Multiple sclerosis
(MS) is a chronic, incurable autoimmune disease. Pathological processes (demyelination) affect the myelin sheaths of neurons in the brain and spinal cord. Healthy tissue is replaced by dense connective tissue, the scar type. It does not conduct nerve impulses, which leads to various neurological symptoms.
Diagnosis of multiple sclerosis at the initial stage of the disease is difficult. It is important to have complete, regular medical checkups. In this case, it is possible to detect the onset of the disease and begin timely treatment. This will help to significantly slow down pathological changes and prolong the patient’s ability to work for a long time.
tests
Causes of multiple sclerosis
At the moment, the exact cause of the disease has not been established. Some of the most likely factors influencing the development of MS are:
- previous viral or bacterial infections;
- prolonged exposure to increased radiation fields;
- chronic poisoning with toxic substances;
- poor quality, inadequate nutrition;
- unfavorable environmental conditions;
- previous injuries;
- frequent stressful situations.
According to statistics, the disease most often occurs at a young age, under 40 years of age. However, it is rare, but still occurs both in children under 15 years of age and in older people. It is more often diagnosed in females; there are female patients for every male. Not only gender matters, but also race. Caucasians are more prone to multiple sclerosis.
The incidence is higher in large, industrial cities, which may indicate the influence of unfavorable environmental conditions and stress. Russia is a high-risk zone, since more than 30 patients are diagnosed here for every 100 thousand people.
Manifestation of multiple sclerosis
Symptoms depend on the location of the most severe demyelination.
1. If the pyramidal system is damaged:
- Increased tendon-periosteal reflexes that occur in response to stimuli.
- Decreased muscle strength and increased muscle fatigue while maintaining functionality.
- Tetraparesis is increased tone of a particular muscle group.
2. With damage to the cerebellum:
- Ataxia (impaired coordination of movements) of the trunk and limbs.
- Intention tremor (vibrations of the whole body or its parts due to uncontrolled muscle contractions).
- Muscular hypotonia (decreased muscle tone and strength up to paresis).
3. When neurons are damaged, paralysis of the following nerves may occur:
- facial;
- oculomotor;
- sublingual;
- trigeminal nerve.
4. Other symptoms of MS:
- bulbar and pseudobulbar syndromes;
- nystagmus - involuntary eye movements;
- joint and muscle pain;
- loss of tactile sensitivity;
- a feeling of pressure in the limbs;
- superficial tingling in the fingers;
- incontinence and retention of urine and bowel movements;
- sexual dysfunction;
- decreased visual acuity and quality (loss of brightness, distorted color perception).
Neuropsychological changes are also observed in multiple sclerosis. They consist in changing habits, reducing mental abilities, resulting in specific organic dementia. Patients suffer from depression, alternating with periods of euphoria, and often lose control of their emotions. Emotional instability, i.e. rapid changes in mood, which is considered one of the early symptoms. To assess the severity of symptoms, a scale from 0 to 6 is used, and the degree of disability of a patient with MS is scored from 0 to 10 on the EDSS scale.
Symptoms and manifestations
The development of the disease can be slow or rapid - it depends on the form. In the case of the second option, the patient has a better chance of seeking help in a timely manner. If sclerosis progresses slowly, patients do not pay attention to the deterioration of their health for a long time.
The most characteristic symptoms of multiple sclerosis:
- Increased fatigue, loss of muscle strength. As the disease progresses, paresis appears. As a rule, symptoms are more pronounced in the lower extremities. Neurological examination revealed reflex disturbances. Dystonia, hypotension.
- Loss of coordination. It manifests itself individually - one person experiences dizziness, handwriting becomes worse, and hand tremors appear. Some people have problems with gait. As the disease progresses, the symptoms intensify and motor function is severely impaired.
- Speech disturbances arise with the development of the disease - at first, chanting of speech is clearly manifested.
- Optic nerve disorders – double vision, nystagmus, strabismus. Disorders of the trigeminal and facial nerves may be observed.
- Loss of sensation is a symptom that, along with motor dysfunction, strongly suggests multiple sclerosis. Parts of the face and limbs go numb. There may be tingling sensations in the muscles.
- Frequent or infrequent urination, frequent or decreased urge to defecate.
- Impotence, decreased libido.
- Changes in the intellectual sphere - decreased memory, concentration, ability to analyze. The patient quickly gets tired when solving intellectual problems and has difficulty switching.
- Psychological disorders – depression, anxiety, nervousness, euphoria.
Symptoms may manifest differently, depending on where the plaques are located in the central nervous system. If you observe several of the listed factors in yourself and or in one of your loved ones, be sure to consult with an experienced neurologist!
Diagnosis of multiple sclerosis
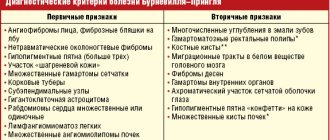
The disease does not have characteristic symptoms unique to it. Therefore, differential diagnosis is always carried out. The doctor needs to rule out a large number of congenital pathologies and diseases of the nervous system. Systemic lupus, stroke, Sjogren's syndrome, Parkinson's and Behçet's diseases have similar changes.
1.
Laboratory diagnostics
When conducting a general blood test, changes in indicators allow one to suspect the development of multiple sclerosis. These include:
- Concentration of lymphocytes - increased content up to 40% or more.
- The number of leukocytes is less than normal.
- Erythrocyte sedimentation rate is increased.
A cerebrospinal fluid puncture will help check for an autoimmune disorder. In MS, a high percentage of immunoglobulins and oligoclonal antibodies (IgG antibodies) will be detected in it.
You can analyze the state of the immune system by doing an immunogram. To do this, it is necessary to donate venous blood for a comprehensive study. It is aimed at identifying the concentration of lymphocytes and immunoglobulins of various types. As a rule, with RSV, the concentration of immune cells is increased, indicating an autoimmune process, and other parameters are decreased, as a result of weakened body defenses.
2. Instrumental diagnostics
The most effective at the moment is considered to be an electromagnetic superposition scan of brain structures (SEMS) or an electroencephalogram. The scan allows you to diagnose multiple sclerosis at an early stage of development, when neurological signs are absent or mild. However, SPEMS has a high error; changes are detected in one case out of three.
The essence of the method is to identify focal losses of myelin. In the presence of pathological changes, the conduction of nerve impulses is disrupted. It is carried out by placing several sensors that monitor bioelectric impulses on the patient’s head. The result is an electroencephalogram - a graphic image of an oscillatory electrical process.
3. Magnetic resonance and computed tomography
Computer and magnetic resonance diagnostics make it possible to assess the state of the nervous system and diagnose MS. The use of a contrast solution helps to increase the efficiency of the study. The drug is administered intravenously and does not cause any sensations or discomfort.
The sensitivity of tomography is extremely high, reaching an accuracy of 95%. Allows you to accurately diagnose multiple sclerosis in the following cases:
- detection of 4 or more foci of demyelination;
- diameter of damage to nerve fibers from 3 mm;
- the lesions are located in the nerve fibers, in the cranial fossa, adjacent to the lateral stomachs.
A contrast solution not only helps to increase visibility, but is itself a marker of the presence of pathology. Its accumulation in the lesions indicates an active inflammatory process. A tomogram of the spinal cord is performed in the same way.
Multiple sclerosis (MS) is the most common inflammatory demyelinating disease of the central nervous system. Despite many years of studying MS, there is still not a single pathognomonic sign of it. In this regard, the search for specific biomarkers in MS is currently an urgent task not only in clinical medicine, but also in neurobiology.
Biomarkers are measurable and quantifiable parameters (for example, the concentration of an enzyme, the distribution of a gene phenotype in a population, the presence of certain substances in biological fluids) that serve to assess physiological and pathological processes in the body, such as the risk of disease, exposure to environmental factors and its influence, diagnosis of the disease, metabolic processes, etc.
Currently, there is an active search for biomarkers of MS that can predict and assess the rate of progression of the disease, help determine treatment tactics and evaluate its effectiveness, clarify the largely unexplored pathogenesis of the disease, and, finally, identify new targets for therapy. In addition, given the nonspecificity of the clinical manifestations of MS, diagnostic markers are also being studied to identify the disease at an early stage of development and promptly begin pathogenetic therapy and identify risk groups for MS [42].
At the moment, no biomarkers with sufficient sensitivity and specificity have been identified for MS. To date, in demyelinating diseases, a specific marker known only for neuromyelitis optica (OM) is antibodies to aquaporin-4 (Aqp-4). Their identification makes it possible to differentiate Devic's neuromyelitis optica from other diseases of the nervous system. Detection rates vary across studies and are likely to depend, among other things, on the ethnicity of the patient population studied.
The search and validation of MS biomarkers is due to the complexity and heterogeneity of the pathogenesis of this disease. Immunochemical research methods have revealed that the formation of demyelination plaques does not occur in the same way in different patients. Four main morphological types (patterns) of demyelination in MS have been identified. Pattern I is characterized by intense macrophage infiltration, prevailing over T-lymphocyte infiltration. Immunoglobulins dominate in pattern II plaques, and C9neo antigen is also detected in large quantities. For plaques of patterns I and II, a common feature is the destruction of all myelin proteins. Features of pattern III include predominant destruction of myelin-associated glycoprotein (MAG) in the distal parts of oligodendrocyte processes and fragmentation of oligodendrocyte nucleoli. This pattern of demyelination in its cytological characteristics is very similar to changes in the white matter during ischemia. Pattern IV plaques describe primary oligodendrocyte degeneration with uniform destruction of all myelin proteins and fragmentation of genetic material.
Thus, histoimmunochemical studies confirm the heterogeneity of the pathogenesis of MS and dictate the need to take into account that the set of biomarkers characterizing the properties of the pathological process with different mechanisms of demyelination can also be heterogeneous.
Markers of inflammation.
The inflammatory response in MS is one of the central links in pathogenesis. It is believed that the first stage in the development of the inflammatory reaction is the activation of lymphocytes with encephalitogenic potential and their penetration into the central nervous system through the blood-brain barrier (BBB). According to current concepts, activation of lymphocytes is associated with disruption of immune homeostasis and the influence of additional exogenous signals, primarily due to constant exposure to bacterial and viral antigens. As they migrate across the BBB, they express metalloproteinases and various cytokines and are reactivated by fragments of myelin antigens, which leads to a further increase in the release of biologically active molecules and the progressive development of an inflammatory response in the central nervous system. Additional damaging factors are toxic mediators actively produced during inflammation, such as nitro compounds and reactive oxygen species. In addition, there is activation of B lymphocytes and increased production of antibodies against myelin components, which determine the development of demyelination, which has been shown both in experimental models and in humans [6].
Biomarkers detected in the blood and CSF of patients with MS are a reflection of the described reactions. Activation of the process is indicated by changes in the levels of cytokines, adhesion molecules, migration and other markers that reflect the current inflammatory reaction and disruption of the integrity of the BBB in the biological fluids of MS patients. A number of studies have noted an increase in pro-inflammatory cytokines TNF-α, IFN-γ, IL-6, IL-23, IL-2, IL-1β, IL-17, CXCL12, CXCL13, IP-10, CCL-5, etc. , adhesion molecules sICAM, sVCAM, VLA-4, LFA-1, etc., as well as matrix metalloproteinases MMP2, MMP8 and MMP9 during an exacerbation. At the same time, a decrease in the levels of other cytokines, such as IL-4 and IL-10, was detected. The relationship between the levels of these molecules has been shown both with the clinical activity of the disease and with the number of contrast-accumulating foci on magnetic resonance imaging (MRI). However, in other studies, no significant changes in cytokine concentrations were noted in MS. In this regard, it was concluded that changes in the levels of pro-inflammatory cytokines are a nonspecific phenomenon that is observed both in MS and in other inflammatory diseases of the nervous system [5, 18, 32, 53, 54, 58, 59, 73, 75] . Quite a lot of research has been devoted to studying changes in the levels of proinflammatory cytokines in response to treatment. When treated with interferon-β drugs, there was a decrease in the levels of TNF-α, IFN-γ, VLA-4, and an increase in IL-4, IL-5, IL-10, CCR-7 [14, 48, 64, 65]. When treated with methylprednisolone, there is a decrease in the levels of VLA-4, LFA-1, VCAM-1 and E-selectin [16]. After natalizumab therapy, the levels of IL-1β, IL-6, IL-8, CXCL9, CXCL10, CXCL11, and CCL22 decreased [49].
The activation of B lymphocytes in patients with MS is indicated by the characteristic detection of intrathecal synthesis of immunoglobulins, which are the main component forming oligoclonal bands (OSBs), detected by immunoelectrophoresis (IEF) of CSF in 95-97% of patients. The presence of OSV in the CSF in patients with clinically isolated syndrome (CIS) significantly increases the likelihood of transition to relapsing-remitting MS, regardless of MRI results. In addition, it has been shown that in patients with MS without TOS in the CSF, the course of the disease is more benign and is often characterized by an atypical clinical picture and MRI findings [30]. At the same time, it is worth noting that OSV can occur in other autoimmune, as well as infectious and oncological diseases of the central nervous system [39]. Interestingly, OSVs appear at the onset of the disease, and subsequently, regardless of the course, activity of the process and treatment, their set does not change [39, 80]. Detection of IgM OSV, especially those directed at lipid antigens, correlates with a more aggressive course of the disease (high proportion of progressive forms, early disability) and a worse response to immunomodulator therapy [8, 10, 45, 70, 72, 79].
Another marker of B cell activation is immunoglobulin kappa light chains (FLC-&kgr;), which are proteins produced by B cells during the production of antibodies.
Subsequently, quite a lot of work was devoted to studying the sensitivity and specificity of this marker for the diagnosis and differential diagnosis of MS. Many studies [22, 31, 56] have shown that the determination of FLC-&kgr; levels, as well as the determination of the monomeric light chain ratio &kgr; to light dimeric chains λ is not inferior in diagnostic significance to OSV in the CSF. It is believed that the composition of FLC is stable during the course of the disease; in addition, it does not change during treatment with immunomodulators [60, 61]. Finally, it is worth noting that one study [61] also showed the prognostic value of FLC-κGr;: patients who had a high concentration of the marker in the CSF were earlier required support when walking.
Changes in the antibody “profile” in MS are detected both in the blood and in the CSF. At the same time, the relationship between the “profiles” of antibodies in the CSF and serum in MS varies. In most patients with a relapsing course, antibody profiles indicate antibody synthesis only within the CNS. In 10% of patients with a relapsing-remitting or secondary progressive form and in almost all patients with a primary progressive form, the TSV part is detected only in the CSF, but there are bands that are found in both the CSF and serum, indicating damage to the BBB [72]. .
The targets of antibodies in MS are unknown. The main proteins, lipids and other candidate compounds are listed in Table. 1
.
However, no study has identified antibodies corresponding to the main band obtained by electrophoresis.
Among the antibodies that make up OSV, there are immunoglobulins of classes G and M. IgM is of particular importance in MS. Intrathecal synthesis of IgM is not a primary immune response, but a persistent one. As a rule, it occurs as a result of activation of one of the subtypes of B cells - CD5+, which synthesize so-called natural antibodies, most often of the IgM class, directed against phylogenetically stable structures [9], primarily lipid antigens. The importance of lipid antigens has been shown in a number of other autoimmune diseases, such as Guillain-Barré syndrome, systemic lupus erythematosus, Sjögren's syndrome, etc. Antibodies to phospholipids, such as cardiolipin, phosphatidylcholine, phosphatidylethanolamine, phosphatidylserine, are more common in patients with MS than in healthy people. and others [7, 26, 63, 68, 71, 78]; cerebrosides and sulfatides [28, 34, 47]; gangliosides, such as GM1 [1, 4, 76, 81], asialo-GM1 [1], GM4 [34], GD1a [1, 47]. However, to date, no “profile” of antibodies to lipids has been identified that is characteristic of one or another form of MS. At the same time, it was noted that antibodies to sulfatides are more common in secondary progressive disease [28], and IgG to GD1a - in primary progressive course [1]. In addition, some lipid antibodies may have prognostic value. Thus, the detection of antibodies to galactocerebroside in patients with CIS is a predictor of its transition to relapsing-remitting MS [50]. The detection of antibodies to cardiolipin was associated with the manifestation of the disease in the form of slowly progressive myelopathy or optic neuropathy [33]. A correlation was found between an increase in antibodies to GM3 and axonal damage and a change in disability towards severity in progressive forms of MS [62]. Finally, an increase in antibody titers to GM1 and phospholipids was associated with disease activity and the appearance of lesions that accumulate contrast on MRI [7, 81].
Because many myelin proteins have been implicated in autoimmune allergic encephalitis (EAE) in animal models [64], it has been suggested that they may be potential biomarkers in MS. Many studies have been conducted to study antibodies to myelin proteins or their individual epitopes. Results have often been inconsistent, but the most promising biochemical markers among myelin proteins have been shown to be MOG (myelin oligodendrocyte protein) and MBP (myelin basic protein), but studies have also been conducted on OSP (oligodendrocyte specific protein), MAG, and others. Antibodies to these components could be detected more often in patients with MS, but did not have a significant prognostic value [3, 12]. Using fairly large samples of patients with CIS, it was demonstrated that the detection of antibodies to MOG and MBP is not associated with a higher incidence of disease progression to MS [37]. Titers of antibodies to MOG and MBP in the serum and CSF of patients with MS were generally higher than in the control group, with higher levels of MOG, some studies showing an association with disease activity or a more severe course (in primary cases). progressive and secondary progressive MS) [15, 21, 35]. Increased IgA titers to MBP and MOG were associated with a progressive course. Since this type of immunoglobulin cannot initiate an inflammatory response, it is believed that their effect is due to the inhibition of remyelination [15].
Due to the assumption that one of the etiological factors in MS are various infectious agents, many studies have been conducted aimed at identifying infectious markers, including antibodies to viral and bacterial antigens, and determining their diagnostic and prognostic value. The largest number of works is devoted to the Epstein-Barr virus (EBV). In MS, a higher proportion of seropositivity to EBV was noted (99% versus 90-95% in the general population); in addition, an association between MS and infectious mononucleosis was shown [57]. Many studies have revealed an increase in the nuclear antigen EBNA-1 and 2 associated with the latent course of infection in the blood serum and CSF of patients with MS, including before the onset of the disease, and a connection with disease activity and poor prognosis has been noted [2, 13, 17]. However, such an association has not been confirmed by other researchers [29]. Therefore, today the diagnostic and prognostic value of determining antibodies to EBNA in MS remains a subject of debate. Data regarding other infectious agents, such as measles, chickenpox, rubella, herpes simplex, cytomegalovirus, HHV-6, chlamydia, mycoplasma, and streptococci viruses, are even more contradictory.
An important link in the pathogenesis of MS is the spread of process activity to surrounding tissues. Astroglia is the most metabolically active component of the nervous system; its changes in inflammatory diseases are undoubtedly more pronounced than in other pathologies of the central nervous system [82].
Glial acidic protein (GFAP) is a large structural protein of the intermediate filaments of astrocytes. An increase in its concentration is associated with high astroglial activity, which most often accompanies the inflammatory process in the central nervous system, accompanied by astrocytosis. It has been shown that during the acute period of the disease, the concentration of GFAP in the CSF increases with extensive damage, such as occurs in neuromyelitis optica, and is an unfavorable prognostic marker [74]. Among patients with MS, an increase in GFAP in the CSF was detected in patients with secondary progressive MS and rarely in relapsing-remitting MS, and positively correlates with the severity of neurological deficit [25, 43, 44, 55].
S100 is an acidic calcium-binding protein, expressed predominantly by astroglia, and is a marker of acute damage to the central nervous system; its increase was detected during the acute period of stroke and traumatic brain injury [20, 52]. Data on changes in the level of this peptide in MS patients during exacerbations are not convincing enough [38, 55].
Finally, one of the most important damaging factors in MS, as in any inflammation, is an increase in the expression of NO synthase mRNA in astrocytes, microglial-macrophage cells, endothelial cells, and, as a rule, such changes are characteristic of active lesions, whereas in In old lesions and lesions in patients with secondary progressive MS, such activity is not observed [41]. The interaction of NO and its metabolic products with proteins leads to the formation of nitrated amino acid residues, S-nitrosothiols (RSNOs), N-nitrosamines (RNNOs), and nitrosohemoglobin.
Most studies show an increase in the level of nitrites in biological fluids compared to the control group: the level of nitrites is higher during exacerbation, depending on the type of MS. Peroxynitrite and reactive oxygen species (ROS) lead to mitochondrial damage, which underlies one of the possible mechanisms of neurodegeneration in MS.
Markers of neurodegeneration.
Until recently, neurodegeneration was considered to be the cause of persistent symptoms in progressive MS. However, thanks to the expansion of biochemical and neuroimaging methods, it has been revealed that neurodegeneration occurs already at the earliest stages of the disease. Pathological studies have found that axonal loss in MS occurs not only in the lesions, but also in the surrounding white matter, and there was no correlation between the extent of the lesions and the degree of axonal damage. In vivo MR spectroscopy revealed a decrease in the amount of N-acetyl aspartate in the white matter unchanged on T2, which confirms axonal destruction. Thus, it can be hypothesized that axonal loss in white matter may occur through two mechanisms. On the one hand, axonal damage can occur as a type of degeneration in foci due to periodic inflammation and demyelination. On the other hand, axonal damage can occur as a diffuse axonopathy that does not correlate with demyelination, which is expressed in a constant increase in neurological deficit, more often with the progressive course of MS. According to histochemical studies, identical changes in axons occur in plaques and in the area of diffusely altered white matter, represented by an increase in the degree of phosphorylation of neurofilaments and a change in their conformation. It is likely that both types of axonopathy may be present to varying degrees in different patients and in different CNS pathways, which may cause significant heterogeneity in the course of the disease.
There are a number of studies aimed at studying changes in the gray matter of the brain in MS using MRI; a significant correlation of the degree of gray matter damage with the EDSS score has been shown already in the early stages of the disease [61]. During clinical observations, it was noted that the cognitive deficit that occurs in patients, as a rule, does not exceed a moderate degree for a long time and does not regress during treatment. Neuroimaging studies of patients with cognitive deficits have shown a significant decrease in the volume of gray matter in the neocortex. Thus, neurodegenerative changes also occur in the cerebral cortex of MS patients.
Neurofilament subunits are highly specific markers of axon destruction. These heteropolymeric proteins are composed of three peptides called light, medium and heavy chains (NfL, NfM and NfH, respectively). Previous studies have obtained scattered information about the content of NfL and NfH in the CSF and blood of MS patients: the concentration of NfL in the CSF is higher in MS patients with relapsing-remitting MS during the exacerbation period compared to the period of remission and patients with primary progressive MS. The maximum concentration of NfL was detected in the 3rd week from the onset of exacerbation. Treatment with natalizumab resulted in a significant reduction in intrathecal NfL levels [25]. Antibodies to NfL are more often found in patients with primary progressive MS [44]. It has also been shown that the level of NfL in the CSF is higher during an exacerbation in patients with a remitting course of the disease than in other variants [44]; a positive correlation of NfL level with cognitive changes in patients with CIS was found, and the presence of antibodies to NfL was shown [19].
Another component of the cytoskeleton are microtubules, consisting of α- and β-tubulin subunits. Associated with microtubules are tau protein and microfilaments, including actin. The levels of tubulin and actin in the CSF are higher in patients with progressive forms of the disease compared to relapsing-remitting MS and correlate with the EDSS score [66]. Thus, actin and tubulin are markers of disease progression. Tau protein acts as a stabilizer of the structure and organization of microtubules; its increase in the CSF has previously been described in Alzheimer's disease. This protein is localized primarily in neurons and glial cells. Conflicting data have been obtained on the association of tau protein with the stage of MS [69]. An increase in tau protein and NfH can be detected already at the onset of the disease; the NfH level is a predictor of the transition of a demyelinating disease to definite MS [11].
The neurodegenerative process is characterized by changes in enzyme activity and, as a consequence, the formation of β-amyloid from the amyloid precursor membrane protein. In MS, the synthesis of amyloid precursor protein in neurons increases, and the mobility of membrane secretase, which is involved in the formation of neurotoxic amyloid 1-42 [27, 40] and β-amyloid 1-40, which is often associated with microangiopathy, increases [23]. Data on the level of β-amyloid peptides in the CSF of MS patients are sparse and conflicting in their results: no difference was found between patients and the control group [67, 77].
Amyloid 1-42 is an extracellular insoluble protein, which explains its decrease in the CSF of patients with Alzheimer's disease. Its decrease was also found in patients with MS; a correlation was shown with cognitive deficits and decreased plasticity induced by transcranial magnetic stimulation [51]. Amyloid peptides may also be new antigens formed as a result of a pathological enzymatic process. The neuroprotective role of β-amyloid 1-40 and 1-42 was demonstrated using the example of experimental autoimmune encephalitis [24].
Protein 14-3-3 is a soluble cytoplasmic protein found in most mammalian tissues that is involved in the regulation of cell cycle processes, apoptosis, and signal transduction. Protein 14-3-3 is a marker of Creutzfeldt-Jakob disease, and its concentration has been shown to increase in patients with Guillain-Barré syndrome. In relapsing-remitting MS, an increase in the 14-3-3 protein in the CSF was detected; according to proteomic research methods (2D electrophoresis and MALDI-MS), the 14-3-3 protein is a marker of the exacerbation phase in MS [69].
The purpose of this study was to investigate neurofilament heavy chains and antisulfatide antibodies in MS.
Material and methods
The study included 3 groups of patients with MS, as well as healthy controls matched by gender and age.
The group studying IgG class immunoglobulins to sulfatide in serum included 51 patients with MS, 15 with secondary progressive MS, 36 with relapsing-remitting MS and 22 sex- and age-matched healthy controls. The characteristics of the groups are presented in Table. 2
.
The degree of disability on the EDSS scale was 3.2 (2; 7) in the group with relapsing-remitting MS and in the group with secondary progressive MS - 6.1 (4.5; 8).
In the group of secondary progressive MS, the average duration of the disease before its onset was 97 (24-220) months. A serum NfH study was conducted in 25 patients with relapsing-remitting MS, 21 with secondary progressive MS, and a comparison group of 13 patients with amyotrophic lateral sclerosis. The control group included 13 patients without pathology of the nervous system who underwent surgery using spinal anesthesia. The characteristics of the patient groups are presented in Table. 3
.
In the relapsing-remitting MS group, the degree of disability on the EDSS scale was 4 [2.5;
4.5], in the group of secondary progressive MS, the duration of the disease was 40.5 months [36; 90], degree of disability on the EDSS scale 6.5 [6.5; 6.5]. Blood sampling was carried out in the morning. Immediately after collection, centrifugation was performed (2000 rpm, 15 min). The resulting sera were stored at -80°C until use.
Determination of antibodies to sulfatide was carried out using ELISA (human sulfatide ELISA kit, Cusabio), according to the manufacturer's instructions. NfH and amyloid 1-42 levels were determined in the serum of patients with secondary progressive MS, the serum and CSF of controls, patients with relapsing-remitting MS, and patients with amyotrophic lateral sclerosis. Determination of NfH was carried out using ELISA (ELISA kit for the Sensitive Detection of the Heavily Phosphorylated, Axonal Variants of the Major Neurofilament subunit NF-H, EnCor Biotechnology Inc.), amyloid 1-42 - using ELISA (ELISA kit for Human Aβ42, Invitrogen). The analysis was performed strictly according to the manufacturers' instructions.
results
In previous studies, the detection of antibodies to galactocerebrosides in patients was a precursor to the transition from CIS to MS; its sulfatides were more often detected in patients with secondary progressive MS [28, 34]. These data may indicate an unfavorable prognostic value when detecting such antibodies in the biological fluids of patients, and therefore antibodies to sulfatide were studied in the serum of patients with MS.
Antibodies to sulfatide were detected in 8 (36%) healthy and 24 (47%) patients with MS. Moreover, they were detected with the same frequency in relapsing-remitting (47%) and secondary progressive (47%) MS, but were not detected in any patient during the first exacerbation of the disease. The detection of antibodies to sulfatide was associated with an earlier onset of the secondary progressive course (40 months in those positive for IgG to sulfatide versus 115 months in those negative).
Taking into account the data on the importance of neurodegeneration at all stages of disease development, the contribution of degenerative processes to the formation of persistent neurological deficits, and the increase in imaging signs of degeneration during a long course of the disease, we conducted a study of the concentration of NfH and amyloid 1-42 in the serum and CSF of patients with relapsing-remitting MS and lateral amyotrophic sclerosis (comparison group), blood serum of patients with secondary progressive MS, serum and CSF of the control group.
When comparing pNFh levels in the CSF, the study groups differed significantly from each other. An increase in the level of neurofilaments was detected in the CSF of patients with relapsing-remitting MS ( p
=0.015) and in patients with amyotrophic lateral sclerosis (
p
=0.005) when compared with the control group, while there were no statistically significant differences between the groups of patients with relapsing-remitting MS and amyotrophic lateral sclerosis. To obtain data comparable to the results of previous studies conducted in this area [19, 25, 44], our results were presented as a percentage of control samples. When comparing serum pNFh levels, no differences were found between the same groups and the secondary progressive MS group.
When studying the level of β-amyloid 1-42 in the CSF of patients with relapsing-remitting MS at the time of exacerbation (14 patients) and the period of remission (5 patients), it was revealed that during the period of exacerbation the amyloid concentration significantly increases by 2 times - 157.5 [97.8; 199.7] and 71.8 [19.7; 86.3] pg/ml, respectively ( p
=0,02).
The data obtained allow us to assume a gradual development of the process of neurodegeneration during the formation of the pathological process characteristic of MS, contrary to the idea of it as a distant process and a consequence of demyelination.
Treatment
Multiple sclerosis
This is a chronic disease, the complete cure of which is impossible. All measures are aimed at slowing the progression of the disease, relieving symptoms and reducing the frequency of exacerbations. There is no single treatment plan; each patient requires an individual approach.
The remitting nature of the disease, characterized by periods of weakening and intensification of symptoms, requires symptomatic treatment, prevention of exacerbations, and inhibition of the transition to the active stage. In the secondary, progressive form, the main goal of therapy is to slow the development of sclerosis. The doctor must understand what stage the patient is in. to correct his condition. To do this, the patient regularly undergoes prescribed tests, undergoes research, most often an MRI and an immunological blood test.
Do not forget that in addition to physiological symptoms, the patient undergoes a psychological personality change. May become depressed, experience chronic fatigue, anxiety and depressive disorders. Multiple sclerosis is associated with a wide range of mental disorders: from personality disorders to altered psychotic states. This also requires attention from a doctor.
Main objectives of treatment:
- Prevent exacerbations.
- Slow down the course of the disease.
- Prevent the development of new symptoms and reduce their severity.
- To alleviate the current symptoms, to help the patient lead his usual lifestyle.
An important role is played by the patient’s social adaptation and timely psychological assistance. Despite the fact that the diagnosis of multiple sclerosis is made by a neurologist, a number of specialists are involved in the treatment: an immunologist, an electrophysiologist, a neuro-ophthalmologist, a neuropsychologist, and a urologist.
Advantages of taking tests at JSC SZTsDM
- All types of laboratory tests, including those for diagnosing MS.
- Data accuracy thanks to modern equipment and qualified employees.
- Quick availability of results, several options for obtaining.
- Friendly staff, confidentiality, no queues.
- Convenient location of terminals.
The laboratories of the Northwestern Center for Evidence-Based Medicine are represented in Pskov, Veliky Novgorod, Kaliningrad, St. Petersburg and other cities of the Leningrad region.
Conclusions:
- Multiple sclerosis is a pathology affecting the nervous system. It is based on damage to the sheaths of nerve fibers and disruption of impulse conduction.
- The disease is not hereditary, but with certain combinations of genes the risk is higher.
- Increased background radiation, intoxication, stress, and previous injuries can provoke the development of the disease.
- When the first symptoms of multiple sclerosis appear, it is important to consult a doctor promptly. It’s better to have it confirmed that it’s just overexertion and fatigue, and not to find yourself in a situation where one on one is the acute phase of the disease.
- With multiple sclerosis, the quality of life deteriorates significantly. First of all, because physical activity decreases. But, if previously multiple sclerosis was immediately a death sentence, now there are methods and drugs through which it is possible not only to relieve the symptoms of the disease, but also to slow down the development of the disease. Doctors have learned to keep the disease under control. With timely diagnosis and treatment, the pathology no longer negatively affects life expectancy.
- CT and laboratory diagnostics play an important role in diagnosis. When clarifying the diagnosis, it is essential where the problem areas are located: in the brain or spinal cord.
In the 5th hospital of the city, treatment of multiple sclerosis is one of the main profiles. The hospital base has expert-class equipment for diagnosing this disease. Consultations with experienced neurologists are available. Treatment is approached in a comprehensive manner. Drug therapy, massage, physical therapy, including cycling on special simulators, and hypobaric oxygenation sessions are organized.