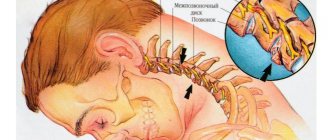
Trigeminal neuralgia (trigeminal neuralgia) is a disease during which attacks of pain (intense, shooting, burning) occur in areas of innervation - areas supplying nerve fibers to the temporal, frontal regions, facial skin, masticatory muscles, ocular conjunctiva, and some muscles of the oral cavity ( for example, mylohyoid).
General information
Pain in the facial area is considered the most difficult in medicine, as it is associated with pathologies of the nervous system, ENT organs, dental system or eyes. However, trigeminal neuralgia is often the cause of such pain.
The problem is at the top of the ranking of neurological diseases due to a large number of factors: excruciating paroxysmal pain, social and work maladjustment (it is extremely difficult for a person to work productively, he is under constant stress), long-term treatment. Symptoms can be identified, but only a specialist can prescribe the exact cause of the disease and truly effective treatment. In the 5th city hospital of Minsk, all conditions have been created for high-quality neurological and neurosurgical care: from diagnosis to treatment.
Symptoms
Most often, the first attacks of pain begin in the jaw area. Pain may appear spontaneously or be provoked by external factors (laughter, chewing movements, articulation). The pain has a shooting character, similar to an electric shock.
To determine the diagnosis, the doctor first of all pays attention to the symptoms that appear, which often appear during sleep:
- one side of the face periodically twitches;
- pain that begins in the jaw area spreads to the cheek, nose, ear, frontal area, eye, throat and tonsils;
- the appearance of red spots on the face (usually on the right);
- copious nasal discharge;
- eyes often water.
Due to pain in the jaw, a person uses only the healthy side to chew food. A lump may form in the muscle on the affected side.
To make an accurate diagnosis and exclude other possible diseases, it is necessary to examine the ENT organs and the oral cavity. An MRI and CT scan should be performed to rule out cluster headache, atypical neuralgia, myofacial pain, jaw pain, and temporal pain.
Pathogenesis
Trigeminal neuralgia develops due to disorders of the central component (blood circulation in the nucleus) or peripheral (peripheral parts of the nerve). For this reason, different approaches are used for treatment.
The pathogenetic mechanisms include vascular, endocrine-metabolic and immunological factors. Because of them, the sensitivity of the nuclei changes and a focus of pathological activity is detected in the central nervous system. After this, trigger (hypersensitive) areas arise in the innervation zones of different branches of the nerve, and when irritated, attacks of pain occur on the face.
The vascular factor is involved in classical neuralgia, when the nerve root is affected by a vertically crossing arterial loop.
Vasculoneural conflict (conflict between a nerve and a vessel) is especially taken into account in people who begin to harden the arteries and nerve fibers. With treginal neuralgia in the elderly, this is the most common case.
Autoimmune processes (in which the body attacks its own cells) cause inflammatory reactions during dental treatment and colds. In this case, it is they that cause trigeminal neuralgia and pain.
Neurostimulation for migraine
Among the non-drug treatments for migraine, transcranial electrical stimulation of the first branch of the trigeminal nerve is used. This treatment method is quite new and there are not enough observations yet. The procedure can only be used on the recommendation of a doctor.
Electrical stimulation is also possible in combination with medications that are used to treat migraines.
Who can use it?
This type of migraine therapy is acceptable for patients whose attacks are infrequent, pass without complications, and do not tend to progress.
Neurostimulation is not contraindicated in patients with a pacemaker, children over 8 years of age, pregnant and lactating women. The main contraindications are epilepsy and recent traumatic brain injury.
How is neurostimulation performed?
Neurostimulation is carried out using small self-adhesive electrodes placed on the skin of the forehead above the eye sockets, where the first branch of the trigeminal nerve passes. The patient can use the transcutaneous electrical stimulator independently.
The device has 3 programs with different stimulation parameters:
- to stop an attack,
- for preventive treatment,
- with a sedative effect.
The benefits of neurostimulation for migraines
The use of electrical stimulators to relieve headache attacks can significantly reduce the use of painkillers.
It is important to note that the use of this type of treatment is possible not only in the form of monotherapy, it is combined both with drugs for the relief of migraine attacks (non-steroidal anti-inflammatory drugs and triptans), and with any type of preventive drug therapy (β-blockers, anticonvulsants, sartans, antidepressants ). This opens up new possibilities for combination therapy, which is especially necessary in complex cases of migraine treatment.
Primary and secondary neuralgia.
The most popular classification is related to etiology (nature of occurrence).
- Primary idiopathic . Arises as a response to vascular compression (squeezing) of the trigeminal root. Most often in practice, such compression occurs in the area of the brain stem.
- Secondary symptomatic . Consequences of infections, the occurrence of tumors and their growth, bone changes.
In order to recognize the nature of trigeminal neuralgia, tomography (neuroimaging) data of the skull and the nerve itself are used.
With true neuralgia, treatment, first of all, needs to focus on the nature of the disease, and with secondary neuralgia, there is a fight against the symptoms and elimination of the underlying disease.
Secondary neuralgia can have a central and peripheral form of manifestation. In the central form, pain appears in the area of one or more branches of the ternary nerve. In the peripheral form, the zone of entry of the nerve root into the medullary pons is involved; in most cases, the loop of the cerebellar artery has pathological changes.
Nature of pain and affected area
Another classification is based on the nature of the pain.
- Type 1 TN . Neuralgia of this type is characterized by a typically pronounced burning sensation. In this case, the pain is acute, but unstable, episodic. The duration of the episodes may vary.
- Type 2 TN . Constant and dull, aching pain.
Type 1 TN ternary neuralgia is more common, while type 2 TN is more rare. At the same time, the disease with this type of manifestation of the disease is most difficult to diagnose, since the picture of the disease is similar to a number of other neurological diseases, and sometimes dental problems, in particular problems with the temporomandibular joint.
The affected area and its scale may also be different, and neighboring zones may be involved. In this regard, the following levels of damage are distinguished:
- Damage to one of the peripheral branches of the trigeminal nerve . When the 1st branch is affected, the sensitivity of the skin is impaired (especially in the forehead and anterior scalp, eyelids, dorsum of the nose, mucous membranes of the upper part of the nasal cavity, a number of reflexes are impaired, for example, the superciliary one). When the 2nd branch is affected, the sensitivity of the skin on the cheekbones and cheeks is lost, the sensitivity of the skin near the outer corners of the eyes is lost, and there are problems with the sensitivity of the skin in the area of the upper jaw, lips, and nose. When the 3rd branch is affected, the lower part of the face (chin, lower lip), tongue, and sometimes there is a problem with the masticatory muscles (up to paralysis).
- Damage to the trigeminal nerve root at the level of the base of the brain . Most often, it is a lesion of the semilunar ganglion, located on the large root of the trigeminal nerve. Most often it is affected by viral diseases. Advanced neuralgia of the semilunar ganglion is fraught with the rapid development of conjunctivitis and keratitis. As a result, you need not only the help of a neurologist, but also an ophthalmologist
- Lesion in the area of the brainstem nuclei . The most painful symptoms are similar to “electric shocks”. Sensation may be lost in areas associated with any branch of the trigeminal nerve.
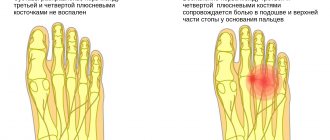
- Dental plexalgia . As the name implies, the localization is associated with the zone of innervation of the dental plexus. The pain is very excruciating. It feels like absolutely everything hurts: the palate, cheekbones, temples, ears, neck (especially the upper third), and the back of the head. The pain especially intensifies when pressing on the problem area.
- Damage to the pterygopalatine ganglion . The processes of the maxillary nerve and a number of fibers in the area of the carotid artery, nasal mucosa, and salivary glands are involved.
- Damage to the area near the orbit . Persistent unilateral headache in the area of innervation of the trigeminal nerve is combined with lacrimation, difficulty breathing, and redness of the face.
Surgical treatment of trigeminal neuralgia - surgery
When the possibilities of conservative therapy have been exhausted, and the patient continues to suffer from attacks of severe pain, surgical treatment of trigeminal neuralgia is recommended. This still occurs in about 30% of patients. Therefore, for them, surgery is the only way a person can get rid of severe pain.
There are several methods of surgical treatment of neuralgia. All of them are aimed at eliminating the irritating effect on the nerve, provided that its source is known, or destroying the nerve.
The methods differ not only in the degree of effectiveness and safety, but also in price. For each patient, the surgeon individually selects the most appropriate method of performing the operation, based on the level and degree of damage to the trigeminal nerve, the clinical picture and existing concomitant diseases.
Today in the arsenal of neurosurgeons there are:
- microvascular or microvascular decompression;
- radiofrequency ablation;
- rhizotomy with glycerol;
- microcompression with a balloon;
- stereotactic radiosurgery.
In the absence of age-related and somatic contraindications, when diagnosing a neurovascular conflict, preference is usually given to microvascular decompression, since it is one of the reconstructive operations and does not lead to loss of sensitivity in one or another area of the face. But when concomitant diseases are detected in a patient, minimally invasive techniques are usually chosen, in particular radiofrequency ablation. It is also indicated for most elderly patients.
But when preparing for surgery, patients should understand that surgical intervention on the nerves requires the highest possible qualifications from a neurosurgeon. The slightest careless movement in such situations can lead to irreversible consequences, including complete loss of facial sensitivity. Therefore, it is important to approach the choice of a clinic and specialist extremely responsibly.
By contacting the SL Clinic, you minimize the risks of the operation, since we employ some of the best neurosurgeons who have considerable practical experience and are scrupulous about the problem of each patient. The clinic has modern equipment, which further increases the chances of success of the operation and reduces the likelihood of postoperative complications. Don’t waste time searching for a suitable medical center, entrust your health to the professionals at SL Clinic and you are guaranteed to receive top-level medical services. The cost of treatment for each method is given in the clinic’s price list.
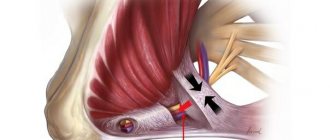
Microvascular decompression
The Jannette procedure, or microvascular decompression, is often used for facial neuralgia. Its main advantage is the preservation of the nerve, while all other operations are destructive. Therefore, after microvascular decompression there is no risk of numbness of part of the face.
But it can only be used in situations where the trigeminal nerve is compressed by a nearby passing blood vessel, from which pulsation is transmitted to the nerve fiber, which provokes pain.
Microvascular decompression is performed openly through an incision behind the ear. The surgeon enters the cranial cavity after trephination of the posterior cranial fossa and revises the position of the trigeminal nerve root, the superior and inferior anterior cerebellar arteries, as well as the superior petrosal vein. After identifying the compression site, he separates the pathologically dilated vessels and introduces a special Teflon separating gasket. It will protect the nerve from mechanical irritation by the pulsating vessel, which will ensure pain relief.
In the vast majority of cases, the method leads to final recovery. Relapses are extremely rare. But microvascular decompression is an open surgical procedure and is associated with high morbidity and intraoperative risks. Therefore, performing the operation requires highly qualified surgeons.
After microvascular destruction, patients must remain in the hospital for up to 10 days. During this time and afterwards, they may experience pain caused by post-operative muscle spasms. To relieve them, taking antispasmodics or NSAIDs is usually sufficient. As the body recovers, the intensity of the pain decreases and soon disappears completely.
Rehabilitation involves taking a number of medications, undergoing a course of physiotherapeutic treatment, and subsequently massage sessions. Such a set of measures will contribute to a speedy recovery and consolidation of the results achieved through surgery.
Radiofrequency ablation
The method is one of the percutaneous operations and is considered the most effective and safe in the treatment of a large number of different diseases, including trigeminal neuralgia.
With the help of an image intensifier, the surgeon is able to precisely control his every movement and the time of exposure to radio waves. Other advantages of the method include:
- no risks associated with general anesthesia;
- extremely short and easy rehabilitation;
- possibility of early activation of patients.
Radiofrequency ablation does not require large incisions and significant tissue trauma. The destruction of the pain-provoking branch, its peripheral node or root is carried out through thermal energy released when ultra-high frequency currents pass through biological tissues.
It is carried out using special equipment consisting of a generator and two electrodes: damaging and indifferent. Ablation of the nerve fiber is performed around the bare end of the damaging electrode. It is introduced into the patient’s body to the selected point of destruction using a hollow guide needle. The length of such a cannula is 100 mm. It is installed under the control of the image intensifier to avoid accidental injury to healthy nerves.
A current with a frequency of 100 Hz is used to destroy sensory fibers, and 2 Hz for motor fibers. Radiofrequency ablation is performed under local anesthesia, so the patient remains conscious throughout the operation. He may feel a slight tingling sensation as the needle gets closer to the affected nerve. To accurately determine the desired branch of the nerve, it is stimulated with current.
After identifying the damaged branch, the electrode heating mode is turned on. It can heat up to 70°C, then the exposure time is only one and a half minutes. But it is preferable to use the pulsed ablation mode, which involves heating the tip of the active electrode only to 42°C. This completely eliminates the possibility of burns to surrounding tissues, but complete ablation requires 2 minutes.
In general, the entire procedure takes no more than 40 minutes. In 90% of cases, it leads to complete recovery, and the pain syndrome either disappears immediately after its completion, or a gradual increase in effect is observed over 6–8 weeks.
After radiofrequency ablation, the patient does not require complex rehabilitation or long-term bed rest. He can leave the clinic the same day.
Percutaneous selective rhizotomy with alcohol
The method involves performing an injection of the drug under MRI or CT control. A thin needle is inserted into the area of the affected nerve root, after which the solution is injected in small portions. The destruction of part of the nerve fiber occurs 3–4 hours after the injection, as a result of which the possibility of conducting a pain impulse is eliminated.
The technique is very old and was used before when there were no other more modern methods of treating neuralgia. This does not exclude the possibility of a relapse, but is not associated with a high risk of loss of sensitivity in the area of innervation of the affected branch of the trigeminal nerve.
Microcompression with a balloon
The operation involves the insertion of a special needle equipped with a small empty balloon. It is brought directly to the affected trigeminal nerve root and inflated until a persistent compression effect is obtained. Pressure has a destructive effect on the nerve fiber and leads to the elimination of pain.
Stereotactic radiosurgery
For more than 50 years, the treatment of neuralgic disorders has been carried out using the so-called Gamma Knife or CyberKnife. This completely bloodless technique does not require any incisions. The effect is carried out through precisely directed ionizing radiation to the affected area of the trigeminal nerve. Guidance is carried out using anatomical landmarks and a computer.
The rays formed by several hundred sources penetrate tissue without damaging them and are precisely focused at the point of impact, creating the required concentration of radiation. The operation, including preparation, takes one day and the patient can leave the clinic immediately after it. When performed correctly, there is absolutely no risk of side effects and complications.
Gamma Knife affects the nerve root located at the point where the brainstem exits the brain. The operation leads to a lasting recovery in 80–90% of cases. Only 7% of patients experience a temporary decrease in facial sensitivity after it.
The method is used to help all patients in whom conservative therapy has failed or was accompanied by severe side effects. In addition, it can be used to treat patients who have previously undergone microvascular decompression and other surgical interventions without obtaining positive changes. But the cost of stereotactic radiosurgery is significantly higher than other methods of surgical treatment of the disease
Causes of inflammation of the trigeminal nerve
Damage to the trigeminal nerve can be caused by both trauma (fractures, tissue ruptures, unprofessional conduction anesthesia) and destruction of the myelin sheath of the nerve itself (a typical problem for patients with multiple sclerosis).
But more often we are talking about the inflammatory nature of the pathology.
The most common causes leading to inflammation of the trigeminal nerve:
- inflammation of the membranes of the brain or spinal cord (meningitis),
- diseases of the paranasal sinuses (sinusitis),
- malocclusion,
- herpes transmitted to the ganglia (nodes) of the trigeminal nerve,
- hypothermia: everyone knows the phrase: “I got a cold on my nerve.” In fact, a person’s tissues become overcooled, and then the nerve becomes inflamed.
- bacterial infection of the upper respiratory tract, throat.
Symptoms of the disease
The most striking symptom of inflammation of the trigeminal nerve is unbearable pain, which is felt in a certain area of the head, on the face. The sensations are shooting and burning in nature, and with minimal movements or touches they intensify and pass through the muscle fibers.
Regardless of the causes of neuritis, the gender of the patient and the pairing of the organ, pain in the vast majority of cases is felt on the right.
Inflammation may also be indicated by:
- increased frequency of sharp attacks of pain up to once every fifteen minutes;
- metallic taste in the mouth;
- discomfort when pressing on the gums;
- twitching of muscles responsible for facial expressions;
- a feeling of hyperthermia at the suspected site of the inflammatory process.
If you do not start therapy, the pain will become stronger and attacks will occur more often. As a result, the fibers will die, and the affected areas will lose sensitivity and paralysis will occur.
It is important to consult a neurologist to eliminate the cause of the pathology, because taking painkillers and NSAIDs only relieves symptoms, but does not affect the disease itself.
The disease usually worsens during the cold season. Sharp pain occurs mainly during the daytime, when the facial muscles are actively used.
Symptoms of inflammation of the trigeminal nerve
The following symptoms indicate nerve inflammation:
- Facial pain.
- Headache, more often migraine.
- Burning sensation, as if “being hit with an electric current” in the area of the cheeks, cheekbones, jaw, forehead, eyes. The pain intensifies when moving the facial muscles, chewing, noise, bright light, or touching the skin.
- Problems with the blink reflex (decreased amplitude) and, accordingly, increased eye vulnerability.
- Involuntary twitching of facial muscles (nervous tic).
- Irritability.
Causes
In many cases, the cause of the disease remains unknown, but more often, after conducting a full medical examination, the doctor can determine the etiology of the disease. The main precursors of nerve inflammation are:
- damage to part of the face by a herpes viral infection;
- trauma that damages the trigeminal nerve;
- atherosclerosis, impaired blood circulation in the vessels of the brain;
- abnormal placement of blood vessels, leading to compression of the nerve;
- aneurysm;
- multiple sclerosis;
- formations in the brain (tumor (meningioma), scars);
Diagnostics
Based only on a survey, a doctor can distinguish tertiary neuralgia from Sjostad syndrome (with this syndrome, longer attacks), post-herpical pain, and typical migraines. To understand the full picture, it is important to carry out a comprehensive diagnosis:
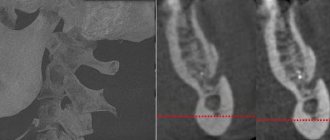
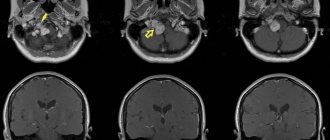
- Tomography. For accurate diagnosis and correct treatment, the most complete data on the state of the brain and the selection of a detailed scheme (the scheme is important for accurate positioning) when performing magnetic resonance imaging of the ternary nerve are extremely important. The most accurate data can be obtained from MRI with contrast.
- Tomography (scanning) scan of the trigeminal nerve. Makes it possible to create layer-by-layer images, identify neurovascular conflict, signs of destruction of the myelin sheath of nerves. The scan allows the doctor to get a complete picture of what the nerve being examined looks like and what is happening where it exits the brain stem.
- It is extremely important that tomography allows not only to identify that there is a neurovascular conflict, but also to understand its cause. This may be a conflict of the cerebellar arteries, a neuroma (neoplasm) of the nerve. In many cases, the trigeminal nerve scan is performed with a simultaneous scan of the facial nerve.
- X-ray of the jaws (if you suspect that the main problem is dental).
- Angiography. Important for verification (confirmation) of the vascular origin of compression with an impressive size of the aneurysm and vascular loop or aneurysm.
Also, in most cases, blood and urine tests are prescribed (the role of these studies is especially valuable in pathologies that arise as a result of infectious diseases).
Diagnostic methods
In order to accurately determine the cause of neuralgia, the neurologist prescribes a number of instrumental examination methods to the patient:
- MRI is a safe research method that allows 100% accurate determination of pathologies of the brain, blood vessels, sclerosis, osteochondrosis;
- CT scan – makes it possible to diagnose diseases of the central nervous system;
- electroneurography or electroneuromyography - helps to determine the speed of impulse movement along the nerve fibers and determine the level of damage to the trigeminal nerve, as well as the mechanism of neuralgia (during electroneuromyography, the sensitivity threshold of muscle fibers is additionally determined, as well as the degree of their contraction).
Laboratory diagnostics are usually not performed, since in the absence of concomitant diseases, blood and urine values are normal.
Treatment
Treatment is aimed at relieving pain and preventing relapses of the disease.
For milder cases of the disease, drug treatment can help; for advanced stages and large affected areas, surgical treatment is used. It also helps to overcome the nature of the disease itself.
Physiotherapeutic techniques are also used in treatment. But most doctors are inclined: they are effective not as primary ones, but only as auxiliary ones: enhancing the effect of conservative drug treatment, and can also be used after surgery at the rehabilitation stage. For example, drug treatment in the acute stage can be effectively combined with light therapy, especially infrared ray therapy in a small dosage. In the acute period and at the time of rehabilitation, phonophoresis, electrophoresis, and darsonvalization provide the desired effect. In the non-acute phase, it is useful to take medicinal baths (for example, with minerals), massages, acupuncture, and paraffin therapy.
Drug treatment
For conservative therapy, the following medications are prescribed:
- Drugs to combat symptoms (pain) . The most common drugs used in drug treatment are carbamazepine, finlepsin, and tegretol. The drug of first choice in most clinics is carbamazepine. It is effective in relieving pain in 70-80% of patients with trigeminal neuralgia.
- Antispasmodics and muscle relaxants of central action . One of the common medications in this situation is baclofen.
- Alcohol blockades (injections) aimed at “freezing” the affected area of the face. The blockades have an effect, but it is short-lived. Therefore, such injections are often resorted to as a temporary measure, for example, in preparation for surgery.
- Metabolic drugs . Their role is important for stabilizing the energy potential of cells and creating an antihypoxic effect.
- Anticonvulsants . Helps slow down the transmission of nerve impulses.
- B vitamins . They have a neurotropic effect (they improve the metabolism of mediators and certain analgesic activity, therefore enhancing the effect of painkillers).
Surgery
Surgical operations are the most effective for combating trigeminal neuralgia. They make it possible not only to eliminate pain, but also to eliminate the chain of impulses and influence the conflict between the root of the cranial nerve emerging from the brain stem and the vessel that adjoins it.
And, if the cause is just such a conflict, doctors recommend immediately thinking about surgery, and not stalling for time and trying to solve the problem with medication.
In this case, microvascular decompression of the trigeminal nerve root is considered the most effective and safe (the nerve is preserved). The operation involves installing a gasket (protector) between the nerve and the vessel.
Microvascular decompression of the trigeminal nerve root is a transcranial endoscopic intervention and is performed through a mini-access (in fact, we are talking about a cosmetic incision - no more than 2.5x2 cm, minimal blood loss, no long-term rehabilitation required)
Mechanical destruction of peripheral branches, glycerin rhizotomy, laser thermocoagulation, and radiofrequency destruction can also be used. They allow you to cope with the victory over pain with dignity, but unlike microvascular decompression, alas, such operations do not have the task of preserving the nerve. Therefore, such operations are used more often in cases where microvascular decompression of the trigeminal nerve root is impossible for some reason. For example, glycerin rhizotomy is often the only possible way to combat neuralgia in patients in severe physical condition at an advanced age with a list of other diseases.
Modern surgical techniques, akin to mechanical destruction, make it possible to eliminate additional destructive interventions and at the same time stimulate the necessary deep structures.
Among the complications of surgical intervention using glycerol rhizotomy, radiofrequency destruction, there are sensory disturbances on the face, keratopathy (the occurrence of corneal dystrophy).
Possible complications after microvascular decompression may be ischemic infarction of the brain stem, air embolism, damage to the trochlear nerve, the occurrence of cerebellar hematoma, paresis (reduction) of the facial muscles.
For this reason, it is extremely important to clearly weigh the degree of risk for the patient and choose the right surgical technique. Whether one or the other is suitable in each specific case depends on the individual characteristics of each patient. Careful attention to these details helps minimize the risks of complications.
Where the operation is performed is also important. All the nuances are important: how accurate the preliminary diagnosis is, the qualifications and experience of the neurosurgeon.
Treatment of trigeminal neuralgia
Initially, treatment always begins with conservative therapy. Only if it is completely ineffective, patients are offered surgery.
Conservative treatment of trigeminal neuralgia includes:
- drug therapy;
- physiotherapy;
- massage.
The use of folk remedies is possible with the permission of a neurologist, but only as a supplement to taking medications and performing physiotherapeutic procedures. Traditional medicine alone is powerless to combat the disease.
It is important not to let the course of neuralgia take its course. Non-intervention can subsequently provoke serious damage to the nervous system, which will not only provoke prolonged pain, but also paralysis or paresis of the facial muscles, hearing loss, nervous tics and facial asymmetry.
Drug treatment
The basis of therapy is the prescription of carbamazepine drugs and its analogues of new generations. This compound is classified as an anticonvulsant or anticonvulsant. It was first synthesized in the middle of the last century. Subsequently, carbamazepine was improved, as a result of which oxcarbazepine, pregabalin and other anticonvulsants appeared on the pharmaceutical market, causing less side effects and giving a more pronounced effect.
Therapy begins with minimal doses of the selected drug. If there is no positive result, the neurologist gradually increases the dosage until the signs of neuralgia disappear. Treatment is continued for at least 30 days, after which a decision is made about the possibility of reducing the dose. If attacks recur, a re-consultation with a doctor and a new review of the dosage is required.
In approximately half of the cases, it is possible to completely eliminate the pain syndrome and gradually stop taking anticonvulsants. However, their effectiveness progressively decreases as the duration of neuralgia increases. Therefore, patients living with this diagnosis for several years require longer-term use of carbamazepine and its analogues.
Unfortunately, in severe cases, the symptoms of neuralgia sometimes cannot be eliminated even within 10 years. There is also a certain percentage of people who are immune to the drugs used.
Additionally, patients are prescribed:
- muscle relaxants to reduce muscle tone;
- agents that improve blood circulation to normalize nerve nutrition and restore the myelin sheath;
- drugs from the NSAID group that have anti-inflammatory and analgesic effects;
- antidepressants to reduce the speed of pain impulses;
- B vitamins.
Physiotherapeutic treatment
Physiotherapy helps increase the effectiveness of drug treatment and helps reduce the dosage of medications used. For these purposes, courses are prescribed:
- UVR - the use of mid-wave ultraviolet irradiation leads to the active release of neurotransmitters responsible for inhibiting excitation. Traditionally, the course includes 10 procedures.
- Laser therapy – thermal laser energy can reduce the sensitivity of nerve fibers. Usually 10 sessions of 4 minutes are prescribed.
- Diadynamic currents - the method involves fixing electrodes in the area of the most sensitive points, including the nasal mucosa, if required. An electric current with a frequency of 50,000 Hz, called Bernard current, is passed through them. This helps lower the pain threshold and block the transmission of nerve impulses along the trigeminal nerve. Thanks to this, complete pain relief can be achieved. The addition of electrophoresis increases the effectiveness of the procedure. As a rule, to obtain a good effect, several courses lasting 5 days are required. Between them there are breaks for a week. Each session takes about a minute.
- UHF - high frequency currents have proven themselves in the treatment of neuralgia. Their impact leads to improved blood circulation and lymph flow, as well as restoration of the sodium-potassium nerve membranes transmitting impulses. Patients are recommended to undergo 15 to 20 sessions, each lasting 15 minutes.
- Electrophoresis is a method often used to eliminate pain by injecting painkillers directly into the lesion. For neuralgia, novocaine, platyphylline and diphenhydramine are administered using electrophoresis. They block the transmission of nerve impulses by acting on potassium-sodium channels. To improve the nutrition of nerve fibers, which is especially important when the myelin sheath is destroyed, B vitamins can also be administered. Electrophoresis is carried out 10 times every 2 days.
Acupuncture also gives good results. A targeted effect on the nerve receptors of trigger zones and on similar points on the opposite side of the face helps eliminate pain. The duration of treatment for each patient is selected individually. In some cases, it is necessary to install needles for a fairly long period of time - more than a day. But often several procedures are enough to obtain pronounced results.
Massage
Manual influence on the muscles of the face, neck and head as a whole during remission of the disease helps to activate lymph and blood flow. Therefore, massage is indicated for patients with trigeminal neuralgia. A correctly performed procedure helps prolong the remission of the disease, but requires highly qualified chiropractor.
The procedure is carried out very carefully. When performing it, the techniques of rubbing, stroking and vibration are used, but the impact on trigger zones is completely excluded. A massage session performed by an insufficiently qualified specialist can provoke an attack of pain.
Procedures
An alternative for patients who are contraindicated for complex operations, but drug and physiotherapeutic treatment does not provide an effect, may be the following procedures during an exacerbation:
- Injection of glycerin with a hollow needle through the cheek . The procedure allows you to influence the fibers responsible for pain, but careful monitoring of the procedure is problematic. Only 80% of patients experience real relief.
- Balloon compression . It is carried out through the skin using a catheter. A big plus of the procedure is the ability to provide immediate pain relief. Disadvantage: Requires general anesthesia.
- Stereotactic rhizotomy under the influence of electrical impulses . The pain relief effect is high, but in addition to eliminating the symptoms of neuralgia, unfortunately, nerve cells also die. Like balloon compression, the procedure requires general anesthesia.
- Development of hypochondria, depression.
Prevention
Inflammation of the trigeminal nerve is not only important to treat promptly. It is important to prevent relapses, and here prevention plays a huge role:
- Avoid any drafts . It is important and necessary to ventilate the room, but do not get exposed to drafts of air, do not work, do not sleep under the air conditioner.
- Avoid hypothermia of the face and head . Don't ignore hats and scarves during the cold season.
- Protect your head and face from injury.
- Visit your dentist regularly . Avoid periodontitis (inflammation of the tissue around the roots of the teeth). If you treat caries, pulpitis, and periodontitis in a timely manner with modern dentistry, you can avoid it.
- Be careful about herpes . This is not just a “cold on the lips”, but a disease that can provoke the occurrence of ternary neuralgia.
- Fight psycho-emotional stress . Meditate.
- Take up exercise therapy . Focus on exercises that are aimed at working muscles (improving their tone) and increasing heart rate (cardio training).
Remember! Relapses are cyclical. Moreover, exacerbations are more common in the autumn-spring period. Therefore, at this time, pay the most attention to prevention.
Technique
Radiofrequency deinervation is carried out with insulated needles 100 mm long with a working bare end at a 5 mm cut. Under visual control, the tip of the needle is placed into the foramen ovale through the 3rd division of the trigeminal nerve into the Gasserian ganglion.
After installing the needle, low current stimulation is carried out at a frequency of 100 Hz for sensory fibers and 2 Hz for motor fibers, while a tingling sensation at less than 0.5 V indicates the optimal approach of the needle to the affected nerve. The nerve is stimulated with current and the desired branch of the trigeminal nerve is searched. After identifying the branch, the ablation procedure is carried out - the tip of the needle is heated to 70 C for 90 seconds or in pulsed radiofrequency ablation mode 42 ° C for 120 seconds. Low temperature conditions do not cause burns. This leads to healing of the inflamed nerve.
Consequences and complications
It is important to start treating neuralgia in a timely manner. Untimely treatment is fraught with the following complications:
- Continuous pain (both headaches and facial pain).
- Paralysis of the facial nerve and, as a result, facial asymmetry.
- Weakening of hearing and vision.
- Weakening of facial muscles, appearance of wrinkles.
- Behavioral disorder. Constant fears. The person constantly thinks that he may have another attack. Therefore, he tries to move minimally when chewing (or chews, moving food behind one cheek), and smile a little.