General information
The nervous system is represented by various nerve plexuses, peripheral nerves, spinal cord and brain.
Neuropathy is a non-inflammatory lesion of the nervous system. Peripheral nerves have a very thin structure and are not resistant to damaging factors. According to the level of damage they distinguish:
- Mononeuropathy. Characterized by damage to one single nerve. Mononeuropathy is considered a fairly common option. Most often, mononeuropathy of the upper limb is diagnosed (mononeuritis of the radial or ulnar nerve).
- Multiple neuropathy affecting several nerve endings.
- Polyneuropathy , which is characterized by the involvement of several nerves localized in one area.
Clinics for treatment with the best prices
Price
Total: 121in 13 cities
Source
- Excluded
: current traumatic lesions of nerves, nerve roots and plexuses - see nerve injuries by body region, neuralgia, neuritis (M79.2), peripheral neuritis during pregnancy (O26.8), radiculitis NOS (M54.1)
- G50 Trigeminal nerve lesions Includes
: 5th cranial nerve lesions - G50.0 Trigeminal neuralgia
- G50.1 Atypical facial pain
- G50.8 Other lesions of the trigeminal nerve
- G50.9 Trigeminal nerve disorder, unspecified
- Includes
: lesions of the 7th cranial nerve
: postherpetic inflammation of the knee ganglion (B02.2)
- Excluded
: disorders of the auditory (8th) nerve (H93.3), optic (2nd) nerve (H46, H47.0), paralytic strabismus due to nerve palsy (H49.0-H49.2)
- G53.0 Neuralgia after herpes zoster (B02.2)
- Excluded
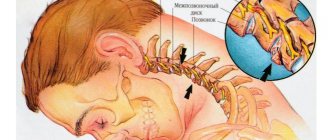
: current traumatic lesions of the nerve roots and plexuses, lesions of the intervertebral discs (M50-M51), neuralgia or neuritis NOS (M79.2), neuritis or radiculitis: brachial NOS, lumbar NOS, lumbosacral NOS, thoracic NOS, radiculitis NOS, radiculopathy NOS (M54.1), spondylosis (M47.-)
- G55.0 Compression of nerve roots and plexuses due to neoplasms (C00 - D48)
- Excluded
: current traumatic nerve damage - see nerve injury by area of the body
- Excluded
: current traumatic nerve damage - see nerve injury by area of the body
: sciatica: NOS (M54.3) associated with intervertebral disc disease (M51.1)
- G58.0 Intercostal neuropathy
- G59.0 Diabetic mononeuropathy (E10 - E14 with common fourth character .4)
Pathogenesis
Neuropathy is usually determined by the nature of the nerve damage and its location. Most often, the pathology forms after a traumatic injury, after suffering from general diseases and during intoxication.
There are 3 main forms of neuropathy:
- Post-traumatic neuropathy. Violation of the integrity of the nerve myelin sheath occurs as a result of acute injury or severe blow. With tissue swelling, improper scar formation and bone fractures, compression of the nerve fibers occurs. Post-traumatic neuropathy is characteristic of the ulnar, sciatic and radial nerves.
- Diabetic neuropathy. Damage to nerve endings is also recorded with high levels of sugar and blood lipids in the blood.
- Toxic neuropathy. As a result of infectious diseases such as herpes , HIV , diphtheria , etc., toxic damage to the nerve plexus occurs. Poisoning with chemical compounds and overdose of certain medications can lead to disruption of the integrity of the nerve trunk.
Neuropathy can develop against the background of a disease of the hepatic system, kidney pathology, osteochondrosis , arthritis , the presence of neoplasms and insufficient levels of thyroid hormones .
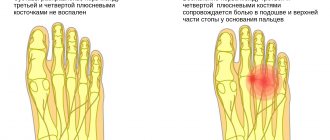
Additional facts
Neuropathy of the peroneal nerve, or peroneal neuropathy, occupies a special position among peripheral mononeuropathies, which also include: neuropathy of the tibial nerve, neuropathy of the femoral nerve, neuropathy of the sciatic nerve, etc. Since the peroneal nerve consists of thick nerve fibers that have a larger layer of myelin sheath, it more susceptible to damage due to metabolic disorders and anoxia. This point is probably responsible for the fairly wide prevalence of peroneal neuropathy. According to some data, neuropathy of the peroneal nerve is observed in 60% of patients in traumatology departments who have undergone surgery and are treated with splints or plaster casts. Only in 30% of cases, neuropathy in such patients is associated with primary nerve damage. It should also be noted that often specialists in the field of neurology have to deal with patients who have a certain history of peroneal neuropathy, including the postoperative period or time of immobilization. This complicates treatment, increases its duration and worsens the result, since the earlier therapy is started, the more effective it is. The superficial peroneal nerve runs along the anterolateral surface of the leg, where it gives off a motor branch to the peroneal muscles, which are responsible for pronation of the foot with its simultaneous plantar flexion. In the area of the medial 1/3 of the leg, the superficial branch of the n peroneus passes under the skin and is divided into 2 dorsal cutaneous nerves - the intermediate and medial. The first innervates the skin of the lower 1/3 of the leg, the dorsum of the foot and the III-IV, IV-V interdigital spaces. The second is responsible for the sensitivity of the medial edge of the foot, the back of the first toe and the II-III interdigital space. Anatomically determined areas of greatest vulnerability of the peroneal nerve are: the place where it passes in the area of the head of the fibula and the place where the nerve exits the foot.
Classification
They are classified according to localization:
- Neuropathy of the lower extremities. The most common diabetic neuropathy of the lower extremities is caused by diabetes mellitus . In this form, the peripheral nervous system innervating the lower extremities is affected.
- Peroneal nerve neuropathy. Characteristically, one peroneal nerve is affected, which is manifested by muscle weakness and impaired sensitivity in the innervated area. ICD-10 code: G57 – mononeuropathies of the lower extremities.
- Distal axonal neuropathy after cutting. Post-traumatic or axonal neuropathy develops as a result of damage to nerve endings that arise from certain structures of the spinal cord and are responsible for transmitting nerve impulses to the limbs. If nerve transmission is difficult or completely interrupted, the patient complains of tingling or complete loss of mobility. Distal axonal neuropathy manifests itself differently depending on the nature, type and location of the pathological process.
- Ischemic neuropathy develops when nerve endings are compressed in the area of the musculoskeletal joints and in the spinal column. A violation of not only innervation, but also blood circulation is recorded, which leads to the formation of ischemia. With a chronic course of the process and a long-term disorder, paresthesia and hypotrophic processes develop, which in severe cases can lead to paralysis and necrosis . Ischemic neuropathy has a wide range of symptoms and is not difficult to diagnose.
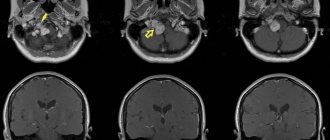
- The best known form is optic neuropathy. Anterior ischemic optic neuropathy . Characterized by damage to the anterior segment of the optic nerve, which leads to very rapid and persistent impairment of visual function, up to complete or partial atrophy of the optic nerve. Anterior optic neuropathy is also known as vascular pseudopanillia . Posterior ischemic optic neuropathy. It is characterized by damage to the retrobulbar posterior part of the optic nerve due to ischemic effects. The posterior form is also fraught with loss of visual perception.
- Ulnar nerve neuropathy. The peripheral nervous system can be affected by several causes. Damage to the ulnar nerve is most often encountered in traumatology. As a result of compression of the nerve trunk, which is located in the area of the elbow joint, the entire upper limb is affected.
- Radial nerve neuropathy. Clinically, it manifests itself as a characteristic symptom of a “dangling hand,” which is caused by the inability to straighten the hand and fingers. Damage to the radial nerve can be associated with trauma, metabolic processes, ischemia, and compression.
- Median nerve neuropathy. The nervus medianus can be affected in any area, which will inevitably lead to swelling and severe pain in the hand area and impaired sensitivity. The process of flexion of all fingers and opposition of the thumb is disrupted.
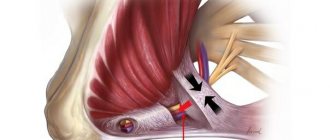
- Pudendal nerve neuropathy. It develops as a result of damage to the pudendal nerve, which is located in the pelvic area. Takes an active part in the act of urination and bowel movement, sending nerve impulses along the nerve trunks that pass through the genitals. Pathology is characterized by severe pain.
- Neuropathy of the tibial nerve. The clinical picture depends on the level of nerve damage. The tibial nerve is responsible for the innervation of the muscles of the foot and lower leg and the sensitivity of the skin in this area. The most common cause of tibial nerve neuropathy is traumatic injury to the nerve trunk.
- Femoral nerve neuropathy. The clinical picture of damage to the femoral nerve depends on the level of damage to the large nerve trunk.
- Neuropathy of the oculomotor nerve. Diagnosis of pathology requires a thorough examination and is complex. The clinical picture is represented by symptoms that occur in many diseases. When the oculomotor nerve is damaged, ptosis, divergent strabismus, etc. are observed.
Cause of occurrence
In most cases, acute oxygen starvation up to anoxia leads to destructive processes in the myelin sheath, disrupting tissue metabolism. Often, this occurs for the following reasons:
- injuries;
- compression;
- vascular pathology;
- infections;
- toxins.
Peroneal nerve neuropathy occurs after injury to the knee, ankle, fibula, or lower leg. These can range from minor bruises to severe dislocations or fractures.
Compression occurs due to compression of the fiber by musculoskeletal structures. Often the compression form of the pathology occurs in people whose work activity requires prolonged squatting. For example, paving slab or parquet layers, berry and vegetable pickers, and others. In this position of the body, compression and disruption of trophism occurs. Another name for compression neuropathy is “tunnel syndrome.”
With vascular pathologies, a lack of oxygen and nutrients depletes the tissues of the lower limb.
Infections and toxins destroy the myelin sheath and tissue.
Reference . In some cases, damage occurs during surgery unrelated to neuritis. This complication is one of the most common when performing operations on the knee joint, lower leg and ankle.
Causes
It is extremely rare that neuropathy develops as a separate independent disease. Most often, nerve endings are affected against the background of a chronic pathology, which acts as a traumatic factor. The development of neuropathy is preceded by the following diseases and conditions:
- hypovitaminosis;
- metabolic disorder ;
- decreased reactivity;
- intoxication , poisoning;
- nerve fiber injury;
- neoplasms (malignant and benign);
- severe hypothermia;
- hereditary pathology;
- diagnosed endocrine diseases.
Causes of inflammation
Neuritis can occur for the following reasons:
- Nerve damage – limb injuries, nerve compression by colloid cords after surgery.
- Nerve compression - tunnel syndrome - prolonged stay in a position that is uncomfortable for the lower extremities, often occurs as a result of professional activity.
- Vascular pathologies and other blood supply disorders - this leads to tissue hypoxia, therefore, metabolic processes are disrupted.
- Toxic lesions - diabetic, kidney.
- Infectious lesions - one of the branches of the nerve fiber is involved in the inflammation process.
- Neuropathy of compression-ischemic etiology develops against the background of the presence of neoplasms - as the tumor increases in size and metastasizes.
Athletes are susceptible to neuropathy, especially runners , people who, due to their professional activities, are forced to lift heavy objects and injure their lower extremities.
It also affects overweight people - in this case, the load on the foot increases significantly, which leads to deformation or damage to the nerve fiber.
Women who wear high-heeled shoes for a long time , especially those with extra pounds and in old age, also risk the development of neuritis. Often the pathology occurs in people who walk barefoot or in shoes without heels at all - with thin soles.
Symptoms of neuropathy
When nerve endings are damaged, muscle fibers become thinner and their reflex function is impaired. In parallel, there is a decrease in contractility and partial loss of sensitivity to stimuli that cause pain.
The clinical picture of neuropathy can be very different, and the pathological process can be localized anywhere, causing neuropathy of the peroneal nerve, trigeminal nerve, facial nerve, ulnar and radial nerve. Damage to sensory, motor or autonomic nerve function negatively affects the patient's quality of life. Several forms of neuropathy occur in patients with diabetes
- Peripheral neuropathy. Characterized by damage to the peripheral nerves that are responsible for the innervation of the upper and lower extremities. Symptoms of neuropathy of the upper extremities manifest themselves in the form of impaired sensitivity in the fingers and toes, a tingling sensation, and a feeling of numbness in the upper extremities. The symptoms of neuropathy of the lower extremities are identical: tingling and sensory disturbances in the lower extremities are noted.
- Proximal form. It is characterized by impaired sensitivity mainly in the lower extremities (buttocks, thigh, lower leg).
- Autonomous form. There is a functional disorder of the genitourinary system and digestive tract organs.
Symptoms of alcoholic neuropathy
Most often, alcoholic neuropathy is accompanied not only by sensory disorders, but also by motor ones. In some cases, patients complain of muscle pain of various locations. The pain syndrome may be accompanied by a sensation of “crawling” in the form of paresthesia, tingling, a feeling of numbness and impaired motor activity.
At the initial stage, patients complain of muscle weakness and paresthesia. In every second patient, the disease first affects the lower extremities, and then the upper ones. There are also simultaneous lesions of the upper and lower belts.
Characteristic symptoms of alcoholic neuropathy:
- a sharp decrease, and in the future a complete absence of tendon reflexes;
- diffuse decrease in muscle tone.
Alcoholic neuropathy is characterized by disruption of the facial muscles, and in more advanced cases, urinary retention is noted. In the advanced stage, alcoholic polyneuropathy is characterized by:
- muscle weakness in the limbs: unilateral or symmetrical;
- paresis and paralysis;
- violation of surface sensitivity;
- sharp inhibition of tendon reflexes followed by their complete extinction.
Symptoms
Clinical manifestations of peroneal neuropathy are determined by the type and location of the lesion. Acute nerve injury is accompanied by a sharp, almost immediate appearance of symptoms of its damage. Chronic injury, dysmetabolic and compression-ischemic disorders are characterized by a gradual increase in the clinical picture. Damage to the common trunk of the peroneal nerve is manifested by a disorder in the extension of the foot and its toes. As a result, the foot hangs down in a plantarflexed position and is slightly internally rotated. Because of this, when walking, moving the leg forward, the patient is forced to bend it strongly at the knee joint so as not to catch the toe on the floor. When lowering the leg to the floor, the patient first stands on his toes, then rests on the lateral plantar edge, and then lowers the heel. This gait resembles that of a rooster or a horse and has corresponding names. Difficult or impossible: raising the lateral edge of the sole, standing on the heels and walking on them. Motor disturbances are combined with sensory disorders extending to the anterolateral surface of the lower leg and dorsum of the foot. There may be pain on the outer surface of the lower leg and foot, which increases with squats. Over time, atrophy of the muscles of the anterolateral region of the leg occurs, which is clearly visible when compared with a healthy leg. Neuropathy of the peroneal nerve with damage to the deep branch is manifested by less pronounced foot drop, reduced extension strength of the foot and toes, sensory disorders on the dorsum of the foot and in the 1st interdigital space. The long course of neuropathy is accompanied by atrophy of small muscles on the dorsum of the foot, which is manifested by retraction of the interosseous spaces.
Tests and diagnostics
Neuropathy is considered a rather difficult disease to diagnose, which is why it is so important to correctly and thoroughly collect anamnesis. The difficulty lies in the long-term absence of certain symptoms. The doctor will have to find out: whether medications were taken, whether viral diseases were suffered, or whether there was contact with certain chemicals.
The onset of the disease can occur against the background of alcohol abuse. The diagnosis is pieced together based on many factors. Neuropathy can occur in different ways: progressing over several days or years, and even lightning fast.
Using palpation, the doctor examines the nerve trunks, identifying pain and thickening along their course. A Tinnel test is required . This method is based on tapping the nerve ending and identifying tingling in the zone of sensitive innervation.
A laboratory blood test is performed to determine ESR, and sugar levels are measured. Additionally, an X-ray examination of the chest . Electrophoresis of whey proteins is also performed .
Diagnostics
A neurologist can make a diagnosis based on the collected history, complaints and symptoms, and the results of instrumental and laboratory examinations. The following examination methods are often used:
- electromyography;
- electroneurography;
- Ultrasound.
Also, the doctor must conduct a series of tests using a special needle to determine the preservation of reflexes, the level of sensitivity reduction, the speed of impulse transmission, and others.
A patient with trauma is additionally given x-rays of bones and joints.
Treatment
Therapy for non-inflammatory damage to nerve endings is individual in nature and requires not only an integrated approach, but also regular prevention.
Treatment methods are selected depending on the form, degree and causes that contributed to the damage to neuromuscular conduction. All therapy is aimed at fully restoring nerve conduction. In case of toxic damage to the nervous system, detoxification measures are carried out (elimination of influencing factors, administration of an antidote ).
Treatment of diabetic neuropathy
In diabetic cases, measures to maintain normal blood sugar levels are recommended. At the same time, it is recommended to get rid of bad habits. Metabolic disorders in diabetes mellitus contribute to an increase in the level of free radicals circulating in the bloodstream, with impaired antioxidant activity of one’s own organs and systems. All this leads to disruption of the integrity of the inner lining of the vessel and nerve fiber.
For diabetic neuropathy, the use of medications based on alpha-lipoic acid is indicated:
- Thiogamma;
- Berlition;
- Espa-Lipon.
The traditional neurological set involves the introduction vitamins for the complete restoration of neuromuscular conduction. It is not recommended to resort to treatment with folk remedies.
Forecast and prevention of occurrence
The prognosis of the pathology depends on how soon the patient sought help from a specialist and how correct the treatment was. Irreversible changes significantly worsen the prognosis and lead to disability.
To prevent the occurrence of neuritis, it is recommended:
- maintain optimal body weight;
- protect your feet from injury;
- periodically give your legs a break during prolonged vertical or uncomfortable body positions;
- wear comfortable shoes with orthopedic insoles;
- do not wear high-heeled shoes on a regular basis;
- people involved in sports need to be regularly screened for compression-ischemic neuropathy (tunnel syndrome).
It is strictly not recommended to delay treatment of the pathology at the first symptoms , as this can aggravate the situation and lead to irreversible consequences. Ignoring the symptoms of pathology leads to incapacity and permanent disability.
Medicines
Treatment of lower extremity neuropathy includes the following medications:
- Neuroprotectors or metabolic accelerators in nerve cells. Drugs for treatment: Mildronate ; Piracetam .
- Anticholinesterase medications , the action of which is aimed at optimizing the sensory functioning of nerve endings. The drugs improve neuromuscular conduction of the lower extremities. These include: Prozerin ; Ipidacrine .
- Antioxidants. Prevent negative consequences from the influence of free radicals on the functioning of the nervous system. A high concentration of free radicals has a destructive effect on the tissues of the peripheral nervous system. Preparations: Cytoflavin ; Mexidol .
- Alpha lipoic acid. The drugs help restore neurocytes and speed up metabolism. High effectiveness is observed in diabetic neuropathy.
- Other medications. The use of B vitamins has a good effect; in particular, B1 , B6 , B12 . Vitamin complexes help restore neuromuscular conduction. There are tablet and injection forms: Milgamma ; Neuromultivitis ; Combilipen .
Self-treatment at home is not recommended.
Treatment of neuropathic pain in adults
Neuropathic pain - what is it?
Neuropathic pain occurs when the transmission of impulse signals along the nerves is disrupted. In adults, neuropathic pain syndrome is described as stabbing, burning, shooting and is often associated with electric shock.
Therapy begins with the simplest painkillers ( Ibuprofen, Ketonal ). If they are ineffective and the pain syndrome is severe, antidepressants and antiepileptic drugs (for example, Tebantin ) are prescribed.
Tricyclic antidepressants
Drugs in this group are often used to relieve neuropathic pain. It is believed that the mechanism of their action is based on preventing the transmission of nerve impulses. The most commonly prescribed medication is Amitriptyline . The effect may occur within a few days, but in some cases, pain therapy is extended for 2-3 weeks. The maximum effect of therapy is recorded at 4-6 weeks of intensive treatment. A side effect of therapy is drowsiness , which is why treatment begins with the smallest doses, gradually increasing the dosage for better tolerability. Drinking plenty of fluids is recommended.
Anticonvulsants, antiepileptic drugs
If it is impossible to use antidepressants, anti-epileptic drugs ( Pregabalin, Gabapentin ) are prescribed. In addition to the treatment of epilepsy, medications are excellent for relieving neuropathic pain syndrome. Treatment begins with the smallest doses, identical to antidepressant therapy.
POLYNEUROPATHIES AND OTHER LESIONS OF THE PERIPHERAL NERVOUS SYSTEM (G60-G64)
Excludes: neuralgia NOS ( M79.2 ) neuritis NOS ( M79.2 ) peripheral neuritis during pregnancy ( O26.8 ) radiculitis NOS ( M54.1 )
G60 Hereditary and idiopathic neuropathy
G60.0 Hereditary motor and sensory neuropathy Disease: • Charcot-Marie-Toots • Dejerine-Sotta Hereditary motor and sensory neuropathy, types I-IY. Hypertrophic neuropathy in children Peroneal muscular atrophy (axonal type) (heper trophic type). Roussy-Levi syndrome G60.1 Refsum's disease G60.2 Neuropathy in combination with hereditary ataxia G60.3 Idiopathic progressive neuropathy G60.8 Other hereditary and idiopathic neuropathies. Morvan's disease. Nelaton's syndrome Sensory neuropathy: • dominant inheritance • recessive inheritance G60.9 Hereditary and idiopathic neuropathy, unspecified
G61 Inflammatory polyneuropathy
G61.0 Guillain-Barre syndrome. Acute (post-)infectious polyneuritis G61.1 Serum neuropathy. If it is necessary to identify the cause, use an additional code of external causes (class XX). G61.8 Other inflammatory polyneuropathies G61.9 Inflammatory polyneuropathy, unspecified
G62 Other polyneuropathies
G62.0 Drug-induced polyneuropathy If necessary, identify the drug, use an additional code for external causes (class XX). G62.1 Alcoholic polyneuropathy G62.2 Polyneuropathy caused by other toxic substances If it is necessary to identify a toxic substance, use an additional code for external causes (class XX). G62.8 Other specified polyneuropathies. Radiation polyneuropathy If necessary, identify the cause, use an additional code for external causes (class XX). G62.9 Polyneuropathy, unspecified. Neuropathy NOS
G63* Polyneuropathy in diseases classified elsewhere
G63.0 * Polyneuropathy in infectious and parasitic diseases classified in other headings Polyneuropathy in: • diphtheria ( A36.8 +) • infectious mononucleosis ( B27 . -+) • leprosy ( A30 . -+) • Lyme disease ( A69.2 +) • mumps ( B26.8 +) • herpes zoster ( B02.2 +) • late syphilis ( A52.1 +) • congenital syphilis ( A50.4 +) • tuberculosis ( A17.8 +) G63.1 * Polyneuropathy in neoplasms ( C00 - D48 +) G63.2 * Diabetic polyneuropathy ( E10 - E14 + with a common fourth sign .4) G63.3 * Polyneuropathy in other endocrine diseases and metabolic disorders ( E00 - E07 +, E15 - E16 +, E20 - E34 +, E70 - E89 +) G63.4 * Polyneuropathy with malnutrition ( E40 - E64 +) G63.5 * Polyneuropathy with systemic connective tissue lesions ( M30 - M35 +) G63.6 * Polyneuropathy with other bone diseases -muscle lesions ( M00 - M25 +, M40 - M96 +) G63.8 * Polyneuropathy in other diseases classified in other headings. Uremic neuropathy ( N18.8 +)
G64 Other disorders of the peripheral nervous system
Peripheral nervous system disorder NOS
Procedures and operations
In addition to drug therapy, neuropathy of the peroneal nerve also includes physiotherapeutic procedures:
- Magnetotherapy. It is based on the effect of a magnetic field on the human body, which helps relieve pain, restore nerve cells, and reduce the severity of the inflammatory reaction.
- Amplipulse. It is based on the effect of modulated current on the affected area, due to which nerve cells are restored and swelling is reduced. Has an anti-inflammatory effect.
- Electrophoresis with drugs . It is based on the influence of an electric field, due to which medications enter the site of inflammation.
- Ultrasound therapy. When exposed to ultrasound, blood circulation is stimulated and the severity of pain is reduced. Has a tonic and anti-inflammatory effect.
- Electrical stimulation. Restoration of neuromuscular conduction occurs under the influence of electric current.
Radial nerve neuropathy is treated in the same way. A course massage is also recommended to restore the radial nerve.
What do you need to remember?
- Peroneal nerve neuropathy is a lesion of the nerve tissue in any of its areas.
- Most often, pathology occurs due to injury and compression of the nerve.
- The main manifestations are impaired expansion of the foot and fingers, impaired sensitivity of the anterior surface of the lower leg.
- The diagnosis is established after a thorough examination of the patient and a series of neurological tests.
- Complex treatment with drug therapy, physical therapy, exercise therapy and surgical correction allows you to completely restore the functioning of the affected structure.
- Often, the disease can be completely eliminated.
Literature
- Averochkin A.I., Shtulman D.R. Tunnel neuropathies // Journal. neuropathol. and psychiatrist, named after. S.S. Korsakov. -1991. No. 4. — P.3-6.
- Akimov G.A., Odinak M.M. Differential diagnosis of nervous diseases: A guide for doctors. St. Petersburg: Hippocrates, 2000. - 664 p.
- Voznesenskaya T.G. Pain syndromes in neurological practice //ed. AM V;yn. M.: Medpress, 2001. - 368 p.
- Flores LP, Koerbel A., Tatagiba M. Peroneal nerve compression resulting from fibular head osteophyte-like lesions. Surg Neurol 2005; 64(3):249-52.
- Perkins AT, Morgenlander JC Endocrinologic causes of peripheral neuropathy. Pins and needles in a stocking-and-glove pattern and other symptoms. Postgrad Med 1997;102(3):81-2, 90-2, 102-6.
Source
Prevention
Preventive measures include timely treatment of infectious and systemic diseases, normalization of general metabolism. It is important to understand that pathology can become chronic, which is why timely and competent treatment is so important.
In case of a mild course of the disease and a chronic form of neuropathy, sanatorium-resort treatment is indicated, where the following is carried out:
- aromatherapy;
- laser and light treatment;
- magnetic therapy;
- massage, exercise therapy;
- acupuncture;
- psychotherapy.
Consequences and complications
There are many complications from peripheral neuropathy and they depend primarily on the causative factor that led to damage to the nerve trunk. Main complications:
- Diabetic foot. It is considered one of the most terrible complications of diabetes.
- Gangrene . The cause of the putrefactive process is the complete lack of blood flow in the affected area. The pathology requires emergency surgical treatment: excision of necrotic areas, amputation of a limb.
- Autonomic cardiovascular neuropathy. It is characterized by disturbances in various autonomic nervous functions, including sweating, bladder control, heart rate, and blood pressure .