve fibers, leading to loss of sensation in the limbs and decreased control of muscle reflexes.
Cervical myelopathy. The pathological process usually develops with age, when changes in cartilage and bone tissue begin. It occurs in the cervical region due to compression of the spinal cord in this area. There is a separate form - cervical myelopathy. Pathology with more serious symptoms (upper limbs are not controlled).
Chest. The name indicates the location. Development is facilitated by a hernia, narrowing or pinching of the spinal canals.
Lumbar. Characterized by certain symptoms:
- If there is compression between the 10th, 11th, 12th thoracic and 1st lumbar vertebrae, then epiconus syndrome develops. Sharp pain appears in the lumbar region and back of the thighs. There is weakness in the lower extremities and paresis of the feet. Achilles and plantar reflexes also disappear.
- When compression is observed in the area of the 2nd lumbar vertebra, conus syndrome begins to develop. With mild pain, changes appear in the rectum and genitourinary system, and the anogenital area also suffers. Bedsores quickly form and the anal reflex is lost.
- If, in addition to the 2nd lumbar root, the discs located below this vertebra are also subjected to compression, a “horsetail” occurs. Unbearable pain appears in the lower part of the body, radiating to the legs.
Compression-ischemic
Compressive myelopathy occurs due to pressure on the spinal cord. More on this below
This type includes a wide range of diseases:
- Cervical spondylosis, which occurs due to wear and tear of the discs, as well as their displacement.
- Malignant neoplasm.
- Purulent inflammation.
- The spinal canal has narrowed. This defect can be congenital, but is more often caused by inflammation or destruction of the vertebrae.
- Hemorrhage in the spinal cord.
- A disc bulges when it pushes into the spinal canal.
Compression is accompanied by the slightest injury if the integrity of the vessel is compromised.
Spondylogenic. The condition progresses due to injury to the spinal cord due to the constant awkward position of the head. The posture and gait of a person gradually changes.
Degenerative. Its appearance is caused by vitamin deficiency, as well as the progression of spinal cord ischemia.
Focal myelopathy. It is a consequence of irradiation or the penetration of radioactive substances into the body. Accompanied by hair loss, inflammation of the skin and brittle bones.
Discirculatory. It is always chronic. The muscles of the limbs weaken, their sensitivity decreases. Sudden muscle contractions appear, and organ dysfunction in the pelvic area begins to occur.
Discogenic. There is another name - vertebral myelopathy. It often develops due to a long process of degeneration of intervertebral discs and is considered an independent disease. Disc herniations occur, compressing the spinal arteries and brain.
Progressive. The cause of this type is Brown-Séquard syndrome. The disease affects almost half of the spinal cord (in cross section) and can cause paralysis. Usually the pathology develops rapidly, but sometimes it lasts for many years.
Chronic. There are many reasons for the development of this type of myelopathy:
- Poliomyelitis, usually leading to paralysis.
- Cirrhosis of the liver.
- Infectious diseases affecting the spinal cord.
- Syringomyelia. Small cavities form in the spinal cord.
- Syphilis.
- Various pathologies of the spine.
In fact, all forms of myelopathy can be classified as chronic if their development does not progress.
Post-traumatic. The designation of the disease indicates the cause of the development of the pathology. Has typical symptoms:
- Disorders in the pelvic area.
- A sharp decrease in sensitivity.
- Paralysis.
Usually such signs remain for life.
There are many variants of spinal cord disease, so you should always keep in mind the possible presence of myelopathy.
Video: “What is myelopathy?”
Find out what infectious diseases of the spine there are:
- You can read more about the diagnosis of tuberculous spondylitis at this link
- You can find out what spinal osteomyelitis is here
- Is it possible to cure spinal discitis with antibiotics? The following article explains
- familiarize yourself with the clinical picture of inflammation of the spinal cord by going to the page
- How dangerous is a spinal epidural abscess?
- Symptoms and treatment methods for spinal spondylodiscitis
Forecast and preventive measures
The prognosis for compression myelopathy is quite satisfactory if areas of tissue compression are detected and eliminated on time. If the disease is ischemic in nature, progression of the disease is possible, but regular therapeutic courses on blood vessels provide stable remission. For the radiation, carcinomatous, hereditary type, the prognosis is usually unfavorable.
To prevent myelopathic processes, it is necessary to prevent and promptly eliminate any disorders associated with vascular and spinal disorders.
You can undergo diagnostics and establish the exact cause of the disease, and receive recommendations for a course of treatment at our medical center. Specialists of the Consultative and Diagnostic Center (formerly the National Diagnostic Center) will help you cope with the developing disease. Click the “SIGN UP” button or call the numbers listed on the website and come see us.
1.What is myelopathy
Myelopathy is a conduction disorder of the spinal cord of inflammatory, traumatic, tumor or vascular origin. Most often, the spinal cord is only partially affected in some area, so the disease is sometimes detected accidentally during MRI diagnostics. In more severe cases, severe symptoms force the patient to consult a surgeon and undergo a thorough examination.
The background for the development of myelopathy can be systemic diseases, in which case the diagnosis acquires the appropriate prefix (diabetic myelopathy, ischemic myelopathy).
The classification of myelopathies correlates this pathology with one of the following conditions:
- non-embolic spinal infarction;
- acute embolic spinal infarction;
- spinal edema;
- subacute necrotizing myelopathy;
- thrombophlebitis and non-pyogenic phlebitis of the spinal cord;
- spinal compression;
- spinal bladder;
- radiation myelopathy;
- drug myelopathy.
Most often, the focus of myelopathy is localized in the cervical region. Thoracic and lumbar myelopathy is a much rarer occurrence.
A must read! Help with treatment and hospitalization!
The main factors in the manifestation of discogenic myelopathy
Degenerative type anomalies that appear during the formation of spinal osteochondrosis most often lead to stretching or rupture of the fibrous element, and peripheral particles are torn off from the membranes of the vertebrae. This phenomenon causes disc displacement with the formation of a hernia. In the case when the fibrous ring does not rupture, the disease has a different name - “protrusion”, and in case of violations and the pulpous interior comes out - “extrusion”. Typically, deformations begin in the posterolateral area, this is where the spinal cord and vessels through which blood cells are transported pass.
The mechanism of occurrence may be disruptions in the functioning of blood circulation in the spinal region, formed as a result of pressure on the vertebral arteries by a hernia of enormous size. The ischemic stage is distinguished by step-by-step stages of development and develops into a chronic disease. In addition, the cause of the anomaly may be an unfavorable process of adhesions after undergoing spinal surgery or injury.
Osteophytes that appear during osteochondrosis become aggravating sources, which have an additional compressive effect on many areas. If blood circulation decreases due to compression of blood vessels and the spinal cord, then such actions cause hypoxia and disruption of cell trophism. Next, the destruction of nerve elements begins, subsequently causing the main clinical picture of the described disease.
Discectomy and microdiscectomy
More radical treatment methods that are advantageously used to eliminate large hernias are discectomy and microdiscectomy. Both operations involve partial or complete removal of the intervertebral disc.
After surgery, the patient needs a long recovery period. Rehabilitation treatment is aimed at the complete restoration of lost motor functions. Today, many different rehabilitation techniques are used to recover from discogenic myelopathy: classical and myofascial massage, electrical stimulation, physical therapy, mud therapy, reflexology, hydrotherapy (radon, hydrogen sulfide and pine baths). Rehabilitation treatment also involves taking medications such as chondroprotectors, metabolites, B vitamins, and vascular drugs.
Cervical myelopathy - what is it?
The main causes of damage to the spinal cord of the cervical spine:
- Violation of spinal microcirculation;
- Intervertebral hernia;
- Inflammatory processes;
- Degenerative-dystrophic changes in the neck;
- Bone destructive damage;
- Compression syndrome;
- Fractures and dislocations of the cervical spine;
- Injuries of the cervical vertebrae;
- Autoimmune processes with damage to the nerve fibers of the cervical plexus (neuromyelitis, transverse myelitis).
Cervical myelopathy of the spinal cord is associated with the occurrence of muscle and ischemic syndromes. Vessels pass through the cervical region, supplying blood to a quarter of the brain. Vertebral artery syndrome (vertebrobasilar) often accompanies spinal changes.
It is not always possible to determine the causes of spinal myelopathy of the cervical spine.
Provoking factors of cervical damage:
- Violation of microcirculation of the neck;
- Infectious processes;
- Ischemic conditions (associated with a lack of oxygen supply);
- Narrowing of the spinal canal at the level of the cervical spine;
- Excessive physical activity with deformation of the vertebral segments, hyperextension of the articular-ligamentous apparatus.
Symptoms of the disease are nonspecific:
- Muscle weakness;
- Pain syndrome of the upper limb;
- Dizziness;
- Impaired walking, unsteady gait;
- Urinary incontinence;
- Problems digesting food.
Spinal nerves extend through the cervical spine, providing innervation to the arms, base of the skull, chest, esophagus, and trachea.
Causes of myelopathy
Myelopathy is a disorder of the spinal cord, most often due to one of several reasons:
- Compression (prolapsed disc herniation, bone growth, displaced vertebra, vertebral fragment);
- Poor circulation of the spinal cord (blockage, narrowing or congenital anomaly of the arteries of the spinal cord, spinal stroke);
- Previous trauma (bruise, spinal fracture, surgery);
- Inflammation of the vertebrae or spinal cord (spinal arachnoiditis, myelitis).
- Complication after spinal puncture.
Spinal cord compression at the level of the 5th and 6th cervical vertebrae
Signs of myelopathy of the lumbar and thoracic regions
Clinical signs of myelopathy depend on the location of the compression site and the degree of damage to the spinal cord structures. Acute post-traumatic myelopathy of the thoracic level manifests itself in the form of severe pain between the shoulder blades, spreading along the costal arches. It is difficult for a person to breathe; a rapid heartbeat and a change in its rhythm may occur. A dry, paroxysmal cough appears, and hiccups may occur due to irritation of the vagus nerve.
Chronic myelopathy of the lumbar vertebra manifests itself in the form of the following clinical symptoms:
- constant dull pain in the lumbar and sacrum areas;
- it can spread along the sciatic nerve to the thighs and legs;
- numbness of the lower extremities and a feeling of muscle weakness;
- rapid fatigue of the leg muscles when walking and climbing stairs;
- paresthesia, sensation of crawling in the legs and in the sacral area;
- bladder dysfunction (hyperactivity, urinary incontinence, urinary retention);
- persistent constipation followed by diarrhea;
- decreased libido and erectile dysfunction in men;
- impaired reproductive ability in women.
An MRI examination and x-ray will help confirm a preliminary diagnosis of myelopathy. In rare cases, cerebrospinal fluid and cerebrospinal fluid are collected to analyze their chemical and cellular composition. This examination is necessary to exclude infections, internal bleeding and a number of other pathologies.