Every year in Russia, about 600 thousand people suffer traumatic brain injury (TBI). 50 thousand of them die, and another 50 thousand become disabled. The incidence of TBI in men is twice as high as that in women, with this relationship maintaining in all age groups.
The most common causes of TBI
Typical clinical manifestations of traumatic brain injury.
TBI is characterized by a three-phase change in consciousness: a primary short-term loss of consciousness at the time of injury, subsequent recovery ( light interval ) and, after a certain period of time, repeated loss of consciousness . However, such a classical development of changes in the state of consciousness is not always observed. Often there are cases that occur without a light gap, or it is erased. Sometimes there may be no primary loss of consciousness. The duration of the clear interval (both with full and partial restoration of consciousness) in most patients with acute EDH is measured in several hours or even minutes.
Patients who have suffered a trauma and are accessible to contact usually complain of a headache with increasing intensity. In many cases, the headache has a bright shell-like hue, radiates to the eyeballs, jaws, and is accompanied by photophobia, hyperesthesia with characteristic facial reactions. The headache is usually constant with periodic crisis-like exacerbations, often accompanied by repeated vomiting . In severe pain, victims moan, demand help, grab their heads with their hands, toss in bed, and lose sleep.
After a traumatic brain injury, patients often experience bradycardia (in almost 1/2 of patients, the pulse rate does not exceed 60 beats per minute); in approximately 1/4 of the observations, an increase in maximum blood pressure above 150 mm Hg is noted. Art.
In victims with traumatic hematomas, it is almost always possible to identify one or another focal symptomatology . Among the signs of damage to the cerebral hemispheres, the first place belongs to motor disorders (weakness in the arm and leg, most often opposite the side of the hematoma). The severity of these disorders varies - from anisoreflexia to hemiplegia (paralysis).
Occasionally, the clinical picture of intracranial hematomas includes symptoms of irritation of the cerebral cortex in the form of general or focal epileptic seizures .
Among craniobasal symptoms, the most important role in the clinic of TBI is given to the dilation of one pupil with a decrease or loss of its reaction to light .
Clinical classification of TBI.
According to the clinical picture, traumatic brain injury is divided into:
1. Focal • brain contusions (mild, moderate, severe), • intracranial hematomas (epidural, subdural, intracerebral), • subdural hygromas, • depressed fractures, • head compression;
2. Diffuse • concussion, • diffuse axonal damage, • subarachnoid hemorrhage.
Diagnostics.
Currently, the gold standard when examining patients with traumatic brain injury is the following set of examinations: 1. Clinical examination by a neurosurgeon. 2. X-ray of the skull in two (at least) projections. 3. Echoencephalography. 4. CT (computed tomography) of the brain. The issue of additional examination methods is decided individually.
Very often, epidural hematomas are accompanied by a fracture of the skull bones.
Types of intracranial hematomas.
Brain contusions include focal macrostructural damage to its substance as a result of trauma. According to the unified clinical classification of traumatic brain injury adopted in Russia, focal brain contusions are divided into three degrees of severity: 1) mild, 2) moderate, and 3) severe.
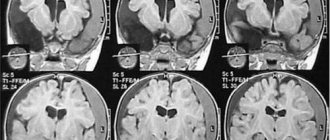
| CT scan of the brain. Severe brain contusion, intracerebral hematomas of both frontal lobes. |
Epidural hematomas are a collection of blood caused by trauma, located between the inner surface of the skull bones and the dura mater, causing local and general compression of the brain.
The frequency of epidural hematomas among observations of initially hospitalized victims with TBI varies widely from 0.54% to 9%.
Causes of epidural hematomas. A temporary local deformation of the skull that occurs during an injury, often with a depressed fracture of the skull bones and rupture of the vessels of the dura mater, leads to the release of blood from the damaged vessel, which, exfoliating the dura mater, spreads within the cranial sutures, where the shell is tightly fused with the internal bone plate. For this reason, epidural hematomas have a smaller area of distribution and greater thickness than subdural hematomas.
| CT scan of the brain. Acute epidural hematoma in the left occipital region with brain dislocation and compression. |
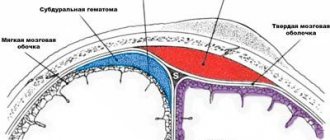
Subdural hematomas are a volumetric accumulation of blood caused by trauma, located between the dura and arachnoid maters and causing local and general compression of the brain.
Subdural hematomas are more common than epidural hematomas. Isolated SDH accounts for approximately 2/5 of the total number of cases of brain-compressing intracranial hemorrhages; they occupy first place among various types of hematomas.
| CT scan of the brain. Acute subdural hematoma in the right fronto-parietal-temporal region with brain dislocation and compression. |
Post-traumatic chronic subdural hematomas are encapsulated volumetric hemorrhage located under the dura mater and cause local and general compression of the brain. The incidence of these hematomas ranges from 2 to 13 cases per 100,000 population per year, increasing significantly in elderly and senile people.
Chronic subdural hematomas differ from acute and subacute traumatic hematomas by a demarcation capsule that usually appears 2 weeks after the injury, which determines all the features of their pathogenesis, clinical course and treatment tactics. The volume of CSH ranges from 50 ml to 250 ml and is more often 100-150 ml.
If previously chronic subdural hematomas were detected exclusively in elderly and senile people, now they have become significantly “younger”, occurring quite often in young and middle-aged people, as well as in children.
The distinctive clinical sign of these hematomas is that the clear interval can last for weeks, months and even years. Clinical manifestation is extremely polymorphic. There is both a gradual development of compression syndrome and a sudden sharp deterioration in the patient’s condition to stupor and coma, spontaneously or under the influence of various additional factors (mild repeated head injury, overheating in the sun, alcohol consumption, colds, etc.).
The clinical picture may resemble various diseases of the central nervous system: benign and malignant brain tumors, etc. During the period of a detailed clinical picture of chronic subdural hematoma, changes in consciousness in the form of stupor or amentive confusion with impaired memory and orientation are frequent.
| CT scan of the brain. Bilateral chronic subdural hematomas. |
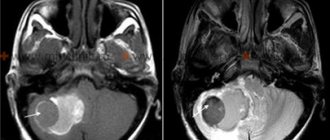
Damage to the structures of the posterior cranial fossa (PCF) is one of the severe types of traumatic brain injury (TBI). Their peculiarity lies in their extremely difficult clinical diagnosis and high mortality. Before the advent of computed tomography, the mortality rate for PCF injury was close to 100%.
The clinical picture of damage to the structures of the PCF is characterized by a severe condition that occurs immediately after the injury: depression of consciousness, a combination of cerebral, meningeal, cerebellar, and brainstem symptoms due to rapid compression of the brainstem and impaired cerebrospinal fluid circulation. If there is significant damage to the substance of the cerebrum, hemispheric symptoms are added.
The proximity of the location of damage to the PCF structures to the liquor-conducting pathways causes their compression and disruption of liquor circulation by a small-volume hematoma. Acute occlusive hydrocephalus, one of the most severe complications of damage to the structures of the posterior canal, is detected in 40%.
Treatment.
All patients with clinical signs of compression of the brain, as well as when this compression is detected on CT or MRI in severely ill patients, are advised to undergo urgent surgery - removal of the hematoma.
Diagnosis and clinical manifestations
If you suspect the appearance of a chronic subdural hematoma, you should contact a neurosurgeon or neurologist. The examination includes a thorough examination, which involves assessing the nature of the injuries received and performing an X-ray of the skull. An additional diagnostic method is ophthalmoscopy.
Experts detect atrophic processes in the stagnant discs of the visual nerve structures in the fundus. But the main examination methods are computed tomography and magnetic resonance imaging of the brain. The first research method is the most preferable and informative.
2. Mechanism of occurrence of subdural hematomas
Such hematomas, as a rule, occur due to a sharp inertial displacement of the brain that occurs during a strong blow to the head
. This can happen during a traffic accident, a fall from a height, an awkward fall on your back followed by hitting your head on the asphalt, for example, during icy conditions, etc. In this case, a rupture of the bridge veins flowing into the superior sagittal sinus occurs.
A similar injury can also occur in the absence of a direct impact with the head on a hard surface - sometimes a fall or an unsuccessful jump from a height to one’s feet, a sudden movement of the head during sudden braking of a vehicle, etc. is sufficient.
A subdural hematoma can also occur on the side of the head opposite to the blow in the event of an impact with an object that has a large surface area - an ice block, a log, a car side, etc.
Visit our Neurosurgery page
Retrochorial hematoma - what is it?
Limited accumulation of blood between the chorion (fertilized egg) and the wall of the uterus creates a risk for bearing a child. Pathology is diagnosed using ultrasound in the first trimester of pregnancy. The cause of the condition is rejection of the chorion from the wall with rupture of blood vessels. Gravidar (retrochorial) hematoma is not related to traumatic brain injury, but is diagnosed with an MRI scan. At the beginning of development, dark red discharge appears from the woman’s vagina. In combination with pain in the lower abdomen, the pathology causes dangerous symptoms. After physical exertion, the manifestations intensify.
The nosology can be asymptomatic and detected after the birth of the child. The size of education plays a significant role.
After the blow, external hematomas appear on the head, leg, and torso. In the early stages, the lesions have a brown color due to rupture of arterial vessels. Tricks are not dangerous if the bleeding has stopped. After a few weeks, the lesions turn purple, then yellow. The color range is explained by the phases of breakdown of hemoglobin in red blood cells. The extent of damage can be determined by the intensity of the skin in the area of hemorrhage.
Possible complications and consequences of epidural hematoma
The consequences of an epidural hematoma are:
- Chronic fatigue syndrome
- Depression
- Speech Impairment
- Neuroses, psychoses
- Decreased memory and mental activity
- Numbness, paralysis of limbs
- Convulsions
Epidural hematoma. CT, axial slice. Convex hyperdense formation adjacent to the calvarium. Sutures serve as a natural barrier to epidural hematomas, since in these areas the dura mater of the brain is tightly attached to the calvarium (a). Epidural hematomas usually occur at the fracture site (b).
Treatment of intracerebral hematoma in CELT
Treatment of hematomas is carried out using conservative and neurosurgical techniques. Their choice depends on the diagnostic results and individual patient indications.
| Hematoma treatment methods | What is? |
| Conservative | Indicated for patients who have maintained clarity of consciousness with hematomas up to 30 mm and no signs of compression of the medulla oblongata. Treatment involves the administration of drugs that reduce the permeability of vascular walls. The procedure is carried out under the control of computed tomography. |
| Neurosurgical | Suitable for large hematomas with pronounced focal symptoms. Depending on the situation, the following removal methods are used:
If there are multiple hematomas, as a rule, only the largest ones are removed. |
The Department of Neurology at CELT sees neurologists and neurosurgeons with many years of experience in scientific and practical work. You can make an appointment with them online on our website or by contacting our operators: +7 (495) 788 33 88.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
3. Symptoms of the disease
The manifestations of a subdural hematoma are very diverse, but among the most basic symptoms of a subdural hematoma the following should be noted:
- severe headache, feeling of fullness;
- the presence of a “light” gap for some time after the injury;
- psychomotor agitation (euphoria, ridiculous behavior, loss of control over the pelvic organs);
- vomit;
- pain when moving the eyes, photophobia;
- in severe cases, loss of consciousness, respiratory rhythm disturbances, convulsions.
Of course, the above symptoms can only signal the presence of a hematoma, and only a thorough diagnosis carried out within the walls of a medical institution will make it possible to make an accurate diagnosis with absolute certainty and immediately begin appropriate treatment.
About our clinic Chistye Prudy metro station Medintercom page!