Home>Articles>Dangerous consequences of simultaneous use of antidepressants and alcohol
quick menu (hide)
- Functioning of antidepressant drugs
- Alcohol while taking antidepressants
- SSRIs-antidepressants and alcohol
- Tricyclic antidepressants
- MAO inhibitors
- Alcohol with herbal antidepressants
- Antidepressants and alcohol: consequences of joint use
- Antidepressants and alcohol after completing a course of medication
Antidepressants and alcoholic drinks are incompatible things. If there is alcohol in the blood, the risk of side effects of antidepressants increases, which especially concerns the central nervous system. Let's look at why this happens.
What is the basis for the functioning of antidepressant drugs?
Basically, antidepressants are taken with the aim of increasing in the body the degree of production of hormones responsible for a favorable emotional background, normal mood, and an active mood.
After completing a course of taking such drugs, the patient begins to become interested in life, events and the people around him. The thoughts that his life is aimless and meaningless disappear.
The effect of taking such medications can be felt 14 days after starting to take the drugs, not earlier. The shortest duration of treatment is 3-4 months.
If the patient also has an alcohol addiction, then for the sake of his health and mental state he must give up alcohol for the entire duration of the course. Otherwise, dangerous side effects may occur, the effects of which will be enhanced by drinking alcohol.
Literature:
- A short reference book on psychopharmacology, pharmacotherapy and mental pathology / Kozlovsky, Vladimir Leonidovich.. - St. Petersburg: SpetsLit, 2015.
- Belikov Readings: materials of the VIII All-Russian Scientific and Practical Conference / Pyatigorsk Medical and Pharmaceutical Institute - branch of the Volga State Medical University of the Ministry of Health of Russia, Pyatigorsk. - Pyatigorsk: RIA-KMV, 2021. - 835 p.
- Delinquency of “Pharmacy drug addiction” as a determining factor in strengthening control over the circulation of medicines / Vladimir Ilyich Zhukovsky, Natalya Vladimirovna Dovgolyuk / 2021 / Humanitarian and legal research.
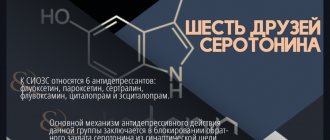
SSRI antidepressants and alcohol: consequences
Serotonin is a signaling substance. Brain cells exchange serotonin molecules to transmit information. If a person is depressed, then he has an imbalance of serotonin.
SSRI antidepressants stabilize the patient's mood, easing the course of depression.
SSRI drugs contain the following active ingredients:
- Fluoxetine;
- Sertraline;
- Paroxetine;
- Citalopram;
- Escitalopram;
- Fluvoxamine;
- Venlafaxine;
- Duloxetine.
Alcoholic drinks should not be combined with selective serotonin reuptake inhibitors, as they increase the side effects of taking antidepressant medications. Also, such combinations can cause depressive psychosis, sexual disorders, and the appearance of hallucinations.
Difficult blood clotting, a sudden decrease or increase in blood pressure, and arrhythmia are possible. Secretory functions may deteriorate.
Complex autonomic disorders may appear.
Consequences
Alcoholic drinks inhibit regulatory centers and suppress natural reactions. The medicine is designed to improve performance. The products act through the monoamine system, which regulates mood and vigor.
Frequent drinking of alcohol increases their production, and the drug tries to restore the emotional background. As a result, the varied effects of alcohol and medication confuse the brain.
Tranquilizers negatively affect the liver. Ethanol puts a double burden on this organ. With the parallel use of alcohol and the drug, a hypertensive crisis may develop, which is often fatal.
The most dangerous consequence can be considered depression of the respiratory system, which leads to respiratory arrest followed by death.
Other side effects of treatment interrupted by alcohol consumption:
- Autonomic disorders, manifested by high blood pressure, arrhythmia, and problems with blood clotting.
- Hallucinations.
- Psychoses.
- Sexual disorders.
- Worsening depression because alcohol reduces the effect of the medication.
- The reaction decreases, the thought process worsens.
- Lethargy.
- Stroke due to increased blood pressure.
Alcohol enhances the absorption of the chemical components of the antidepressant, which is why the improvement occurs faster, but the effect is short-lived. After an emotional and psychological uplift, the patient’s condition sharply worsens, he experiences a stronger feeling of depression.
Often, patients drive their bodies to alcohol dependence when drinking alcohol during treatment.
A decrease in concentration is dangerous when it comes to professions and activities that require special attention. The hypnotic effect is dangerous when driving a car or working on complex machines.
Tricyclic antidepressants
The structure of these drugs is similar: 3 connected ring-shaped molecules. This list includes drugs that contain the following active ingredients:
- Amitriptyline;
- Clomipramine;
- Imipramine;
- Tianeptine;
- Pipofezin.
Such drugs have increased toxicity, so drinking alcohol while taking them is prohibited. Tricyclics have many serious side effects, and the presence of alcohol in the blood increases the risk of their occurrence or enhances their effects.
Tricyclic drugs are not compatible with alcohol, other medications, or certain foods.
Possible adverse reactions include the following.
- Problems with the functioning of the digestive tract (constipation, urinary retention). State of drowsiness, rapid heartbeat. Confusion of thoughts and consciousness may be recorded.
- A person gains excess weight and his blood pressure drops.
- Loss of appetite, feeling of nausea.
- Ejaculation and erection become worse.
- Convulsive attacks occur.
- Psychopathological symptoms worsen.
- Hypotension is observed.
results
During the prescribed 56-day course of treatment with Velaxin, 31 (96.9%) people were recognized as responders, of which a “minor” effect of treatment was observed in 1 (3.1%) patient, a “moderate” effect in 3 (9.4 %), “good” - in 2 (6.25%), and 25 (78.1%) patients showed a “significant” therapeutic effect. Thus, a decrease in the intensity of depressive disorders by 50% or more during treatment with Velaxin was found in the vast majority of cases - in 27 (84.4%) patients, as shown in Fig. 1.
Rice. 1. The degree of severity of the therapeutic effect of Velaxin for endogenous depression. The x-axis is the degree of reduction according to HAM-D,%; The y-axis is % of patients.
In general, the effectiveness of Velaxin, assessed on the 56th day of therapy, was quite high: the average total score of depression severity according to HAM-D was reduced by 85.9%. By the end of the 1st week of treatment with Velaxin, a positive therapeutic response to the drug was observed: the reduction in depression was at the level of a “minor” effect, but was approaching a 20% reduction in disorders, bordering on a “moderate” improvement. A clear “moderate” improvement (reduction in HAM-D score by 33.2%) was observed by the 14th day of treatment; between the 21st and 28th days of treatment, the therapeutic effect reached the “good” range with a decrease in HAM-D scores by 50% or more, and by the 6th week the effect of Velaxin treatment was already approaching the “significant” border (up to 76.7% reduction in the severity of depressive symptoms). In the subsequent 7-8 weeks of therapy, an undeniable “significant” improvement in the patients’ condition was detected (reduction of disorders by more than 80%), up to “recovery” (Fig. 2). In 20 out of 31 patients (64.5% of cases) who completed the course of treatment with Velaxin, depression was completely reduced and “entry” into remission was observed (their total HAM-D score became 6 or lower).
Rice. 2. The spectrum of therapeutic action of velaxin for endogenous depression (HAM-D score). Here and in Figs 3, 4 and 5 (in the last one - the right axis): on the ordinate - the average score as a percentage of the score before the start of therapy, on the x-axis - the day of therapy.
The severity of the condition, assessed by the CGI-S subscale, on average decreased during treatment with Velaxin from 4.7 to 1.6 points at the end of the study (from “significantly expressed” to less than “mildly expressed”, i.e., to the virtual absence of distress ). Moreover, a noticeable decrease in the severity of symptoms was noted in the period between the 7th and 21st days of treatment, when the intensity of the manifestations of depression consistently decreased on average to “moderately” and “weakly” expressed. From the 5th week of therapy, the severity of depressive disorders became “very weak”, and at the 7-8th week of course therapy there was a practical “exit” from depression with the “absence” of depressive symptoms (their average level of severity was 1.6 points). During the 56-day course of therapy, assessment of the degree of improvement in the depressive state on the CGI-I subscale showed a “deterioration” of the mental state (5th assessment level) in only 1 (3.1%) person, remained “unchanged” (4th assessment level) also in 1 (3.1%) patient, “minor improvement” (3rd level) - also in 1 (3.1%), “pronounced” improvement (2nd level) was observed in 4 (12 .6%), the remaining 25 (78.1%) patients showed a “significant” improvement (grade 1).
It was found that in the spectrum of antidepressant action of Velaxin, all 3 components of its psychotropic activity, in accordance with the final results of treatment, are presented to almost the same extent with a slight advantage in terms of anti-depressive action (see Fig. 2). Thus, the degree of reduction in the average total score of disorders on items 1-3 and 22-24 of HAM-D (reflecting the actual thymoleptic effect of the drug) was 88.2%, on items 7 and 8 (stimulating effect) - 83.7%, and on points 9 and 10 (anti-anxiety effect) - 85.1%. However, the implementation of all 3 components of the action of Velaxin over time was different and had its own characteristics. Thus, thymoleptic and especially anxiolytic effects were detected most quickly during treatment. They developed almost in parallel, reaching a level of reduction in the severity of disorders according to HAM-D by 32.8 and 37.1%, respectively, by the 14th day of therapy (“moderate” effect). At the same time, the stimulating effect of Velaxin was somewhat “lagged” compared to the anti-anxiety and anti-sadness effects, reaching similar values (“moderate” effect - reduction of disorders by 36.9%) only by the 21st day of the study.
Subsequently, in the period from the 21st to the 28th days of treatment, the thymoleptic and anti-anxiety components of the action in the spectrum of antidepressant activity of Velaxin leveled off and increased in rate of development to the range of a clear “good” effect (score reduction by 60.2 and 59. 2%). But already from the 5th week of treatment, the thymoleptic effect itself began to surpass the anxiolytic one in terms of the depth of reduction of disorders according to the corresponding HAM-D items: the thymoleptic effect appeared at the “significant” level already at the 6th week, and the anti-anxiety effect only after the 7th week course therapy. The formation of the stimulating effect was “lagged” in the degree of manifestation compared to the other two components of the action of Velaxin at 1 week, and its “significant” severity was determined only at the 8th week of treatment. And only at this stage of treatment, as already mentioned, the depth of the stimulating effect of Velaxin approximately coincided with the severity of the thymoleptic and anxiolytic effects.
In accordance with established data on the peculiarities of the implementation of individual components of antidepressant action in the spectrum of psychotropic activity of velaxin, its therapeutic effectiveness was analyzed depending on the syndromic type of depression, i.e., on the dominant affect that determines the picture of the depressive state (Fig. 3). It was found that with leading anxious affect, the reduction in the average total score on HAM-D was 85.5% by the 56th day of treatment; with a predominance of apatho-adynamic affect, the effectiveness of Velaxin was similar - the average total score on HAM-D decreased by 85.9%. The highest effectiveness of Velaxin was observed in the treatment of patients with a leading sad affect in the picture of depression - the reduction in the average total score on HAM-D was 91.1%. But with a relatively similar degree of reduction in depressive symptoms, differences were also noted in the dynamics of the implementation of the antidepressant effect of the drug. Thus, with leading anxious and melancholy affects, i.e. in patients with positive affectivity and the most typical manifestations of depression, the reduction of depressive symptoms proceeded at an equal pace, reaching 21.1% (with anxious depression) and 22.5% (with melancholy depression) already by the 7th day of therapy. Subsequently, the decrease in the average total score on HAM-D occurred more intensively and reached more than 50% reduction in depressive symptoms by the 28th day of treatment. When treating patients with negative affectivity (atypical apatho-adynamic depression) with Velaxin, improvement occurred more slowly. A reduction in the average total HAM-D score by 20% or more (“moderate” effect) occurred only in the 2-3rd week of therapy; and only by the 4th week a “good” effect of Velaxin was recorded (reduction of disorders by 61.3%). By the 7-8th week of treatment, the improvement in the condition was already “significant” (more than 80% reduction in disorders), it coincided in severity with the therapeutic effect of Velaxin for anxious depression and was somewhat “lag behind” the effect for melancholy depression.
Rice. 3. Dynamics of the effectiveness of Velaxin for different types of endogenous depression (HAM-D score).
Analysis of the effectiveness of Velaxin depending on the nosological affiliation of depression also revealed some features (Fig. 4): the lowest rate of decrease in the average total score on HAM-D by the end of the course of treatment was in patients with low-progressive schizophrenia, it was equal to 82.3%. These same patients also had the slowest rate of reduction in depressive disorders - by the 7th day it was only 15.2%, and a reduction of 50% or more (the limit of a “good” effect) was achieved only by the 28th day; A “significant” effect was detected in patients with low-progressive schizophrenia only after the 7th week of treatment with Velaxin. In patients with affective illness (MDP, cyclothymia), the reduction in the average total score on HAM-D at the end of course therapy was close in value (86.6%), and the rate of reduction in depressive symptoms was similar: by the 7th day this figure reached 18 .2%, and by the 4th week of therapy it was already 59.4% (“good” effect). The best treatment result was achieved in patients with postpsychotic depression and paroxysmal schizophrenia - 90.4% reduction in disorders on the 56th day of treatment. Despite the fact that by the end of the 1st week of the study, the rate of reduction in depressive symptoms reached gradations of “insignificant” improvement (19.2%), subsequently the reduction in depressive symptoms occurred more intensively than with MDP, demonstrating a “good” effect already at 14 days. 1st day of treatment (symptom reduction rate -53.9%), and by the 28th day it was already 76.5%, i.e. it was almost on the border of “significant”. However, it should be noted that in these patients the initial severity of depressive disorders was significantly lower, at the level of “moderate” severity, than in other, more “severe” depressions (23 points on HAM-D versus 31.3 points for affective illness and 31.6 for low-progressive schizophrenia).
Rice. 4. Antidepressant effect of Velaxin in different nosological groups of patients (HAM-D score).
All of the indicated patterns of development of the therapeutic effect of Velaxin indicate the absence of a direct dependence on the size of its daily dose. As can be seen from Fig. 5, the therapeutic effect began to appear and increase from the 3-4th week of treatment (reduction of depressive symptoms by 50% or more according to HAM-D), with an increase in the average daily dose to the maximum (182.1-198.2 mg per day) . But subsequently, despite stabilization and even a slight decrease in the achieved maximum average daily dose of Velaxin (up to 190.3 mg per day), the response to therapy continued to increase at a faster pace, to the level of “significant” improvement,
Rice. 5. The relationship between the therapeutic effect (HAM-D score) and the daily dose of Velaxin. On the left ordinate is the average daily dose of the drug (mg).
During the course of Velaxin therapy, 45 adverse events of various types were registered in 21 (65.6%) patients; in 5 they were single, and in 16 they were combined. The most common were mental and autonomic adverse events noted on the UKU scale; they occurred in 40% of patients. One patient withdrew from the study early (after 2 weeks of treatment) due to the development of acute affective-delusional psychosis, requiring a change in therapy. Neurological and other side effects occurred in only 8.9 and 11.1% of patients. The most common individual side effects observed were “excitement/anxiety” (in 15.5% of patients), decreased sleep duration and nausea (in 11.1%), tachycardia and hyperhidrosis (in 6.6%), sedation and constipation (in 4.4%). All other side effects occurred in isolated cases. The incidence of side effects during a course of treatment with Velaxin was highest in the 2nd week of treatment, when the average daily dose of the drug was insignificant (157.7 mg per day). The most common adverse events during this period were psychiatric and autonomic adverse events. But subsequently, despite increasing the average daily dose, the incidence of side effects gradually decreased. The exception was “other” side effects, the frequency of which practically remained at the same level until the end of treatment. These were mainly sexual dysfunctions, which developed according to an increase in the daily dose of Velaxin.
It should be noted that, in general, all adverse events were mild or approaching moderate severity in the first 2 weeks of treatment, and then their average severity as assessed by UKU decreased to a “mild” level, despite a gradual increase in the average daily doses of Velaxin. At the same time, mental side effects were initially the most severe: the average UKU severity score at 1–2 weeks of treatment was 1.9–2.0. However, during the further course of treatment, the severity of adverse mental symptoms decreased from the 3rd week. The severity of some other adverse events increased slightly compared to the initial one: if on the 2nd week of treatment their severity on average corresponded to the UKU “mild” degree (1 point), then later they reached 1.5 points, and at the same time their degree severity increased according to an increase in the average dose of Velaxin.
MAO inhibitors
MAO inhibitors are active substances that slow down the enzyme monoamine oxidase. These drugs include those that contain the following active ingredients: pirlindole and moclobemide.
When taking these inhibitors, you should not drink alcohol, otherwise serotonin and tyramine syndromes may occur. Taking antidepressants and alcohol lead to depression of the respiratory center and is therefore life-threatening. It is necessary to carefully follow the diet, as there are many drugs and foods that are incompatible with MAO inhibitors.
Possible adverse reactions include:
- accelerated production of adrenaline and increase in its level;
- neutralizing the effects of an antidepressant drug when drinking alcohol;
- hypertensive attacks;
- more frequent heartbeat.
When taking MAO inhibitors, non-alcoholic beer is also prohibited. Beer contains a lot of tyramine, a substance that increases adrenaline levels. When combined with an antidepressant drug, this can lead to terrifying consequences for a person.
It is forbidden to drink even half a glass of dry wine.
What antidepressants can alcohol be combined with?
As the safest option, experts consider the combined use of strong drinks and antidepressant drugs created using ademetionine or the herb St. John's wort. To avoid negative reactions, doses of alcohol should be small. During the week, you are allowed to take alcohol once in doses that are not capable of provoking the development of a hangover syndrome. The maximum permissible portion of a strong drink (cognac, vodka) is 1 glass.
Antidepressants that can be treated with alcohol include:
- Heptor.
- Heptral.
- Deprim.
- Negrustin
- Life 600.
The listed products contain ademetionine or St. John's wort. Despite their relative neutrality regarding alcohol, it is important not to exceed the recommended doses of strong drinks. In addition, you should take breaks between drinking alcohol (at least 1 week).
Important information. If, in addition to the listed drugs, other types of antidepressants are taken, you will need to completely eliminate even small doses of alcohol.
Tricyclic antidepressants and alcohol - compatibility
Tricyclic antidepressants are drugs created on the basis of:
- amitriptyline;
- imipramine;
- pipofezin;
- clomipramine;
- tianeptine.
These components are included in Elivel, Clominal, Coaxil, Azafen, Melipramin, Anafranil and other antidepressant products.
Patients often ask whether alcohol can be consumed while taking tricyclic antidepressants. These drugs are not considered highly toxic, and yet their combined use with alcohol is a strict taboo. Violation of such a prohibition can result in the development of severe side effects.
Tricyclic antidepressant medications also exhibit negative interactions with certain medications and foods, requiring increased caution during their use.
Is it possible to drink alcohol with herbal antidepressants?
Mild herbal antidepressant drugs are known to have a mild calming effect. If a specialist has prescribed a person to take a course with such drugs, then drinking alcoholic beverages in this situation is not prohibited. However, you need to drink it in small doses to avoid a hangover.
The minimum break between drinking alcohol should be 7 days.
Thus, you must carefully read the instructions for the medications prescribed by your doctor. If “Antidepressant” is indicated in the “Pharmacological group” section, this means that drinking alcohol is prohibited during the period.
Antidepressants and alcohol: consequences of joint use
There is a popular belief that alcohol is an affordable and effective “antidepressant”, which is also sold without a prescription. But in reality, the euphoria felt after drinking alcohol passes very quickly.
At first, the person's mood improves, but soon he feels increased irritability, and then becomes aggressive. After sobering up occurs, problematic, tormenting situations that led to a depressive state come flooding back.
Often people try to drink alcoholic beverages every day in order to feel tolerable.
The consequences of this situation include the formation of a persistent dependence on alcohol, as well as the complete ineffectiveness of taking antidepressant medications.
Antidepressants and alcohol, which are not compatible, as confirmed by experts, make the treatment of depression useless. A person develops serious health problems that become impossible to control.
When mixing antidepressant drugs and alcohol, negative health consequences arise - the appearance of pathologies in the brain and internal organs. Adverse consequences include:
- vegetative-vascular dystonia;
- arterial hypertension;
- cirrhosis of the liver;
- increased depression.
Antidepressants and alcohol after completing a course of medication
Often, addiction to alcohol is a prerequisite for the onset of depression. Treatment can only be carried out when the body has been cleansed of ethyl alcohol and its metabolic products. For this purpose, a strong detoxification is carried out, during which enterosorbents are used and detoxification agents are administered intravenously.
Testing will help determine whether alcohol has been completely eliminated from the patient’s body. If the result is positive, then the person is prescribed treatment for depression with appropriate medications.
When the course of medication has come to an end or there is an objective need to stop taking it, then starting to drink alcohol is allowed only 14 days after the treatment course has completed. Otherwise, a person will experience serious disorders of both the nervous system and all internal organs.
According to patients who have undergone full treatment for depression, it is necessary to get rid of alcohol addiction in order to have a chance to live a healthier and happier life.
Features of the pharmacological effects of Zoloft
Sertraline is a serotonin reuptake blocker produced by enteroendocrine cells of the epithelium of the gastrointestinal tract and the median nuclei of the brain stem. The hormone produced in the gastrointestinal tract activates a number of important physiological functions - gastrointestinal motility, uterine contractions, vasoconstriction, platelet aggregation and much more.
A neurotransmitter synthesized by the central nervous system is responsible for regulating mood, normalizing sleep-wake cycles, attention, appetite, sexual behavior and aggression. Activates the state of passion and inhibits pain impulses.
The anti-anxiety drug works by increasing and accumulating the level of the “happiness hormone”. Due to its balanced effect, when used in therapeutic doses, it does not have a stimulating or sedative effect, does not cause dependence or withdrawal symptoms.
But, not belonging to the class of narcotic substances, Zoloft causes an effect similar to taking drugs that increase the production of serotonin - amphetamine and its analogues. This became the reason for the unauthorized use of the drug.
An increased dosage, combination with other antidepressants or ethanol produces a prolonged effect and excessive accumulation of the hormone, causing symptoms of excess. Serotonic syndrome is a dangerous condition accompanied by impaired autonomic functions, changes in mental background and neuromuscular excitation, causing irreversible health problems.