A brain lipoma is a tumor consisting of adipose tissue and is localized in the brain under the frontal cortex. The common name for lipoma is wen. The cavity of the formation is filled with a fatty substance located in the subcutaneous capsule. The size of the wen reaches several millimeters at an early stage of development and five centimeters at a late stage.
This pathology is characterized by painlessness, mobility, slow growth and a latent form of development, due to which the lipoma cannot be detected independently at the initial stage of the disease. Gender, age and body weight are not determining factors in the occurrence of intracranial wen. The ICD-10 code D17 defines a wen as a benign neoplasm. Despite this, the disease can transform into a malignant pathology.
Types of intracranial lipoma
There are a number of types of brain lipoma with characteristic features and different locations in the head.
- Interhemispheric lipoma forms in the callosal tissue of the brain. The most common form of wen is multiple. The tumor interferes with the normal functioning of the cerebellum and provokes disturbances in human behavior and cognitive functions. Wen provokes the occurrence of massive mental disorders, affecting both hemispheres of the brain. Against the background of the disorder, the appearance of hallucinations, memory disorders, and even progressive dementia is observed.
Brain lipoma
- A lipoma of the interhemispheric fissure of the brain is discovered by chance during a full profile examination of the human body, since it is secretive at the initial stage of development. Most people can live with a brain tumor for many years and be unaware of the pathology. Increasing in size, the lipoma interferes with normal blood circulation in the intracranial area, which is fraught with frequent loss of consciousness, dizziness, nausea and headaches. The mutated tissue of the wen adversely affects the central region of the brain, causing visual and auditory hallucinations, behavioral disturbances and motor dysfunction. The fatty tissue puts pressure on the central nervous system, disrupting the circulation of cerebrospinal fluid. The human brain is considered the most dangerous place to localize a wen, as it causes mental disorders and, spreading to the pituitary gland, can lead to paralysis.
- The pericallosal tumor does not affect the corpus callosum and is localized nearby. The pathology is characterized by large size and rapid growth. This type of pathology is recognized as congenital.
- A spinal cord tumor is a neoplasm that is localized in the spine and has the ability to grow deep into the spinal canal. The wen is soft and elastic to the touch. The disease is easily diagnosed by palpation. Most often the disease occurs in newborns. Spinal cord fatty tissues have three types: intradural, filum terminale and lipomyelomeningocele. The pathology of the filum terminale consists of a fatty consistency and is located in the upper region of the intergluteal fold. The main symptom of this disease is the appearance of a skin growth over the buttocks. Skin pathology does not have hair. Wen of the filum terminale is considered a rare phenomenon and occurs in only 5% of the population, mainly in children. Spinal cord adipose tissue occurs as a result of traumatic brain injury, hereditary predisposition, pathological changes in surrounding tissues and diseases of the internal secretion of glands and diabetes mellitus. The pathology can be congenital or acquired. In a child, the first symptoms appear as they grow up in the form of headaches, pelvic dysfunction, pain and compression in the area where the pathology occurs.
Spinal cord lipoma
- Lipoma of the falx cerebri, or Falx's wen, is a capsule filled with fatty fluid, which is located in the area of the frontal lobe of the skull. This type of wen causes frequent headaches, motor dysfunction and involuntary twitching of the limbs. The size of Falx lipoma can reach five centimeters in diameter. The first symptom of the presence of a falx lipoma is behavioral disturbances in a child, which is caused by the localization of the tumor.
- Lipomas of the corpus callosum of the brain spread to the subcortical formations and adjacent parts of the cerebral cortex, which complicates the timely diagnosis of primary symptoms. Location: frontal, temporal and occipital regions of the skull. Located in the frontal lobe, the tumor provokes the occurrence of apathy, lethargy, dysarthria, early pelvic disorders and bilateral motor disorders. Lipoma of the occipital lobe does not have a negative effect on the human mind, but sensory and psychosensory disorders are noticed. The fatty tissue located in the temporal lobe provokes memory impairment and impairs the quality of speech. Any type of lipoma of the corpus callosum is accompanied by the occurrence of mental disorders.
- Intracranial quadrigeminal lipoma is a congenital pathology of low density, located in the occipital region. This phenomenon occurs in adults and children. The pathology is characterized by slow growth. The first symptoms manifest themselves in impaired functioning of the respiratory organs, decreased mobility of the limbs and the occurrence of regular headaches. The localization of this pathology provokes visual impairment.
- A calcified lipoma has a capsule consisting not only of adipose tissue, but also of calcium. Pathology of this type can form necrosis of the corpus callosum.
- Interhemispheric tumor occurs as a result of underdevelopment of the corpus callosum and occurs mainly in children. Lipoma of this type is considered congenital.
Brain lipoma in section
- Fibrolipoma is a congenital pathology of the spinal cord. The disease is characterized by fatty transformation, thickening, shortening and loss of elasticity of the dorsal filament. Most often occurs in children during progressive growth and development - from 4 to 18 years. The greatest growth of the tumor occurs in the first year of a child’s life - the size can reach 24 centimeters in diameter. During a general examination of the skin, 30% of hidden skin abnormalities are detected. Symptoms of fibrolipoma include pain in the lumbar region and thoracic spine, functional disorders of the pelvic organs, the occurrence of meningitis, hair growth in the area where the pathology appears and pain in the lower extremities during physical activity.
Symptoms of lipomas
The clinical picture of the pathology is quite sparse and is characterized by:
- the presence of a palpable formation, which is distinguished by its soft consistency, mobility, and elasticity;
- the appearance of pain due to compression of nerve trunks or growth in internal organs;
- stability of the compact size or its increase with weight loss;
- swelling of the limbs and disruption of their function (if the formation compresses nerves and blood vessels).
If a malignant process develops, general malaise and headaches appear, blood pressure rises and other characteristic symptoms of intoxication of the body appear.
In this case, depending on the exact location of the compaction, other, more pronounced symptoms and signs may occur:
- neoplasms in the esophagus cause nausea and cough;
- seals on the trachea and bronchi cause a painful dry cough that does not subside after taking antitussive drugs;
- a fatty tumor on cartilage and tendons causes pain in the joints and impedes movement;
- formation in the mammary gland provokes pain in this area;
- compaction in the kidney area causes increased blood pressure, colic and lower back pain;
- a formation in the head causes neurological symptoms – headaches, dizziness;
- lipoma of the neck is accompanied by hoarseness, hoarseness, difficulty swallowing;
- a neoplasm in the heart area causes the development of cardiac pathologies: arrhythmia, heart failure, etc.
Agenesis of the corpus callosum
This phenomenon often accompanies various brain defects, including lipomas. Agenesis of the corpus callosum develops in the fetus and is predominantly found in children. The disease manifests itself in the form of delayed physical and mental development of the child, convulsive seizures and paralysis. Isolated agenesis is asymptomatic and is discovered accidentally during a profile examination.
Pathology occurs at the 12th week of fetal development. In medical practice, total agenesis occurs, when the posterior part of the corpus callosum is absent, and partial agenesis, in which the anterior part of the corpus callosum is absent.
Brain pathology negatively affects the functioning of the nervous system and significantly slows down mental development in children: cases of mental retardation, idiocy, and dysfunction of the speech apparatus have been recorded.
What is a brain lipoma?
This is a tumor structure formed by lipocytes (“fat cells” in Latin).
They get out of control and begin to multiply (divide) frequently. As a result, there are more of them than are needed in a particular place. A tumor is emerging. Lipoma is a benign brain tumor; it grows very slowly, does not grow through nearby structures (however, it gradually compresses them), does not metastasize, and does not turn into cancer.
Pericallosal lipoma of the brain on MRI
General symptoms of the disease
Common symptoms of the disease by which wen can be recognized include:
- aching pain in the frontal region of the head;
- involuntary movement of limbs;
- nausea and vomiting;
- dizziness;
- compression in the temporal region of the head;
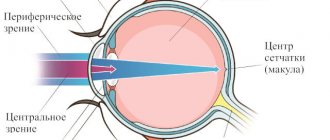
- deterioration of vision and concentration;
- decreased mental abilities;
- a sharp increase and decrease in blood pressure;
- insomnia, lethargy, apathy;
- lack of appetite and constipation.
Treatment methods used
When identifying a brain lipoma, first of all, the presence of symptoms, location, and its size are recorded. If the tumor is benign and does not affect the patient’s quality of life, doctors in this clinical case take a wait-and-see approach. To track dynamics, constant monitoring of possible growth in education will be required.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
Fatty tumors are insensitive to the effects of highly active X-ray radiation and the use of cytostatic agents (chemotherapy).
An increase in lipoma size, which puts pressure on nerve endings and blood vessels, is an absolute indication for surgical treatment.
The choice of surgical intervention method directly depends on the location of the wen and the individual characteristics of the patient.
Endoscopic treatment
During the operation, a small hole is made and drilled into the skull. An endoscope with a video camera is inserted through it to obtain a full overview.
A thorough examination of the formation will allow the formation to be completely removed within healthy tissue.
Conventional surgery
The operation takes place under general anesthesia. The surgeon performs trepanation of the skull followed by extraction of adipose tissue and capsule. This method is justified for large tumor sizes.
The operation is traumatic, but the number of relapses with this treatment is minimal. The stitches are removed after 7 days.
Difficulties during removal arise if the tumor is intertwined with nerves and blood vessels. Any inaccurate movement by the surgeon can lead to serious consequences.
Carrying out aspiration puncture
A special needle with suction is inserted through a small hole in the skull, with the help of which the wen is removed. The disadvantage of this method is the impossibility of removing the capsule and, as a consequence, the risk of relapse.
Before surgery, it is mandatory to conduct an HIV test, a general clinical laboratory examination, and determine the biochemical composition of the blood and glucose level. It is important at the preparation stage to exclude any contraindications for surgery.
Complications during lipoma removal occur rarely and in most cases are associated with subsequent infection of the postoperative wound, as well as the appearance of a hematoma. Treatment with traditional methods is unacceptable in this case.
Only the use of modern techniques will avoid severe damage to parts of the brain. After removal of the lipoma, a histological examination is possible.
Causes
The factors influencing the occurrence of wen have not yet been fully elucidated, but probable causes include:
- heredity;
- bad habits, especially abuse of alcoholic beverages and tobacco products, as they have a direct effect on the brain;
- infectious diseases of the central nervous system increase the risk of tumor development;
- foci of inflammatory processes located in the brain;
- polluted environment;
- unhealthy diet, especially abuse of fatty, sweet and spicy foods;
- physical and chemical effects on the brain;
- presence of mental illness, especially schizophrenia;
- stress, lack of sleep, nervous tension.
Causes of lipomas
Experts identify a set of prerequisites that can provoke the formation of lipomas. Among the most common:
- genetic factors, hereditary predisposition;
- disruption of metabolic processes in the body and fatty tissues;
- insufficient level of personal hygiene;
- malfunctions of the thyroid and pancreas;
- chronic pathologies that significantly affect the body’s immune forces (diabetes, hepatitis, HIV, etc.);
- dependence on alcohol, tobacco, drugs;
- poor nutrition;
- obesity, excess fatty tissue;
- injuries, damage;
- sedentary lifestyle, lack of physical activity.
Despite the fact that lipoma is a benign formation, there is always a risk of developing its malignant form. This probability is especially high for people who are included in the relevant risk groups: they have precancerous diseases (polyps, dysplasia), have already suffered from oncological pathologies, have a hereditary predisposition to the formation of tumors, and are under the constant influence of carcinogens, radiation and other harmful environmental factors.
Diagnostics
Wen in the brain at an early stage of development is difficult to detect due to the lack of symptoms. Cases have been recorded where people lived with a tumor for decades and were not aware of the existence of the phenomenon. The pathology is discovered accidentally during a profile examination of the patient. You should not wait for the first symptoms of a tumor, because modern methods for diagnosing such pathologies are known.
CT scan
CT is an informative and safe examination of the intracranial area. The method allows you to make an accurate diagnosis and replaces ultrasound or radiography, or saves time and makes it possible to find out the results immediately. Using computed tomography, the tumor is visualized in detail, down to the vessels and nerve endings.
Neurosonography
Ultrasound examination of the brain, or neurosonography, is actively used in pediatrics and helps to obtain information about the location, size and degree of tumor growth within the cranial space. Already in the first month of life, a newborn should be examined for the presence of congenital tumors. With the help of neurosonography, even a small tumor at an early stage of development can be detected. It is advisable to undergo examination for children born with low body weight, birth injuries, developmental pathologies and intrauterine infection.
MRI
Magnetic resonance imaging, or MRI, provides accurate information about the extent of tumor development. Diagnosis using this method is much more effective than CT or ultrasound, since MRI makes it possible to obtain a three-dimensional image of a lipoma, which is a more detailed image. The wen has a sharply defined shape in the resulting images. The main sign of lipoma detection is the high signal intensity of adipose tissue when pathology is detected.
Types of lipomas
There are several main classifications of lipomas that are actively used in medical practice. Depending on the type of tissue that is involved in the pathological process, the following types of neoplasms are distinguished:
- perineural - localized around nerve trunks;
- intermuscular – located between the muscles of the body;
- lumbosacral - grow near the vertebrae or in the spinal canal;
- soft tissues - located on the surface of the skin, less often subcutaneous;
- joints - are located in the synovial membrane or vagina of the joints.
The formation can appear in almost any part of the body and internal organs. Depending on the location of the compaction , the following types of lipomas are most often diagnosed:
- mammary gland - forms in the glandular tissue and deforms the shape of the breast as it grows;
- breasts - a soft and mobile formation that appears in the subcutaneous fatty tissues;
- head - a frequently occurring pathology, which is mainly formed as a result of insufficient hygiene;
- back - one of the most common neoplasms, characterized by extremely slow development;
- neck is a hereditary disease that, during development, can impair the airways, cause weakness and angina.
There are also other, less common places where pathology forms, which include the brain, limbs, skin, peritoneum, eyes, lips and face.
Also, these compactions are divided into two large groups: single and multiple. The first represent a single formation in any part of the body. The latter, accordingly, are characterized by multiple manifestations in different areas of the body and are much less common.
Treatment
Most often, patients seek medical help when the lipoma needs to be removed. This is due to the absence of symptoms at an early stage or medical wait-and-see tactics. Doctors do not recommend treating at the initial stage of development, so as not to provoke changes or growth of pathology, and observe the patient for a long time until the first symptoms appear. Increasing in size, the wen brings discomfort and pain, and then the question arises of removing the tumor.
Surgical intervention
The fatty tissue poses a threat to the life and mental health of a person, increasing to a substantial size, so surgeons carry out radical removal along with the capsule to avoid further relapses. During the operation, craniotomy is performed, that is, part of the skull is removed.
Brain surgery
Minimally invasive intervention
This method includes endoscopic tumor neutralization, which is carried out using an endoscope and a video camera. The doctor removes the fat along with the capsule using this method. Minimally invasive intervention also includes the puncture-aspiration method of removal.
During the procedure, a hole is made in the patient's skull through which the operation takes place. A tube is inserted into the hole and the pathological fatty tissue is removed using an electric suction. The only drawback of the operation is that the wen capsule remains in the human brain and this causes the recurrence of lipomatosis.
Drug therapy
Proponents of the medicinal method are confident that the brain wen can be removed without surgery. To do this, the doctor prescribes medications that help reduce the size of the lipoma. Most often, hormonal treatment is used, since hormone imbalance is one of the reasons for the appearance of wen, according to theoretical assumptions. Therapy gives results at the initial stage of development, but at the same time it turns out to be ineffective when the wen grows rapidly. To eliminate the wen, non-traditional methods are actively used: people are sure that herbal decoctions and compresses cause complete resorption of the tumor, but often folk remedies are ineffective. Treatment should be carried out comprehensively and only as prescribed by a doctor.
Differential diagnosis
Since lipoma does not produce symptoms for a long time, it is often diagnosed accidentally, during preventive and periodic examinations or during research for other pathologies.
If the clinical picture has already formed, then pay attention to the following complaints of the subject: nausea, increasing pain, insomnia. During a neurological examination, the doctor assesses the state of the patient’s reflexes, skin and deep sensitivity, muscle strength, checks whether there are disorders of the sphere of consciousness, and inquires about the facts of epileptic seizures.
Instrumental studies remain the main ones in identifying a tumor.
X-ray examination
On an x-ray, this tumor appears as a cleared area with a smooth contour.
But the internal structure of the formation cannot be determined from an x-ray. Therefore, they turn to neuroimaging methods.
Neuroimaging
The following methods are used:
- Ultrasound . The location, size, and structure of the lipoma are visualized. The tumor is visible as a hypoechoic (lighter compared to the surrounding tissues) formation of a regular shape, without swelling around.
- CT differentiates lipoma from other neoplasms. In the photographs, the tumor appears as a non-enhancing homogeneous structure with reduced density (down to –100 units N).
- MRI accurately identifies tumors because the resonance from lipomas is the same as from fat. On T1 and T2 images, the tumor gives a pronounced signal; complete disappearance of resonance occurs on fat-suppressed MRI.
Lipomas are differentiated from the following intracranial formations:
- intracranial dermoid (when ruptured, it is observed in the form of multiple inclusions in the subarachnoid space, located in the midline);
- teratoma;
- fatty degeneration of other tumors: gliomas, ependymomas;
- a saccular aneurysm filled with clots.
Based on the theory that lipoma in brain tissue is most often the result of dysembryogenesis, the presence of multiple developmental anomalies must be assumed. If a doctor observes skin stigmas, developmental anomalies of the intestinal tube, pelvic organs, and musculoskeletal system, then he may suspect a diagnosis of brain lipoma.
Diagnosis of lipomas
A lipoma under the skin is easily diagnosed by inspection and palpation.
Lipomas inside the body are detected using:
- Ultrasound
- MRI
- radiography.
In unclear cases, a biopsy is performed, in which a small amount of tissue is examined under a microscope.
Which doctor should I contact?
Since lipoma can grow anywhere in the body, it is diagnosed and treated by doctors of various specialties. This depends on the location of the formation. Lipomas on the skin are dealt with by a surgeon and a dermatologist, lipomas in the breast area by a mammologist, lipomas of the brain or spine by a neurosurgeon.
What is the difference between atheroma and lipoma?
Lipoma is a formation of adipose tissue, while atheroma is an accumulation of sebaceous gland secretion due to blockage of its duct. Accordingly, atheroma cannot occur where there are no sebaceous glands, i.e. in the lungs, brain, abdominal cavity, spermatic cord, etc. Atheroma often grows on the scalp, tends to become inflamed and suppurative, and is located more superficially. When atheroma becomes inflamed, it increases in size and redness occurs, which does not happen with lipoma. In order to find out whether the patient has an atheroma or a lipoma, an ultrasound is performed.
Types of extracerebral formations of the brain
A feature of extracerebral formations is their long course without obvious clinical manifestations. Patients are unaware of the development of the disease for a long time and do not seek medical help, until the pathological focus increases significantly. Often it is an accidental discovery during a planned preventive examination.
Meningiomas are characterized by relatively slow growth and limited location. The pathological focus develops from the arachnoendothelial cells of the meninges. Statistics show that the disease occurs mainly in women over 30 years of age. Such extracerebral formations of the brain can reach significant sizes.
Most often they are localized in the area of the cranial fossa. In this case, the patient’s sense of smell deteriorates, various mental disorders and decreased vision are possible. With an extracerebral space-occupying lesion in the parietal region, compression of the optic nerves is possible.
Localization of tumors
When an extracerebral formation is localized in the frontal region, clinical manifestations do not appear immediately. The disease threatens the patient's life and causes a gradual increase in tumor size. If the meningioma is located on the left, then clinical manifestations will be expressed predominantly on the opposite side. Patients will experience headaches, decreased muscle tone, blurred vision, and motor seizures.
Extracerebral space-occupying formations located on the right usually cause certain symptoms that are localized on the opposite side - on the left.
We wrote above that meningiomas and other similar extracerebral formations are more common in women. Hormonal changes can provoke the development of the disease. It has been observed that such diseases actively develop during pregnancy. Meningiomas often appear against the background of malignant degeneration of the mammary glands in women (metastases to the brain).
Also among the provoking factors, traumatic brain injuries come first. The disease can develop either almost immediately after brain damage or over the next few years. The risk group includes people who have suffered radiation exposure and periodically come into contact with various toxic substances.
Neuroma
The exact location of the tumor can only be determined through comprehensive diagnostics:
- Magnetic resonance imaging. The main method for studying brain formations. Most often complemented by contrast. The method allows you to detect even a small tumor and assess the degree of damage to blood vessels and surrounding tissues.
- CT scan. Suitable for identifying meningiomas of different locations.
- Angiography. The method allows you to assess the blood flow in the tumor, determine further treatment tactics, and conduct high-quality preoperative preparation of the patient.
Extracerebral formations of the middle and posterior cranial fossa, including meningioma of this localization, can reach large sizes. In this case, the patient experiences severe mental disorders, including decreased criticism.
The extracerebral formation of the falx is located in the area of the falx process. The disease manifests itself as epileptic seizures and convulsions. In a complicated course, paralysis of the legs, dysfunction of the pelvic organs, and other dangerous complications occur.
Treatment methods
Brain tumors are treated primarily surgically. It is recommended to contact a neurosurgeon when the first symptoms appear. A persistent headache combined with visual disturbances and a tendency to seizures may indicate the presence of the disease. As the disease progresses, intracranial pressure increases. This leads to nausea and vomiting.
Treatment is prescribed by a neurosurgeon taking into account the results of diagnosis and examination. Severe neurological symptoms with active growth of the tumor are an indication for surgical intervention. The operation can be performed to remove the pathological focus partially or completely. The chosen tactic depends on the proximity of the vital centers of the brain to the tumor.
After surgical removal of the tumor, a rehabilitation period is carried out. It necessarily includes a set of measures that are aimed at restoring impaired functions of the brain and the entire body. Patients may undergo therapeutic exercises, massage, physiotherapeutic procedures, taking neuroprotectors and other drugs with a similar effect.