Varieties
Sensitivity disorders are divided into two groups - increased or decreased.
Reduced ones include analgesia, hypoesthesia, and termanesthesia. With analgesia, a person does not feel pain; it can occur in many diseases and injuries of the nervous system. Hypoesthesia is manifested by a decrease in tactile sensitivity; the patient does not respond to skin punctures or insects crawling on the body. Thermaneesthesia is characterized by a violation of the perception of temperature conditions (warm and cold influences).
Increased sensitivity distinguishes terms such as hyperalgesia, hyperesthesia and hyperpathia. Hyperalgesia is a pathologically increased perception of pain; sharp or increased perception of stimuli is called hyperpathy. In this condition, the unpleasant sensations continue for quite a long time, the patient cannot determine the exact location and the sensations of irritation continue longer than contact with the irritant occurs. Hyperesthesia is an increased perception of stimuli, but at the same time the patient is able to sense the correct location of the stimulus and what type of impact.
Disorders in which the patient perceives a single effect as multiple are called polyesthesia. Allocheiria is a condition in which the patient feels irritation not at the site of its impact, but in the same areas on the opposite side of the body. With dysesthesia, there is a perverted perception of stimuli, that is, their confusion. When exposed to pain, the patient may feel warmth; when exposed to low temperatures, a tingling sensation. Paresthesia is a spontaneously occurring and short-term sensation of numbness, burning and a feeling of “crawling sensations”.
Publications in the media
Sensory disturbances can occur with both central and peripheral damage to the nervous system. Terminology • Dermatome - zone of innervation of the skin from one dorsal ganglion and the corresponding segment of the spinal cord • Anesthesia - lack of sensitivity (tactile, temperature, pain, etc.) •• Dissociated - absence of pain and temperature sensitivity while maintaining proprioceptive or vice versa •• Hysterical - anesthesia in patients with hysteria, characterized by the absence of organic damage to receptors, pathways and centers of the nervous system and usually spreading to areas of the body, the boundaries of which do not correspond to the zones of innervation of certain roots or nerves •• Root - anesthesia in the zone of innervation of a certain dorsal root of the spinal cord •• Partial - absence of one or more types of sensitivity while maintaining the others •• Segmental - dissociated or total anesthesia in the zone of innervation of a certain segment of the spinal cord •• Total - absence of all types of sensitivity •• Traumatic - anesthesia resulting from damage to sensory nerves and (or) nervous centers systems • Hypoesthesia - decreased superficial sensitivity • Hyperesthesia - increased sensitivity • Hypalgesia - decreased pain sensitivity •
Hyperalgesia - increased pain sensitivity • Paresthesia - a spontaneously occurring unpleasant sensation of numbness, tingling, burning, crawling, etc. • Dysesthesia - a perversion of sensitivity (for example, heat is perceived as pain or cold) • Numbness - an unusual sensation consisting in deterioration of skin perception (sensitivity) • Hyperpathia - a perversion of sensitivity, characterized by an increase in the threshold of perception, the lack of precise localization of sensations of an unpleasant nature, inclination to irradiation, long aftereffect; occurs when mixed and sensory nerves are incompletely interrupted, when they are restored after transection, when the thalamus or posterior columns of the spinal cord are damaged • Polyesthesia is a disorder of superficial sensitivity, in which irritation of one point is perceived as irritation of many points • Allocheiria is a sensitivity disorder in which applied to certain areas of the limb, irritation is felt in a symmetrical area of the opposite limb • Synesthesia - the occurrence of irritation of a sense organ along with adequate other sensations (for example, the sensation of color when listening to music) • Batianesthesia - lack of proprioceptive sensitivity.
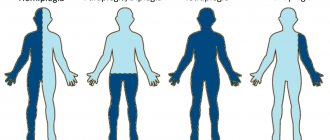
Etiology • Areas of hypoesthesia in all extremities in a sock-and-glove pattern are characteristic of polyneuropathy • Involvement of one limb or one side of the body suggests a central lesion • Involvement of individual nerves (multiple mononeuropathy) • Involvement of nerve roots (radiculopathy) • Involvement of the spinal cord (sensory impairment below a certain level level) • Damage to the brain (hemihypesthesia) • Hyperpathy occurs when the mixed and sensory nerves are incompletely interrupted, when they are restored after transection, when the thalamus or posterior columns of the spinal cord are damaged • Dissociated anesthesia indicates damage to the area of the brain where conductors of different modalities pass separately. It is especially typical for lesions of the posterior horns, the anterior commissure of the spinal cord and for lesions in the brain stem. Clinical picture
• Types of sensory disorders •• Peripheral •• Segmental - impaired sensitivity in the zone of segmental innervation •• Conductive - impaired sensitivity throughout below the level of the lesion •• Cortical - local loss of sensitivity; determined by damage to a certain area of the cortex.
• There are symptoms of irritation , loss and distortion of the function of sensory conductors •• The most common sign of irritation of sensory neurons is pain ••• Types of pain: local (local) - occurs in the area of irritation; projection - with irritation of the nerve trunk; is projected into the skin area innervated by this nerve; irradiating - occurs in the zone of innervation of one of the branches of the nerve when irritation is applied in the zone of innervation of another branch of the same nerve; reflected - for diseases of internal organs, localized in the Zakharyin-Heda zones; causalgia (see Causalgia syndrome); phantom - observed after amputation of limbs ••• Pain sensations can be sharp, dull, cutting, stabbing, etc. •••
When nerve roots that carry out predominantly somatic innervation are damaged, somatalgia occurs, localized in the zone of branching of the spinal roots or peripheral nerves. Paroxysmal or constant in nature ••• When fibers of the predominantly sympathetic nervous system are damaged, sympathalgia (vegetalgia) develops. The pain is diffuse, deep, pressing, burning, constant or paroxysmal. Often accompanied by spasm of peripheral vessels, impaired sweating, trophic disorders ••• Hyperalgesia •• Symptoms of loss - loss of sensitivity (any type of superficial and deep): anesthesia, hypesthesia, analgesia, hypalgesia •• Perversion of sensitivity - hyperpathia.
• Qualitative disorders of surface sensitivity : polyesthesia, allocheiria, synesthesia, dysesthesia, bathyanesthesia. Sensitivity testing • Pain sensitivity - using a pin, examine symmetrical areas of the skin. If a difference is detected, temperature sensitivity is checked in the same areas using test tubes with warm and cold water • Articular-muscular feeling - passive movements of the terminal phalanges of the fingers and toes up or down with the patient's eyes closed. If the patient finds it difficult to accurately indicate in which joint the doctor makes passive movements, it is necessary to examine more proximal joints • Vibration sensitivity - checked using a tuning fork with a frequency of 64 or 128 Hz •
The tactile sense is determined using a piece of cotton • If sensitivity disorders are detected, it is necessary to establish the anatomical localization of the lesions, i.e. make a topical diagnosis.
Diagnostics • An important criterion for diagnosis is the coincidence of motor and sensory disorders, changes in reflexes • X-ray of the spine • CT, MRI • Lumbar puncture • Electromyography.
ICD-10 • F44.6 Dissociative anesthesia or loss of sensory perception • G46.6* Purely sensitive lacunar syndrome (I60-I67+) • R20 Impaired skin sensitivity • R43 Impaired sense of smell and taste • R94.1 Abnormalities identified during testing functional studies of the peripheral nervous system and individual sensory organs
Treatment of sensitivity disorders
Therapy depends on the disease that caused the pathology. For example, if the diagnosis reveals osteochondrosis, at the Professor Gorbakov Clinic in Krasnogorsk they prescribe:
- medications - anti-inflammatory drugs, decongestants and angioprotectors;
- manual therapy, massage and other local treatments;
- physiotherapy – “magnets”, UVT, laser;
- exercise therapy;
- acupuncture, vacuum therapy.
If a disorder of skin sensitivity occurs due to a hernia or protrusion, chondroprotectors are prescribed to strengthen the tissues of the intervertebral discs.
The choice of physiotherapeutic methods in the clinic is also carried out depending on the underlying cause. For example, for diabetes mellitus, electrophoresis of nicotinic acid and zinc in the iliac region is indicated, and for multiple sclerosis, magnetic laser irradiation, cryotherapy and massage are indicated. Very often, doctors recommend treating skin sensitivity disorders by supplementing the diet with vitamin B12 and folic acid, the deficiency of which causes the syndrome.
Types of Numbness
Depending on the disease that provoked the syndrome, numbness can affect different parts of the body:
- If the cause is a pathology of the brain, the loss of sensitivity will affect the limbs on the opposite side. So, if the right hemisphere is damaged, the left leg or arm will suffer.
- With diseases of the spinal cord, numbness occurs in the area located below.
- Polyneuropathy provokes the “gloves and socks” syndrome.
- If the culprit is a peripheral nerve, the person will feel a loss of sensitivity in a finger - for example, the little toe on the foot, or the big toe - in the area of innervation.
Dictionary
Sensitivity disorders are often observed in various diseases of the nervous system and, as a rule, are used to clarify the tonic diagnosis, as well as to monitor the dynamics of the pathological process under the influence of the patient’s treatment. There are quantitative and qualitative disturbances of sensitivity. Quantitative ones are a decrease in the intensity of sensation - hypoesthesia or complete loss of sensitivity - anesthesia. This applies to all types of sensitivity: hypalgesia, analgesia - decrease or absence of pain sensitivity, thermohypesthesia, thermoanesthesia - decrease or absence of temperature sensitivity, topohypesthesia, topanesthesia - decrease or loss of the ability to localize irritations, etc. Increased sensitivity - hyperesthesia is associated with a decrease in the threshold for the perception of or other irritation. Qualitative disturbances of sensitivity include distortion of the perception of external stimuli, for example: the occurrence of a sensation of pain during cold or heat stimulation - thermalgia, a feeling of a larger size of the palpated object - macroesthesia, the sensation of many objects instead of one - polyesthesia, a sensation of pain in a different area in relation to the injection site - synalgia, a feeling of irritation not in the place of its application - alloesthesia, a feeling of irritation in a symmetrical area on the other side - allocheiria, inadequate perception of various irritations - dysesthesia. Hyperpathy is a special form of qualitative change in sensitivity - a kind of painful perception of various sharp irritations. With hyperpathy, the threshold of excitability increases (mild irritations are perceived in the hyperpathic zone less clearly than normal, and intense irritations are sharply painful, extremely unpleasant, painful), irritations are poorly localized by the patient, and their aftereffect is long-lasting. Sensory disorders include paresthesia - a variety of sensations not associated with any external influence - goosebumps, numbness, tingling, stiffening of skin areas, pain in the roots of the hair (trichalgia), a feeling of moisture in the skin, movement of drops of liquid on it (hygroparesthesia). Especially often, various paresthesias are observed with tabes dorsalis, funicular myelosis and other diseases of the nervous system, in which the posterior cords of the spinal cord and dorsal roots are involved in the process. Symptoms of irritation of sensitive conductors include pain, incl. in amputated limbs and with causalgia often combined with the symptom of hygromania (craving for wet things). Sanatorium-resort treatment is recommended for sensory disorders in sanatoriums with a medical profile: treatment of diseases of the nervous system.
Clinical diagnostics in neurology
1.8. Basic provisions of the theory of pain mechanisms according to R. Melzack
Canadian scientists R. Melzack and P. D. Wall in 1965 proposed the theory of control of afferent flow at the input, or the theory of the entrance gate. Its essence boils down to the fact that pain afferentation comes from receptors along myelinated and unmyelinated fibers to the sensitive cells of the spinal cord (V Rexed plate). These fibers give off collaterals to the cells of the posterior gelatinous substance (substancia gelatinosa)
, located in plates II – III. The posterior gelatinous substance (gelatinous substance of Roland) is secreted as part of the posterior horn and, like a crescent, is adjacent to its posterior end. The gelatinous substance is most powerfully developed in the region of the trigeminal nerve nuclei and the upper cervical region. In the caudal direction, it is present along the entire length of the dorsal horns of the spinal cord. Its quantity increases according to the levels of origin of roots and nerve endings.
The pain and temperature sensitivity fibers of the dorsal roots in the dorsal horns end not only at the own nuclei of the dorsal horns, but also in the gelatinous substance. In this case, impulses from myelinated fibers activate neurons of the Roland substance, while impulses from unmyelinated fibers inhibit their activity. The gelatinous substance, closely associated with the sensitive cells of the dorsal horn of the spinal cord, is an inhibitory system in relation to them. In this regard, excitation of Roland's substance has a presynaptic inhibitory effect on the axon terminals of the first sensory neurons or a postsynaptic inhibitory effect on spinal sensory cells, as a result of which the flow of pain impulses into the overlying parts of the nervous system decreases - the pain gates close. When the gelatinous substance is inhibited, the opposite effect occurs: the transmission of nociceptive excitation is facilitated - the gates to pain open.
Thus, under the influence of impulses from the overlying structures (central gray periaqueductal substance, raphe nuclei, caudate and red nuclei, paragiant cell nucleus of the reticular formation, paraventricular and anterior parts of the hypothalamus, some nuclei of the thalamus and cerebral cortex), passing along thick myelin fibers, gelatinous the substance actively functions and inhibits the transmission of impulses coming from the periphery, i.e., “closes the gate.” At the same time, a limited number of selected signals is received in the higher departments, but sufficient to carry out the necessary information. Under the influence of impulses carried through small-diameter fibers (unmyelinated), the functioning of the Roland substance is inhibited; it loses control over the flow of afferent signals, which, significantly exceeding the necessary information flow, rushes through “transfer” points to the overlying sensory centers.
In 1998, R. Melzack proposed a new – neuromatrix – theory of pain. The author believes that there is a physical and a phantom body. The physical body is experienced through sensory stimulation from the periphery. The phantom body can exist in the absence of peripheral impulses. The feeling of one's own body is genetically programmed and occurs in the neuronal circuits of the central nervous system (in the limbic system). The sensation of pain is produced by a pattern of nerve impulses generated by the neuromatrix (under the influence of sensory impulses or independently, in accordance with the genetic program).
1.9. Peripheral variant of sensitivity disorders
A variant of sensitivity disorder is understood as a set of sensory disorders of a certain type and their localization when the sensory pathway is damaged at various levels. It is customary to distinguish the following types of sensory disorders: peripheral, spinal, cerebral and functional.
Rice. 1.3.
Distribution of skin sensitivity according to peripheral nerves (according to P. Duus)
The listed options, with the exception of the functional one, can, in turn, be divided by localization into several types, and some types (for example, the conduction cerebral type) into subtypes.
The peripheral variant is characterized by sensitivity disorders that occur when sensory pathways within the peripheral nervous system are damaged (peripheral nerves, plexuses, roots) (Fig. 1.3).
Types of Peripheral Sensory Disorders
1. Neural type of sensitivity disorders.
Occurs when sensory or mixed nerves (its main trunk or sensory branches) are damaged. Sensory disorders in neuritis (inflammatory processes) and neuropathies - non-inflammatory lesions (compression-ischemic, traumatic, toxic, etc. - see Chapter 11) do not fundamentally differ in the topical localization of sensory disorders and are characterized by the following main features:
– sensitivity disorders may have the nature of symptoms of irritation (pain, paresthesia, hyperpathia, pain in the nerve trunk during palpation, positive symptoms of tension, pain at the nerve exit points) and (or) symptoms of loss (anesthesia, hypoesthesia, etc.);
– symptoms of prolapse and irritation are most pronounced in the zone of autonomous innervation. Symptoms of irritation often predominate. It should be taken into account that in some pain syndromes (for example, at the repercussion stage of causalgia), pain can also occur outside the zone of innervation of the affected nerve;
– for pain due to nerve irritation, a special character is typical: shooting, burning, “tearing”, caused or intensified by palpation or tension of the nerve, they are accompanied by pronounced vegetative-trophic disorders. Such pain in combination with other symptoms of irritation without symptoms of prolapse determine the clinical picture of neuralgia, and the presence of symptoms of prolapse (in combination with or without symptoms of irritation) already suggests neuritis (neuropathy).
– the pathological process leading to the neural type of sensory disorders may be limited to one or involve several nerves (mono-, multi-, multiple neuritis or neuropathies - see subsection 2.16).
The main causes of neuralgia are irritation of the nerve due to its partial compression, which is most often caused by tunnel syndrome - compression of the affected nerve in the bone or fibrous canal (trigeminal neuralgia, etc.), as well as other local pathological processes (tumors, metastases, hematomas, adhesions and etc.).
The development of neuropathies with predominantly sensory disorders is observed with a concussion of the nerve (neuropraxia), as well as with some tunnel neuropathies and reflex-dystrophic syndromes (causalgia). In other forms of the above pathology of mixed nerves, sensory disorders are also observed, but they are usually combined with the neural type of movement disorders or are significantly inferior to the latter in severity.
2. Polyneuritic type of sensitivity disorders.
It occurs as a result of inflammatory (polyneuritis) or non-inflammatory (polyneuropathy) damage to predominantly distal parts of the peripheral nerves. Sensitivity disorders are characterized by the following symptoms:
– localization predominantly in the distal parts of the extremities like “gloves” and (or) “socks”, symmetry, lack of a clear boundary of sensory disorders;
– among sensory disorders, symptoms of irritation may be observed - pain, paresthesia, hyperesthesia, hyperpathia, pain in the nerve trunks during palpation and tension and (or) symptoms of loss - hypoesthesia, anesthesia;
– symptoms of loss and (or) irritation affect, as a rule, all types of sensitivity, although their severity may vary depending on the nature of the pathological process and the stage of the disease;
– specific symptoms are often identified that arise as a result of deep sensitivity disorders: in the legs – sensitive ataxia, in the arms – pseudoathetosis and (or) false astereognosis;
– the above-described sensitivity disorders are often combined with vegetative-trophic disorders of predominantly distal localization.
The presence and nature of sensory disorders, as well as their severity, are determined primarily by the etiological factors of polyneuritis or polyneuropathy. Polyneuritis with a purely sensory variant of the polyneuritic syndrome is significantly more common only in tuberculosis, early neurosyphilis, and typhus. Polyneuropathies with predominantly sensory disorders include: alcoholic, diabetic, as well as polyneuropathies due to folic acid deficiency, endocrine diseases (hypothyroidism, pituitary pathology), drug intoxication (isoniazid, PAS, etc.), tumors of internal organs. Acute inflammatory demyelinating polyradiculoneuropathy Guillain-Barré may begin with polyneuritic sensory disorders, although motor polyneuritic disorders subsequently develop and predominate.
3. Radicular type of sensitivity disorders.
This type of peripheral variant is characterized by a violation of all types of sensitivity and radicular pain in the form of stripes, which are transverse on the body and longitudinal on the limbs (Fig. 1.4).
Rice. 1.4.
Segmental innervation of the skin (according to Hansen-Schliack)
They can occur with pathology of the dorsal root, the Babinsky-Nageotte radicular nerve (part of the root from the dura mater to the spinal ganglion), the spinal ganglion, the spinal cord of Sicard
(formed as a result of the fusion of the motor and sensory roots). The etiological factors of their damage are varied: infectious-toxic, infectious-allergic, compression-ischemic, traumatic, toxic, dysmetabolic, hereditary (see subsection 11.4).
Among them, the dominant one in frequency is the pathology of the spinal cord of a non-inflammatory nature (funiculopathy), which in the domestic literature is traditionally referred to as radiculitis. The clinical picture of radicular syndrome is characterized by the following symptoms:
– radicular sensitivity disorders, radicular pain and paresthesia in the area of the corresponding dermatome;
– symptoms of root tension in combination with reactive pain;
– muscular-tonic syndromes;
– local pain in the area where the roots exit the intervertebral foramina (Vallée’s point);
– a combination of radicular sensory and radicular motor disorders of varying severity;
– when the spinal ganglion is involved in the pathological process (herpetic ganglionitis), the above clinical symptoms characteristic of the radicular type of sensitivity disorders are supplemented by herpetic rashes.
When establishing the nosology of the radicular type of sensory disorders, it should be borne in mind that in most cases various vertebrogenic pathologies can lead to its development:
– vertebrogenic pathology, predominantly of a degenerative-dystrophic nature (the main ones are pathology of the intervertebral discs, spondylosis deformans, spondyloarthrosis, ligamentosis ossificans, narrow spinal canal syndrome);
– inflammatory lesions of the vertebral bodies (purulent spondylitis, tuberculous, brucellosis, fungal, etc.);
– tumors of the vertebral bodies (primary benign and malignant, metastatic tumors, myeloma);
– developmental anomalies of the spine ( spina bifida
, additional cervical vertebra, anomalies of the craniovertebral junction, etc.);
– spinal dysplasia (fibrous dysplasia, Scheuermann-Mau disease, Paget disease, achondroplasia, spondyloepiphyseal dysplasia);
– endocrine-metabolic osteodystrophy (more often with hyperparathyroidism, hypothyroidism, diabetes mellitus);
– traumatic lesions of the spine (soft tissue bruise, sprain, rupture of ligaments, fractures of bodies, arches, processes, traumatic hernias).
In contrast to radicular syndromes of the lumbosacral and cervical regions, thoracic radicular syndromes are extremely rarely the result of degenerative processes in the thoracic spine. The development of radicular thoracalgia is usually associated with inflammatory (spondylitis), systemic (Bechterew's disease) and metastatic lesions. It should also be taken into account that radicular pain at the cervical and thoracic level may be of a reflected nature due to pathology of the thoracic or abdominal organs.
1.10. Spinal variant of sensitivity disorders
The spinal variant of sensitivity disorders may be caused by damage to the dorsal horn and sensory pathways in the spinal cord (segmental and conductive types, respectively).
1. Segmental spinal type.
Occurs when the posterior horn of the spinal cord and the anterior white commissure are damaged. When the dorsal horn is damaged, it is manifested by disorders of only pain and temperature sensitivity in the zone of the corresponding dermatomes, which are localized similar to the incoming root (radicular-segmental zones of sensory disorders) with the preservation of deep and largely tactile sensitivity - a dissociated disorder of surface sensitivity in the corresponding segments. Paresthesia is not typical. There are no motor disorders. The segmental type of sensitivity disorders usually has upper and lower levels (boundaries). Dull and aching retrocorn pain predominates. A segmental variant of sensory disorders caused by damage to the dorsal horn is observed in syringomyelia and syringomyelitic syndrome of other etiologies (see subsection 3.6). In cases of damage to the anterior white commissure, sensitivity disorders are dissociated and symmetrical (“butterfly”).
2. Conductive spinal type with damage to the lateral and posterior cords
. Caused by damage to the lateral spinothalamic tract in the lateral cords, the thin fasciculus (Gaulle) and the sphenoid fasciculus (Burdach) in the posterior cords. With a transverse lesion of the spinal cord, the conduction type is characterized by a violation of deep sensitivity from the level of the lesion on its side, a violation of superficial sensitivity two segments below the lesion on the side contralateral to the lesion. Occurs with spinal strokes, injuries and tumors of the spinal cord, demyelinating diseases, isolated lesions of the posterior cords (neurosyphilis, funicular myelosis, Friedreich's ataxia, Roussy-Lewy disease, atypical forms of neural amyotrophy with predominant deep sensitivity disorders, etc.).
3. Conductive spinal type with damage to the anterior white commissure
. Clinically it differs from the segmental type in the symmetry (on both sides) of dissociated sensory disorders.
Sensory disorders are the most important component of spinal cord lesion syndromes: Brown-Séquard syndrome, complete transverse spinal cord lesion syndrome, etc. (see Chapter 3).
1.11. Cerebral variant of sensitivity disorders
May occur with damage to the sensory nuclei of the cranial nerves (nuclear type), cerebral structures, conduction pathways of general sensitivity at various levels (medulla oblongata, pons, midbrain, thalamus optic, internal capsule, corona radiata) and the cerebral cortex - respectively, conduction cerebral and cortical types. A common feature of conduction cerebral sensitivity disorders is that they are localized on the side of the body opposite to the lesion (hemianesthesia, sometimes alternating).
1. Damage to the pathways of general sensitivity in the brain stem below the thalamus optica.
It is characterized primarily by the occurrence of alternating syndromes: on the affected side, a defect of a certain cranial nerve (nerves) is detected, and on the opposite side - isolated disorders of all types of sensitivity of the conduction type (hemianesthesia or hemihyposthesia) or in combination with other hemidisorders: pyramidal, cerebellar, etc. .
2. Damage to the optic thalamus.
In this case, conduction sensory disorders are usually included in the “three hemi” syndrome: hemianesthesia, hemiataxia, hemianopsia. Often, when the optic thalamus is damaged, peculiar thalamic pain occurs in the opposite half of the body - hemialgia. They are perceived as a painful feeling of cold or burning, are difficult to describe to the patient and are poorly localized.
3. Damage to the internal capsule.
Sensory disorders arise due to damage to the fibers of the third sensory neurons in the posterior third of the posterior thigh of the internal capsule. They are characterized by hemianesthesia or deep hemihyposthesia of all types of sensitivity on the side of the body contralateral to the lesion, without a convincing difference in their severity in the arm and leg. Sensory disorders are usually included in the “three hemis” syndrome: hemianesthesia, hemiplegia, hemianopsia.
4. Defeat of the radiant crown.
It is characterized by sensory disorders that are more limited in extent, affecting predominantly the upper (brachiofacial localization) or lower limb. With extensive damage to the corona radiata, sensory disorders can be combined with hemiparesis and are characterized, in contrast to capsular, by uneven distribution in the arm or leg, up to monoparesis and monohyposthesia of the limb.
5. Damage to the cortex.
Cortical sensitivity disorders can be caused by damage to the posterior central gyrus and parietopostcentral regions, as well as the superior parietal lobule.
Damage to the posterior central gyrus and parietopostcentral regions may result in symptoms of prolapse and/or irritation.
Symptoms of hair loss
. The localization of sensory disorders corresponds to the somatotopic localization of the pathological focus (half of the face, arm, leg), and their severity is greatest in the distal parts of the arm or leg - pseudopolyneuritic type in the form of one “glove” or “sock”. Mostly deep and complex types of sensitivity suffer. A number of specific symptoms are possible: afferent paresis, afferent (kinesthetic) apraxia, oral apraxia, afferent motor aphasia, false astereognosis.
Symptoms of irritation
usually manifest as paresthesia, localized or spreading over half the body (without “march” and with “march”, respectively - a sensitive version of Jacksonian epilepsy).
Damage to the superior parietal lobule. With symptoms of prolapse, sensitivity is upset over the entire half of the body without asymmetry in the arm or leg, true astereognosis is characteristic in one or both arms, and afferent paresis is often noted. Symptoms of irritation in the form of paresthesias occur simultaneously on the entire half of the body (hemiparesthesia); they can also manifest as adversive seizures due to damage to the posterior adversive field.
1.12. Functional variant of sensitivity disorders
The distribution of sensitive disorders does not correspond to any of the organic types and is determined by the patient’s personal ideas about the nature of sensitive disorders. Signs of functional sensitivity disorders:
– the boundaries of sensitive disorders vary from study to study;
– usually patients, when presenting hemianesthesia, indicate its boundaries strictly along the midline. With an organic lesion on the body, this cannot happen, since the border of sensory disorders in this case is always shifted towards the latter;
– if you conduct a sensitivity study in the initial state, and then shift the fold of abdominal skin to the side, i.e., artificially make a new midline, then the patient in both cases will complain about sensitivity disorders in the midline (with an organic lesion, the border of the disorders will shift together with skin);
– sensitivity disorders are often distributed according to an anatomical principle (up to the elbow or axillary fold, etc.).
The functional variant of sensitive disorders can occur in people with neuroses, psychopathy, and endogenous mental illnesses.