Recovery
The skull repair procedure may vary depending on the type of surgery performed and the physical condition of the patient.
As a rule, they try not to keep the patient in for too long and, when the condition stabilizes, they are sent home to more quickly restore the rhythm of life. A long stay does not allow the immune system to strengthen, which leads to an increased risk of getting an infection in the hospital or after discharge. After the operation, the patient is transferred to a ward where his condition is constantly monitored. After getting rid of anesthesia, the breathing tubes are removed, and then the patient is sent to the neurology and intensive care department for further observation, the period of which does not exceed 2 weeks. During this period, you need to lead a sedentary lifestyle as much as possible, try to make as little body movements as possible.
After discharge, you should take all medications prescribed by your doctor, but you should not exceed or, conversely, decrease the dosage without first consulting your doctor. The patient is prohibited from driving, performing any physical or mental activity, or performing exercises until the doctor gives permission. Not following your doctor's instructions may cause difficulty in recovery and unwanted side effects in the future.
Once cleared by your surgeon, you can begin a program of early exercise, such as stretching your neck and back. You should also take frequent walks in the fresh air, although initially their duration should be minimal.
The recovery process can last up to 4 weeks, and by the final date it will be possible to return to your normal work
However, you will still need to take precautions until your rehabilitation is complete, which can last up to 3 months. Ignoring your doctor's instructions may result in the above consequences, as well as paralysis, loss of mental function, and permanent brain damage.
Craniotomy or craniotomy is a complex medical operation known since ancient times. It is carried out in special cases when the doctor needs to gain access to the brain and its membranes, emerging pathologies and blood vessels. Modern medicine makes surgery safer for the patient compared to past times when it was associated with high mortality.
Discussion
Transpalpebral approach appeared in neurosurgical practice relatively recently. The desire to minimize surgical aggression has led to the use of approaches that have already proven themselves in orbital and plastic surgery. Using the concept of minimalism in neurosurgery to protect the brain from concomitant trauma, combined with skin incision along the natural crease of the upper eyelid, provides excellent functional and cosmetic outcomes. Transorbital access is the shortest and most focused route to the pathology of the PCN and the chiasmal-sellar region.
Traditional approaches include various modifications of pterional craniotomy in the form of orbitopterional, orbitozygomatic, transcavernous, supraorbital craniotomy. Despite their versatility and prevalence, they require a fairly large incision of soft tissue, significant devascularization and denervation of the temporal muscle, which leads to its atrophy and dysfunction of the temporomandibular joint, numbness of half the head against the background of damage to the frontal branch of the facial nerve, and traumatic alopecia. The already established transnasal endoscopic approach is ideal for most pituitary adenomas and craniopharyngiomas. However, if the tumor is located in the anterior parts of the PCN or with significant prechiasmatic and lateral spread beyond the supraclinoid part of the internal carotid artery, the use of the transnasal approach is limited.
When compared with the classic supraorbital keyhole approach, proposed and popularized by A. Perneczky, TPC has a number of important advantages. An incision along the eyebrow can lead to traumatic alopecia and scar formation. And the skin incision along the upper eyelid is camouflaged in a natural fold and is made below the projection of the supraorbital nerve and the frontal branch of the facial nerves, which eliminates the corresponding complications and provides an excellent cosmetic result. At the same time, complications such as numbness of the supraorbital region and weakness of the frontal muscle are excluded. Thin skin in the eyelid area ensures rapid healing of the wound. The consequence of these factors is the rapid recovery of patients, their early activation and satisfaction with the cosmetic effect.
Often, an incision along the upper eyelid is used in plastic surgery for blepharoplasty and in ophthalmic surgery for the removal of space-occupying formations of the orbit. We used it in the surgery of space-occupying lesions of the anterior quadrant and anterior circulation aneurysms.
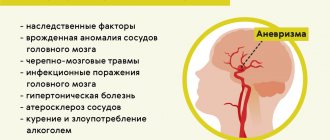
Among aneurysms, we gave preference to localization in the area of the ophthalmic and supraclinoid segments of the ICA, the anterior cerebral artery - the anterior communicating artery. In our opinion, this approach can also be used for aneurysms of the M1 segment of the middle cerebral artery. We used TPC only for unruptured aneurysms and aneurysms in the cold period of hemorrhage, 20 days after subarachnoid hemorrhage. In the acute period of hemorrhage, the use of traditional approaches or the classic supraorbital mini-access is justified. Complex and giant aneurysms also dictate the use of extended craniobasal approaches.
The key principles of working through keyhole approaches in the form of early brain relaxation facilitate maneuvering and create conditions for the use of traditional microsurgical techniques. Pre-placement of a lumbar drain is used if the tumor prevents rapid access to the cisterns. The main tenets of key-hole surgery include the principle of “wait, then see.” Therefore, knowledge of cisternal neuroanatomy and significant experience working through traditional approaches are critical. In order to increase visibility and control at the final stages of tumor dissection, endoscopic assistance is used. Along with opening of aneurysms, intraoperative fluorescein angiography with indocyanine green makes it possible to monitor the adequacy of clipping.
TPK has its limitations and disadvantages, which are common to all keyhole accesses. These include insufficient lighting and work space, and the risk of penetration into the frontal sinus. In some cases, the neurosurgeon has to demonstrate “acrobatic” dexterity in order to work in a limited field, which, theoretically, with insufficient experience, can jeopardize the outcome of the surgical intervention. Solutions to these problems include adequate patient selection, careful preoperative preparation, the use of neuronavigation to plan extrasinus access, and the use of frontal sinus mucosal preservation techniques during insertion. In our series, none of the patients developed complications such as the development of mucocele and/or sinus infection.
Currently, global experience in performing TPC in neurosurgical practice is small and requires further evaluation. Thus, N. Andaluz et al. [32-37], analyzing the use of TPC in 5 patients with anterior circulation aneurysms and 3 patients with tumors of the chiasmal-sellar region, noted the absence of complications, excellent cosmetic results and rapid recovery of patients. A number of similar works also emphasize rapid recovery and excellent cosmetic results. However, these studies represent small series of patients. The most impressive is the work of K. Abdel Aziz et al. The authors analyzed the results of treatment of 40 patients with aneurysms of the anterior sections of the circle of Willis (31 patients), 7 patients with meningiomas of the proximal area and 2 patients with formations of the pole of the frontal lobe. Access time varied from 45 to 60 minutes. Among access-associated complications, the authors note the development of periorbital hematoma (1 patient), which required revision, infection from the postoperative wound (2), liquorrhea (1), which required installation of a lumbar drainage for 4 days. The authors characterize TPC as a focused approach to PCF lesions and anterior circulation aneurysms with excellent functional and cosmetic outcomes [38]. The results of our work correspond to the results of similar works by foreign authors.
Craniotomy: when necessary, implementation, rehabilitation
Craniotomy is rightfully considered one of the most complex surgical interventions. The operation has been known since ancient times, when they tried to treat injuries, tumors and hemorrhages in this way. Of course, ancient medicine did not allow one to avoid various complications, so such manipulations were accompanied by high mortality. Now trepanation is performed in neurosurgical hospitals by highly qualified surgeons and is intended, first of all, to save the patient’s life.
Craniotomy consists of creating a hole in the bones through which the doctor gains access to the brain and its membranes, vessels, and pathological formations. It also allows you to quickly reduce the growing intracranial pressure, thereby preventing the death of the patient.
The operation has strict indications, and the obstacles to it are often relative, since in order to save the patient’s life, the surgeon can neglect concomitant pathology. Craniotomy is not performed in terminal conditions, severe shock, septic processes, and in other cases it can improve the patient’s condition, even if there are serious disorders of the internal organs.
Operation for the elite
Arab and Chinese healers in numerous medical manuals recommended trepanation for the treatment of melancholy, tumors, epilepsy, paralysis and many other diseases, as well as the exorcism of spirits. It is believed that the practice of such operations was practiced by European druids, Arab shamans, African sorcerers, and Indian priests. Evidence of trepanations of famous personalities of the 16th-17th centuries has been preserved, as well as the names of craniosurgeons from different countries.
For example, the founder of the Jesuit order, Ignatius de Loyola, was treated for epileptic seizures using trepanation. Duke Albrecht V of Bavaria, Lorenzo Medici, Duke of Urbino, English Prince Rupert, King Nicholas I of Montenegro, Dutch independence fighter William of Orange, philosopher Erasmus of Rotterdam, writer Francois Rabelais were subject to similar influences...
Such a number of eminent persons, many of whom suffered from headaches, visions and premonitions, indicates the practice of ancient priests that had been preserved for centuries - maintaining the sacred functions of leaders. The belief that rulers and leaders were supported by divine powers persisted throughout the Middle Ages, and they tried to strengthen it in every possible way.
In addition, there was a tradition of trepanation of jesters, fools, holy fools, who in various European cultures acted as mystical reflections of kings who fell into the underworld and therefore lost their minds. To a certain extent, such an operation was supposed to restore reason, make the madman a philosopher, seer, owner of new knowledge and abilities.
Historical reference
In neurosurgery, trephination is the making of a hole in some part of the skull to gain direct access to brain tissue. However, such surgery should not be considered an invention of modern medicine. Archaeological finds indicate that our ancestors could have drilled holes in the skull for medicinal purposes several thousand years ago. Since the Late Paleolithic era (40-11 thousand years ago), trepanation has been used in almost all corners of the planet. The operation was used by ancient Greek and Roman doctors, healers of several parts of Africa, South America and the South Pacific.
Hippocrates proposed trepanation as a way to treat head wounds, including removing bone fragments from the brain after injury. For this procedure, his followers came up with a special drill. Prehistoric trepanations in the culture of ancient civilizations of Peru were performed with a ceremonial knife called a tumi. Residents of the southern regions of the Pacific Ocean performed surgery using sharply sharpened shells. In Europe, flint and obsidian were used for the same purposes.
The purpose of trephination was not always to open access to the brain for further manipulation. In ancient times, a hole in the skull often served as an outlet for evil spirits, which were considered the cause of disease. Also, the hole in the skull was seen as a kind of channel for obtaining special knowledge and spiritual experience. In Egypt, pharaohs underwent such an operation, presumably to make it easier for the soul to leave the body after death.
From Hippocrates to the Middle Ages
The procedure for craniotomy was also described by one of the most popular doctors of antiquity, Hippocrates . He advised the use of this type of operation (and this is described in detail in his works) to treat cranial injuries, as well as to get rid of epilepsy. In his work “On Head Wounds,” the ancient doctor described in great detail the structure of the skull and the types of injuries for which intervention was indicated.
Article on the topic
Wheel of history. What is Hippocrates famous for? Five centuries later, Galen used this Hippocratic base to perform the trephination procedure for hydrocephalus.
In the Middle Ages, aesculapians became skilled in matters of neurosurgery. For them, this method of treatment was an excellent option for relieving a person of constant headaches and cramps. At the same time, as notes preserved from those times note, the doctor had to be strong enough, because after cutting the skin, he needed to break the bones of the skull with tools like a chisel and a hammer. And it was necessary to act in such a way as not to damage the brain. After the operation, the hole in the head was not closed, but simply covered with skin.
Over time, instruments changed, and doctors began to use a special drill for trepanation. Researchers are also surprised by another fact - despite the fact that there was no anesthesia at that time, the percentage of surviving patients was quite high.
Consequences after craniotomy
The severity of the consequences in the postoperative period depends on the reason for the operation, the age of the patient, and the presence of concomitant diseases. If neurological disorders were not immediately detected after trepanation, this does not mean that they will definitely not arise in the future. If the cerebral cortex is damaged, hearing and vision impairment of varying severity, up to complete loss, may occur.
The consequence may be a stroke due to thrombosis or thromboembolism. During trephination for abscesses, pathogenic flora may spread through the membranes of the brain, which will lead to meningitis and encephalitis. After many hours of anesthesia, disorders of the respiratory and cardiovascular systems are possible. If the neurovascular bundles are damaged, numbness, complete loss of sensitivity, and movement of certain areas of the skin, muscles, and limbs are possible. Postoperative consequences can manifest themselves in the form of mental and behavioral disorders.
Surgical treatment of wounds of soft tissues of the head
In the presence of wounds of the soft tissues of the head, the operation begins with the preparation of the surgical field. The hair around the wound is shaved. The wound is washed generously with a 3% hydrogen peroxide solution to remove small foreign bodies, hair, etc.
The edges of the wound are carefully treated with an antiseptic. The antiseptic solution should not get into the wound itself. The edges of the wound are then infiltrated with an antibiotic solution acceptable for endolumbar administration (penicillin sodium salt, kanamycin), based on 0.5% novocaine. This achieves both local anesthesia and prevention of wound infection.
The needle should be inserted near the edge of the wound through the skin, but not through the wound surface itself (Fig. 39).
Inserting a needle through the wound surface promotes infection deeper into undamaged tissue and provokes the development of suppuration in the postoperative period.
Rice. 39. Place of needle insertion during primary surgical treatment of soft tissue wounds of the head:
a – through intact tissue (correct); b – over the edge of the wound (incorrect)
Excision of the edges of the wound is carried out taking into account the location of the arterial trunks so that as little as possible gets into the incisions. Excision must be economical and performed in such a way that after suturing the wound, the underlying tissue (bone, dura mater) is necessarily covered with soft tissue. In cases where, due to extensive soft tissue defects or excessive excision during PSO, the bone remains uncovered, there is a danger of necrosis, infection and osteomyelitis of the bone. If it is still not possible to cover the exposed bone due to a lack of soft tissue, then proceed as follows. In the area of the bone that cannot be covered, the outer compact plate is removed to the diploic layer using a rotator equipped with a spear. It is desirable to form an almost continuous area from the removed outer plate. This creates conditions for the growth of granulation tissue and subsequent favorable engraftment of skin grafts. The rules for suturing wounds of soft tissues of the head are outlined at the end of the chapter.
How is craniotomy performed?
There are 6 main steps during a craniotomy. Depending on the underlying problem being treated and the complexity, the procedure may take 3 to 5 hours or more.
Step 1 - patient preparation. No food or drink is allowed after midnight the night before surgery. Patients with craniotomy are admitted to the hospital in the morning. General anesthesia is administered intravenously while the patient lies on the operating table. The person falls asleep, and his head is in a 3-pin cranial fixation device, which is attached to the table and holds the head in an upright position during the procedure. Inserting a lumbar (spinal) drain into the lower back helps remove cerebrospinal fluid (CSF), allowing the brain to relax during surgery. The patient may be given the drug Manit, which relaxes the brain.
Step 2 - skin incision. After the scalp has been coated with antiseptic, a skin incision is made, usually behind the hairline. The surgeon tries to ensure a good cosmetic result after the operation. Sometimes the hair can be shaved sparingly.
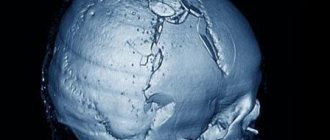
Step 3 - performing a craniotomy, opening the skull. The skin and muscles rise to the bone. Next, the surgeon uses a drill to make one or more small holes in the skull. By inserting a special saw through the holes of the burrs, the surgeon reduces the contour of the bone flap. The cut piece of bone is lifted and exposed to the protective covering of the brain called the dura mater. The bone flap is stored securely until it is replaced at the end of the procedure.
Step 4 - opening the brain. After opening the dura mater with surgical scissors, the surgeon places it back to expose the brain. Retractors placed on the brain need to be repaired or removed. Neurosurgeons use special magnifying glasses (loupe, or operating microscope) to see fine nerves and blood vessels.
Step 5 - fix the problem. Because the brain is tightly enclosed within the bony skull, tissue cannot be easily moved to the side, making it difficult to access and correct any problems. Neurosurgeons use a variety of very small instruments to work deep within the brain. These include long-handled scissors, dissectors, drills, lasers, ultrasonic aspirators (to break up tumors and suck up debris), and computer imaging guidance systems. In some cases, monitoring is used to stimulate specific cranial nerves while the response is monitored in the brain. This is done in order to preserve the function of the nerves and ensure that they are not damaged later during the operation.
Step 6 - closing the craniotomy. With the problem of removing or repairing retractors, the dura mater, closed with sutures, is also removed from the brain. The bone flap is placed back in its original position and secured to the skull with titanium plates and screws. The plates and screws are permanently left to support the skull, which can sometimes be felt under the skin. In some cases, drainage tubes may be placed under the skin for several days to remove blood or surgical fluid. The muscles and skin are stitched back together.
The entire procedure lasts 180-240 minutes.
News
A generally accepted tactic for the treatment of acute traumatic intracranial hematomas and foci of brain contusion is their early diagnosis and removal before the development of brain dislocation and irreversible changes in the brain stem structures. The conditions for revision of intracranial formations and radical removal of all foci of brain damage are: the correct location of the burr window in relation to the traumatic focus and a sufficient size of the burr hole. trephination method ) is influenced by a large number of factors: type, volume, localization of the intracranial traumatic focus, the presence of comminuted fractures of the bones of the calvarium, the severity of manifestations of secondary factors of brain damage (edema, ischemia). Equipping the hospital with diagnostic equipment, the traditions of the department and the personal experience of the surgeon are also of no small importance.
Trephination can be resection, after which a hole is left in the skull, and osteoplastic (KPTCH), when the sawed bone flap is placed in place, covering the trepanation window. If for some reason it is impossible to save the bone flap (for example, the presence of a depressed fracture at the site of the proposed trepanation), then the trepanation hole is closed with a foreign material (acrylic plastics, medical cement, metal plate, etc.). This type of trepanation is called alloplastic. Thus, during plastic surgery, the bone defect in the skull is closed. Separately, there is decompressive craniotomy (DTC), proposed back in 1905 by N. Cushing, the purpose of which is to create additional reserve intracranial space with increasing swelling and prolapse of the brain or with a high probability of developing these processes after removal of the traumatic focus [1]. DST is performed by removing a fragment of the bones of the cranial vault, dissection, and then plastic surgery of the dura mater (DRM). Resection trepanation is performed by resection with nippers or cutting out a bone flap from the burr holes with a Geeley saw and removing it.
There are one- and two-sided craniotomies . Depending on the location of the traumatic focus, when planning surgical access, trepanations are distinguished: • in the frontal region (unilateral frontal, bifrontal) - for access to the frontal lobes and formations of the anterior cranial fossa; • in the temporal region (temporal) – most often performed in case of traumatic brain injury (TBI), to access the formations of the middle cranial fossa; • in the frontotemporal region (frontolateral, pterional) – for simultaneous access to the formations of the anterior and middle cranial fossae; • in the frontal-temporo-parietal region - used for extensive areas of contusion and crushing of the brain, for revision of the pole-basal sections of the frontal and temporal lobes; if necessary, decompressive trepanation can be performed from such access; • in the parietal region; • in the occipital region; • trephination of the posterior cranial fossa – for access to subtentorial lesions (median and paramedian suboccipital trepanation) [2, 3].
The advantages of KPTCH are: the ability to preserve one’s own bone tissue to close the trepanation defect, to avoid future repeated cranioplasty operations and the development of “trephine syndrome.” When using KPTCH, there is no influence of external atmospheric pressure on the brain substance, which leads to a more rapid restoration of cerebral circulation in ischemic tissues in the postoperative period. Simultaneous plastic surgery of a bone defect performed during surgery significantly reduces the period of temporary disability and improves the quality of life of patients.
Technique for performing KPTCH.
The position of the patient on the operating table depends on the location of the intracranial lesion. As a rule, trepanation in the frontal, temporal and parietal regions is performed with the patient in the supine position; during trephination in the occipital region or in the posterior cranial fossa - on the side, stomach or while sitting. When positioned on the back, it is necessary to ensure that the patient’s head is elevated in relation to the body by 10–15° and rotated from the vertical line, depending on the objectives of the surgical approach. A low head position impedes venous drainage from the cranial cavity, which can lead to increased intracranial pressure (ICP). The line of the skin incision should be formed taking into account the shape, size and location of the bone flap, as well as depending on the course of the main neurovascular trunks of the skin. To project the topography of the lobes, sulci and convolutions of the brain, various schemes can be used (Kronlein, Taylor-Haughton). Bleeding from damaged skin vessels is stopped by applying hemostatic clamps or using special skin clips. KPTCH can be performed by cutting a free bone flap, a periosteal bone flap, or a bone flap on a musculoperiosteal pedicle. The dura mater is opened with an arcuate incision along the perimeter of the bone window, departing from it by 0.5–0.7 cm. The dura mater incision should begin in the avascular zone. Coagulation of bleeding vessels of the dura mater is carried out before opening it, since after its dissection the membrane wrinkles and deforms, which prevents its further hermetically suturing. After the main stage of the operation (removal of hematoma, foci of contusion and crush of the brain), the dura mater should be sutured hermetically in order to prevent postoperative wound liquorrhea, subcutaneous hygromas, etc. To prevent the formation of postoperative epidural hematomas, the dura mater is sutured and pulled to the periosteum along the perimeter of the bone defect, as well as at its center. In order to create normal anatomical relationships in the wound when performing osteoplastic trephination, the stage of fixing the bone flap is important. The bone flap must be fixed using periosteal or bone sutures with Dacron, wire or absorbable suture material (in children), as well as titanium or plastic craniofixes. It should be remembered that weak fixation of the bone flap can lead in the postoperative period to its migration, deformation of the skull and, as a consequence, to re-operation.
Cerebral edema and ischemia, leading to a decrease in cerebral perfusion pressure (CPP) and the development of intracranial hypertension (IH), are the main pathophysiological processes leading to an unfavorable outcome. The purpose of DTC is to increase intracranial volume, thereby reducing ICP, increasing the level of oxygen tension in brain tissue (PtiO2) and improving the functional state of the brain. However, in practice, it is not always possible to predict the development of postoperative edema or the evolution of foci of brain contusion.
DST is performed, as a rule, in conditions of increasing cerebral edema, and it should be performed in such a way as to level out the conditions of brain infringement. This is achieved by removing the bone flap, dissecting the dura mater and performing its free plastic surgery. Quite often there are incorrect definitions of craniotomies that contradict the meaning of surgical intervention (for example, “osteoplastic decompressive trephination” or “osteoplastic trepanation with delayed fixation of a bone flap”). This confuses the neurosurgeon regarding the correct technique for performing a particular trepanation method. Instead of true DST, plastic trepanation can be performed, which does not produce the clinically desired decompressive effect, and in some cases can worsen the patient’s condition. Sometimes, when performing DST, surgeons do not remove the bone flap, but leave it in the surgical area without fixing it to the edges of the defect and forming a so-called valve or bone valve. According to the authors, after the elimination of cerebral edema, the bone flap falls into place, thereby closing the window in the skull. But since DST is performed to reduce ICP, the preservation of obstacles (bone, dura mater) defeats the purpose of the operation and reduces its effectiveness. Such operations are vicious.
To prevent dislocation of the bone flap when performing osteoplastic craniotomy , it is necessary to firmly fix it to the bones of the skull. It is preferable to use fixation with metal craniofixes or plates. Resection craniotomy is not the same as decompressive craniotomy. If during resection craniotomy the dura mater is not dissected, then there will be no decompressive effect. Decompressive craniotomy is impossible without dissection of the dura mater. Depending on the location of the trepanation window, the following types of DPT are distinguished: • in the temporal region (temporal and bitemporal); • in the frontal region (frontal and bifrontal); • in the frontotemporal region (unilateral and bilateral); • in the occipital region (occipital). DTC can be one- or two-sided. Separately, craniectomy, hemicraniectomy and circular craniotomy are distinguished. During craniectomy, both hemispheres of the skull are resected so that only a strip of bone tissue remains above the superior sagittal sinus. Hemicraniectomy is an operation in which almost the entire hemisphere of the skull is resected on one side. A circular craniotomy is performed by biting a “path” along the largest perimeter of the skull in such a way that the upper part of the skull becomes mobile in relation to the lower. Currently, craniectomy, hemicraniectomy and circular craniotomy are practically not used due to their high traumatic nature. The most commonly used is the infratemporal DTC.
Rules for performing DTC
When performing DST, it is necessary to fulfill a number of requirements, deviation from which reduces the effectiveness of the operation and leads to complications. A prerequisite for performing DST is a large size of the bone defect. The dimensions of the trepanation window should not prevent free prolapse of the brain as long as postoperative edema persists. A small-sized trepanation defect leads to entrapment of the brain matter, compression of the veins, ischemia and infarction of the strangulated area and, as a consequence, an increase in cerebral edema. In addition, conditions are created for additional trauma to the damaged brain. The size of the trepanation window has a significant impact on the outcome of surgical treatment. Thus, in patients with a defect size of 12x15 cm, postoperative mortality is 20% lower and 15% more good functional outcomes than in patients with a trepanation window size of 6x8 cm [4]. The trepanation window is placed closer to the place of attachment of the cerebellar tentorium, since decompression carried out at the level of the intended herniation can prevent or minimize the effect of dislocation of the brain stem at the level of its peduncles; in addition, revision of the basal parts of the frontal and temporal lobes is facilitated. Thus, a trepanation window is placed as low as possible in the temporal region, with resection of the squama of the temporal bone and the greater wing of the sphenoid bone in the area from the external auditory canal to the frontozygomatic suture. Resection of the edge of the temporal bone is mandatory when performing decompressive trepanation . During surgery of acute intracranial hematomas or foci of contusion and crush of the brain, the decompressive effect of the operation largely depends on the location of the trepanation, and DST may not give the desired effect if, due to inaccurate diagnosis, it is performed far from the traumatic focus. When planning the size and localization of a trepanation defect, it is necessary to take into account computed tomography (CT) data of the brain. A correctly applied trepanation window allows for radical removal of the source of damage and revision of the intrathecal space. Another important point when performing DST is the correct opening of the dura mater. It should be cut with a wide incision along the entire perimeter of the trepanation defect with the base facing the base of the skull so as to preserve the feeding arterial vessels (a. meningea media). It is not advisable to use other options for the dura mater incision - cruciform or H-shaped, since with such an incision the area of the trepanation window is reduced by approximately 1/3 (Fig. 4, 5). The most appropriate seems to be an arcuate opening of the dura mater, which achieves the largest decompression area [3].
Scircle=pr2, Ssquare=A2.
For example, with D=6 cm Scircle=28 cm2, Ssquare=18 cm2;
eS=Scircle–Ssquare=10 cm2=36%.
A typical mistake when opening the dura mater during DST is making an incision directly along the edge of the bone defect. In this case, the bony edge of the trepanation window remains uncovered by soft tissue, which creates conditions for greater trauma to the brain substance during intraoperative swelling. To avoid these undesirable complications, the dura mater should be opened along the perimeter of the bone window, stepping back from it by 0.5–0.7 cm. In addition, the remaining edge of the dura mater can be used to suture a graft to it when performing free dura mater plastic surgery (Fig. 6). After removal of the hematoma, foci of contusion and crushing of the brain, free plastic dura mater should be used as a mandatory step in the treatment of DTS. It is performed to create a sufficient volume during protrusion of the brain substance, subject to reliable separation of the brain and soft tissues in order to prevent the subsequent adhesive process between the brain and the soft integumentary tissues of the skull. A defect in the dura mater is usually replaced with plastic material. The best results are obtained by using dura mater prostheses made from modern synthetic materials (for example, polytetrafluoroethylene) or based on processed collagen. You should not use muscle, femoral fascia, aponeurosis, lyophilized cadaveric membrane as plastic materials, or even refuse to perform dura mater plastic surgery, as this promotes the fusion of the brain with autologous tissues. The area of the dura mater prosthesis must be large enough to prevent contact of the brain with the aponeurosis and the formation of brain scars. This is very important for the prevention of epileptic seizures in the postoperative period and facilitates subsequent plastic surgery of the skull defect during the rehabilitation of victims. After free dura mater plastic surgery, the temporal muscle and aponeurosis are sutured with single interrupted sutures along the perimeter of the bone defect. The aponeurosis should be sutured especially carefully, because it is it that will hold the wound after removing the skin sutures if the brain prolapse continues in the postoperative period. The consequence and main disadvantage of DTC are skull defects, leading to the formation of a rough meningeal scar, traumatic epilepsy and encephalopathy, and impaired blood and liquor circulation. In addition, in conditions of edema, with significant prolapse of the brain substance into the trepanation defect, there is a risk of divergence of the edges of the postoperative wound with the formation of wound liquorrhea, brain prolapse and the subsequent development of purulent-inflammatory complications. In the late postoperative period, a bone defect leading to skull deformation causes psychological discomfort in patients, and also increases the risk of repeated brain injury.
Choosing a craniotomy method
Attitudes towards decompressive and osteoplastic craniotomy have changed over time and the advent of new technologies in the diagnosis and treatment of severe TBI. Before the use of modern neuroimaging methods, in the surgical treatment of victims with TBI, in the vast majority of cases, preference was given to DST, considering it a necessary component of the operation when removing an intracranial hematoma. DST was often performed for a prophylactic purpose - to increase the volume of the cranial cavity in case of possible progression of cerebral edema in the postoperative period. As clinical experience accumulated, it was noted that in the groups of patients with KPTCH and DTC, the results of surgical treatment practically do not differ from each other, and the method of craniotomy does not have a significant effect on the outcome. With the introduction of CT, magnetic resonance imaging (MRI), and methods for measuring ICP, the indications for the use of DPT have narrowed significantly. Most often, the question of choosing a method of craniotomy arises before the surgeon when treating victims who are in a comatose state with large-scale injuries. Unfortunately, in practice we have to deal with insufficient equipment of hospitals with modern diagnostic equipment and a lack of opportunities for multimodal neuromonitoring. Then you have to rely on the data of a clinical neurological examination and CT scan of the brain, and in some cases, only on the clinical picture of the victims.
Indications for osteoplastic and decompressive craniotomy
Until the 80s of the 20th century, in the surgical treatment of patients with severe TBI, DST was used in the vast majority of cases. As a rule, DST was performed for a prophylactic purpose - to increase the volume of the cranial cavity in case of possible progression of cerebral edema in the postoperative period, although edema did not develop in all cases. Over time, a tendency gradually emerged to use one or another method of craniotomy, depending on the intraoperative state of the brain substance. It was noted that performing osteoplastic craniotomy in the acute period of TBI can significantly reduce the period of temporary disability, and long-term results of surgical treatment of patients are largely determined by the severity of TBI, the volume of surgical intervention and to a lesser extent depend on the method of trephination. Currently, the optimal method of craniotomy is osteoplastic. Proponents of osteoplastic trepanation advise its use even for patients in serious condition, regardless of the type of lesion. Osteoplastic trephination, as a rule, is used for single intracranial hematomas of convexital location and small volume, when the possibility of developing acute edema of the brain substance in the postoperative period is excluded. The selection criterion is the compensated state of the patients: preservation of consciousness, stable indicators of the cardiovascular and respiratory systems, the initial stages of the development of dislocation syndrome. DST is performed during intraoperative prolapse of the brain substance, its increasing swelling and dislocation, with a high probability of the development of these processes after removal of large (more than 100 cm3) traumatic subdural and intracerebral hematomas, in the presence of massive areas of contusion and crushing of the brain, and especially with their combinations - pathology, provoking the rapid development of cerebral edema with subsequent dislocation and compression of its trunk. It is also recommended to use decompressive trepanation for extensive lesions of brain matter with mass effect, located in the poles of the frontal and temporal lobes. One of the decisive factors when choosing decompressive trepanation is the presence in the clinical picture of respiratory and hemodynamic disorders, which are signs of the late stages of dislocation syndrome - the mesencephalic and pontine stages. Carrying out DTC can be considered justified if there is a persistent increase in ICP to a level of 35–40 mm Hg. Art. for a period of 30 minutes to 48 hours, refractory to conservative therapy. It is not advisable to perform DST in cases of primary damage to the brain stem [4–7]. In order to determine the optimal method of craniotomy for severe TBI at the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky conducted a prospective randomized study of 73 patients who underwent surgical treatment for TBI. A comparison was made of a group of patients who underwent DTC or CPTC. The groups were compared by gender, age, time from the moment of injury to surgery, level of consciousness before surgery, volume of the lesion, size of lateral dislocation, degree of axial dislocation. We did not find any significant differences in these parameters (p>0.05). The conditions for inclusion of victims in the study were developed based on a retrospective analysis of the results of surgical treatment of 1082 victims with TBI. We also assessed the results of ICP monitoring during surgery and in the postoperative period. Risk factors that influenced the outcome of surgical treatment of victims in the groups were identified: clinical - the age of the patients, the degree of wakefulness before surgery and neuroimaging data - the volume of damage, the magnitude of lateral and degree of axial dislocation, the value of the 2nd ventriculocranial coefficient (VCC-2). Analyzing the dynamics of changes in ICP during surgery and in the postoperative period of victims who underwent removal of a traumatic intracranial lesion, we identified 3 types of pressure changes. In the first type, a significant decrease in ICP was noted during surgery, regardless of the initial level. The maximum reduction in ICP to normal levels occurred at the stage of hematoma removal. By the end of the operation, ICP did not exceed a critical level (20 mm Hg). In all victims, there was a slight increase in the next day, but by the 2nd day the ICP level decreased slightly and did not exceed the normal value. Type 2 was characterized by a decrease in ICP to a normal level at the end of the operation and a significant tendency to increase in the first 2 days after surgery. In type 3, the maximum decrease in ICP was noted at the stage of hematoma removal, but by the end of the operation the ICP level significantly exceeded normal values and remained high thereafter. The study showed that there was no significant difference in the outcomes of surgical treatment in patients with KPTCH and DTC, prospectively selected into groups according to given parameters. We emphasize once again that our study was carried out on victims whose intraoperative brain state allowed for CBTC to be performed. We have not obtained convincing data on the unequal impact of extracranial and intracranial factors in the studied groups [8, 9]. The conducted studies allowed us to give recommendations for performing DTC: 1. VH uncontrollable by intensive therapy methods in combination with the clinical picture of the victim and brain CT data (ICP level in the postoperative period is more than 40 mm Hg, late stages of development of dislocation syndrome with violation of vital functions, diffuse cerebral edema with signs of gross axial dislocation). 2. Intraoperative manifestations of edema and swelling of the brain. 3. The presence of multiple intracranial injuries (a combination of subdural, intracerebral hematomas and foci of brain contusion) with a simultaneous decrease in the value of VKK-2, according to brain CT, less than 8% in young patients (up to 50 years). 4. II or III type of ICP dynamics.
Literature
1. Cushing H. Subtemporal decompressive operation for the intracranial complications associated with bursting fractures of the skull. Ann Surg 1908; 47. 2. Lebedev V.V., Krylov V.V. Emergency neurosurgery: A guide for doctors. M.: Medicine, 2000. 3. Lebedev V.V., Krylov V.V., Tkachev V.V. Decompressive craniotomy. Neurosurgery. 1998; 2:38–43. 4. Jiang JY, Xu W, Li WP. Efficacy of standard trauma craniotomy for refractory intracranial hypertension with severe traumatic brain injury: a multicenter, prospective, randomized controlled study. J Neurotrauma 2005; 22: 623–8. 5. Guerra WK, Gaab MR, Dietz H et. al. Surgical decompression for traumatic brain swelling: indications and results. J Neurosurg 1999; 90: 187–96. 6. Guidelines for the management of severe traumatic brain injury. Brain Trauma Foundation, American Association of Neurological Surgeries, Joint Sections on Neurotrauma and Critical Care. J Neurotrauma 2000; 17: 451–627. 7. Polin RS, Shaffrey ME, Bogaev CA et al. Decompressive bifrontal craniectomy in the treatment of severe refractory posttraumatic cerebral edema. Neurosurgery 1997; 41: 84–92; discussion 92–94. 8. Krylov V.V., Talypov A.E., Puras Yu.V. Intracranial pressure in brain injuries. Neurosurgery. 2007; 4:12–9. 9. Puras Yu.V., Talypov A.E., Krylov V.V. Criteria for choosing methods of craniotomy in victims with severe traumatic brain injury. Honey. disasters. 2008; 1:32–8.
Journal of Surgery No. 1. year 2009.
Similar articles:
Articles → Selective neurotomy in the treatment of focal spastic syndrome.
News → Features of traumatic brain injury in children
Articles → Mild traumatic brain injury
Articles → Pathophysiology of headache in patients in the recovery and long-term periods of mild traumatic brain injury
Articles → Electrophysiological studies of the optic nerve in patients at various times after traumatic brain injury
Craniotomy - types
To eliminate many pathologies, trepanation is used, the types of which are named based on the location of access to the brain and the method of performing the operation. The bones of the skull (on the vault) are represented by several plastics, covered with periosteum on top and adjacent to the braincase below. If the periosteum, as the main nourishing tissue, is damaged, there is a risk of necrosis and bone death. To avoid this, craniotomy is performed using the following methods:
- classical osteoplastic;
- resection;
- for the purpose of decompression;
- conscious operation;
- Stereotaxy is a study of the brain using a computer.
Osteoplastic craniotomy
The most famous type of craniotomy, a classic method of opening the skull, during which a small section of the parietal bone is sawed out without damaging the periosteum. The cut piece is connected with the periosteum to the cranial vault. The pedicled skin flap is folded back and, after the operation, is placed in place or removed. The periosteum is sutured. After surgery, no bone defect is observed. Trepanation (osteoplastic) of the skull is divided into two types:
- With cutting out a skin-periosteal-bone flap at the same time (according to Wagner-Wolf).
- With cutting out a skin-aponeurotic flap, which has a wide base, and then an osteoperiosteal flap on a narrow stalk (Olivecron trepanation).
Decompressive trephination
One of the methods designed to reduce intracranial pressure and improve the condition (and function) of the brain is decompressive craniotomy (DCT) or Cushing trephination, named after the famous neurosurgeon. With it, a hole is created in the bones of the skull, through which the harmful element that caused the resulting hypertension is eliminated. This could be pus, blood, cerebrospinal fluid, or edematous fluid. Negative health consequences after surgery are minimal, rehabilitation is short.
Resection trepanation
Resection surgery has a less favorable prognosis for rehabilitation; craniotomy is performed by applying a burr hole and then expanding it to the required size (for this, wire cutters are used). The sawed area is removed along with the periosteum without possible restoration. The bone defect is covered with soft tissue. As a rule, this technique is used when trepanation of the posterior cranial fossa is necessary, as well as treatment of cranial wounds.
Awake craniotomy
One of the modern methods of surgery is trepanation without anesthesia. The patient is conscious, his brain is not turned off. He is given relaxation drugs and local anesthesia is injected. Such intervention is required when the pathological area is located too close to the reflexogenic zones (and there is a danger of damaging it). During the operation, surgeons constantly monitor the patient’s condition and the activity of organs, monitoring the process.
Osteoplastic trepanation
Osteoplastic trephination aims not only to open the skull, but also to penetrate inside for various manipulations (removal of hematoma and crush areas after injury, tumor), and its end result should be restoration of the integrity of tissues, including bones. In the case of osteoplastic trepanation, the bone fragment is returned to its place, thus eliminating the formed defect, and a repeat operation is no longer required.
In this type of operation, a burr hole is made where the path to the affected area of the brain will be the shortest. The first step is a horseshoe-shaped incision into the soft tissues of the head. It is important that the base of this flap is at the bottom, since the vessels supplying the skin and underlying tissue run radially from bottom to top, and their integrity must not be compromised to ensure normal blood flow and healing. The width of the base of the flap is about 6-7 cm.
After the musculocutaneous flap with the aponeurosis is separated from the surface of the bone, it is turned down, fixed on napkins soaked in saline solution or hydrogen peroxide, and the surgeon proceeds to the next stage - the formation of the osteoperiosteal flap.
stages of osteoplastic trepanation according to Wagner-Wolf
The periosteum is cut and peeled off according to the diameter of the cutter, which the surgeon uses to make several holes. The sections of bone preserved between the holes are cut out using a Gigli saw, but one “lintel” remains intact, and the bone in this place is broken. The bone flap will be connected to the skull through the periosteum in the area of the fractured area.
To ensure that the fragment of the skull bone does not fall inward after being placed in its original place, the cut is made at an angle of 45°. The area of the outer surface of the bone flap turns out to be larger than the inner one, and after this fragment is returned to its place, it is firmly fixed in it.
Having reached the dura mater, the surgeon dissects it and enters the cranial cavity, where he can perform all the necessary manipulations. After the intended goal is achieved, the tissues are sutured in the reverse order. Sutures of absorbable threads are placed on the dura mater of the brain, the bone flap is returned to its place and fixed with wire or thick threads, and the musculocutaneous area is sutured with catgut. It is possible to leave a drainage in the wound for the outflow of discharge. The sutures are removed by the end of the first week after surgery.
Video: performing osteoplastic trepanation
Rehabilitation after craniotomy
The first day after the end of the operation, the patient is in intensive care, connected to devices. The next 3-7 days should be spent in a hospital under the supervision of doctors. This period of time allotted for recovery after craniotomy is very conditional; if a person experiences complications, it can increase. During the rehabilitation period, the patient is prescribed medications:
- painkillers;
- antibiotics - to prevent inflammation;
- antiemetics;
- sedatives;
- anticonvulsants;
- steroid drugs that remove excess water from the body.
The sterile dressing is removed from the wound within 24 hours. The skin around the wound should be constantly treated and kept clean. After 2 days, the patient is allowed to get up and walk a little. After discharge home, rehabilitation continues. The following conditions must be observed:
- do not lift objects weighing more than 3 kg;
- stop smoking;
- eliminate nervous unrest;
- take a course with a speech therapist to restore speech;
- bend over as little as possible;
- go on a diet prescribed by a doctor;
- Take short, supervised walks every day.
You should very carefully monitor the emotional state of a person after surgery. Some people become susceptible to depression and nervous disorders
It is necessary to surround them with care and attention, to protect them from unnecessary worries. If you can’t cope with anxiety on your own, you need to consult a psychologist.
Looking for new answers
Dr. Bart Hughes in the early 60s of the 20th century wrote about craniotomy as an opportunity to achieve a harmonious state of mind, awaken creativity and mental balance. By the way, before starting to actively promote trepanation, Hughes made a hole with a diameter of about 6 mm in his own skull and only after that began to look for supporters of his theory.
Not far from Oxford, in an ancient castle, the walls of which are decorated with family portraits, live Lord James Neidpath (former teacher of US President Bill Clinton) and his wife Amanda Fielding (artist). After meeting Hughes, they performed a trepanation. Amanda actively promotes the operation, saying that the procedure improves mental abilities, sharpens perception and gives vitality.
Moreover, the actress believes that when acting on stage she gains additional emotionality and a more acute understanding of the heroines whose roles she plays. Amanda is working to ensure that trepanations are accessible and that doctors officially do it at the request of patients.
Bart Hughes believes that this is one of the most effective ways of self-knowledge, achieving a higher level of consciousness, in comparison with such a way of heightening the senses as drug use. Amanda not only listened to all of Hughes’s explanations and found them logical, but also, having performed trephination at home, after 4 hours she decided to test the effect of the operation.
She tied a turban around her head and went to a costume ball. According to her, she experienced the euphoria of freedom and relaxation, the richness of perception of the surrounding world and the ease of perception of everything that was happening around.
The press names musician John Lennon among those who want or have carried out the operation, as well as numerous jewelers, professors, art dealers from London, librarians from Amsterdam and farmers from Texas. Some of them have rallied around Amanda as like-minded people in the Trepanation Trust and even sponsor scientific research from medical and philosophical institutions studying this ancient phenomenon at the present stage of human development.
What are the consequences for children and adults?
- Asthenia – constant feeling of fatigue, depression, sensitivity to atmospheric phenomena, insomnia, tearfulness;
- Speech disorders are common in both children and adults. It is difficult to immediately determine whether this phenomenon is temporary. So you just have to wait and watch;
- Psychosis;
- Forgetfulness;
- Paralysis;
- Convulsions (more often in children);
- Loss of coordination (more pronounced in children);
- Hydrocephalus (in children, less often in adults);
- ZPR (in children).
Infectious complication
As after any surgical intervention, trepanation negatively affects the body's protective functions, which increases the risk of infection.
Brain infections are extremely rare, but the wound itself can easily become infected by poorly handling the instruments
The lungs, intestines, and bladder suffer from infection. All these organs tend to catch infections first.
After surgery on the skull, the likelihood of developing a number of infections increases significantly, and infection of the brain tissue itself occurs much less frequently, which is associated with appropriate sterilization of the area undergoing surgery.
The greater risk of infection is the lungs, intestines and bladder, the functions of which are regulated by parts of the brain. This circumstance is largely due to forced restrictions on a person’s mobility and lifestyle changes after surgery. Prevention of such complications is physical therapy, diet, and sleep. Treatment of infections is carried out medically - by prescribing appropriate antibiotics.
Blood clots and blood clots
Pathological processes and changes in brain tissue, poor mobility in the postoperative period can cause blood stagnation, which causes the formation of blood clots. The veins in the legs are most often affected.
If a blood clot breaks loose, it can migrate throughout the body, settling in the lungs or heart. Very often, the detachment of a blood clot leads to death. There are also cases of pulmonary artery thrombosis, which is a very dangerous consequence and requires immediate intervention. This disease leads to very serious consequences, including death.
The best prevention against clots is exercise, plenty of fresh air and anticoagulants (blood thinners).
Neurological disorders
To speed up the healing process, steroidal anti-inflammatory drugs are prescribed.
With more serious errors made during surgery, pathologies may last longer. There are many causes for symptoms, and they all depend on more than one factor.
Bleeding
Bleeding is one of the most common phenomena after trepanation. For several days after surgery, the vessels may bleed. This problem is eliminated by drainage. Usually there is little blood and it does not cause problems.
But there are cases when the bleeding is so profuse that repeated trephination has to be done to stop it and prevent more serious consequences.
Blood that accumulates in the cranial cavity can affect motor centers or nerve endings, causing seizures. In order to avoid such manifestations during surgery, the patient should be given intravenous anticonvulsant drugs in advance.
Implants
There is a list of mandatory qualities that they must have:
- sufficient strength;
- biocompatibility;
- ease;
- plastic;
- do not cause infectious complications;
- do not have a carcinogenic effect.
Implants can be made from the patient's own bone (autografts) or artificial (xenografts).
Autografts
This is bone that has been temporarily removed to access the patient's brain tissue. If the bone needs to be preserved to close a skull defect later, it is placed under the skin of the patient's abdomen or anterior outer thigh. If such preservation is not possible, other techniques using the person’s own bone tissue are used. And if it is impossible to replace the defect with autografts, they resort to materials replacing them.
Xenografts
The so-called “artificial bones” are made of metal (aluminum or titanium), using methyl methacrylate or hydroxyapatite.
Each of the mentioned implants has its own advantages and disadvantages. For example, hydroxyapatite can be used for defects up to 30 square centimeters. This material is completely biocompatible. And it is able to turn into its own bone tissue after 18 months with small defects. And the risk of infectious complications for this type of implant is the lowest among similar ones.
Titanium is the least likely to cause local inflammatory reactions. And from it it is possible to recreate lost fragments of the facial skeleton, the base of the skull, the vault and the walls of the orbit. This is done using simulation and neuronavigation in the preoperative period.
The doctor will help you understand the variety of implants, as well as find out what the latest medical developments in the field of implantology are, during an in-person consultation. Fill out an application on our website and we will make an appointment with a leading specialist in the field of neurosurgery.
In each specific case, it is important to take into account not only the direct benefits for a person, but also the aesthetic and psychological aspects. As well as restrictions imposed on the patient in connection with the choice (for example, a metal implant does not allow the patient to subsequently resort to MRI examination).