The type of stroke - an acute circulatory disorder in a particular area of the brain, is determined by the immediate cause that caused it - hemorrhage in the medulla or blockage of a cerebral artery with a thrombus or embolus. There are two types of strokes, and knowing their differences is necessary to choose the right treatment strategy.
Neurologists at the Yusupov Hospital use modern neuroimaging methods, ultrasound, laboratory and instrumental diagnostic methods, which allow timely diagnosis, determination of the type of stroke and the degree of brain dysfunction.
Depending on the cause underlying the occurrence of acute cerebrovascular accident, the following types are distinguished:
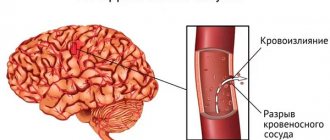
- Hemorrhagic. This form of the disease develops as a result of rupture of a blood vessel, which is accompanied by the leakage of blood into the thickness of the medulla (cerebral hemorrhage) or under the meninges (subarachnoid hemorrhage);
- Ischemic (cerebral infarction). The development of the disease is based on a complete or partial disruption of blood flow through a cerebral artery, caused by its blockage by an embolus (embolic stroke) or thrombus (thrombotic stroke). It occurs several times more often than hemorrhagic.
The division of stroke into hemorrhagic and ischemic is quite arbitrary, since with any form of the disease, both hemorrhagic and ischemic foci simultaneously appear in the patient’s brain tissue. Therefore, it is more correct to talk about a predominantly hemorrhagic or predominantly ischemic cerebral stroke, but for convenience, shorter designations have been adopted.
Causes and risk factors
Ischemic and hemorrhagic types of brain damage are characterized by different causes of the development of the disease.
The main cause of ischemic stroke is cerebral atherosclerosis. Patients often suffer from other diseases that develop against the background of atherosclerosis (angina pectoris, myocardial infarction).
Causes of different types of cerebral infarction:
- Atherothrombotic occurs as a result of thrombosis of large and medium arteries. The development of ischemic atherothrombotic stroke is stepwise, occurs within a day, attacks often begin in sleep;
- Cardioembolic develops as a result of complete or partial embolism (blockage) of an artery. The onset is sudden during wakefulness, accompanied by severe neurological symptoms. Often develops into hemorrhagic stroke (ischemic stroke with hemorrhagic transformation);
- Hemodynamic is caused by a decrease in blood pressure, a drop in cardiac output (myocardial ischemia, bradycardia);
- Lacunar develops against the background of hypertension as a result of damage to small perforating (extending from the main arteries) vessels. Symptoms increase gradually. It is distinguished by the absence of general cerebral symptoms and the severity of focal symptoms in accordance with the localization of ischemia (paralysis, loss of vision, speech impairment);
- Rheological or hemorheological microocclusion. The cause of the disease is not vascular occlusion (blockage), but a change in blood viscosity due to impaired hemostasis. Accompanied by scant neurological symptoms;
The causes of hemorrhagic stroke can be primary (defect in the development of vascular walls, decreased elasticity and strength) and secondary.
The primary causes of cerebral hemorrhage include rupture of an aneurysm. Secondary ones include grade 2 and 3 hypertension and embolism (complete blockage of an artery by a blood clot).
Risk factors:
- Heredity (hemophilia);
- Constant stress, chronic fatigue (leads to vascular spasms and the development of ischemia);
- Overweight;
- Diabetes;
- Heart disease (arrhythmia);
- Lipid metabolism disorders, atherosclerosis (threatens embolism);
- Bad habits (alcohol, smoking).
Postoperative management of elderly patients
After the operation is completed, the postoperative period begins. It is divided into near and distant. The immediate period begins immediately after surgery and continues until discharge from the hospital. Remote begins from the moment of discharge until the patient is no longer bothered by general and local disorders.
In elderly patients, the functioning of the respiratory and cardiovascular systems is reduced. In addition, their body cannot, due to age, resist infections. Reparative processes during the healing of postoperative wounds are also deteriorated. These factors make the recovery period more difficult.
Age negatively affects the vital capacity of the lungs, reducing their maximum ventilation and disrupting the drainage function of the bronchial tree. The result is often pneumonia. During rehabilitation, breathing exercises, massage, and bronchodilators are used.
Almost all older people suffer from atherosclerosis and cardiosclerosis. There is a tendency to hypercoagulation - increased blood clotting, which leads to the formation of blood clots
It is important to thin the blood and activate patients. Physical activity reduces the risk of blood clots
Gastric and acid-enzymatic functions of the gastrointestinal tract are reduced, so high-calorie foods that are easily digested are prescribed. In older people, purulent complications develop, so you need to carefully monitor wounds.
From the editor: How does migraine in children manifest, detect and treat?
Precursors of the development of cerebral infarction
Hemorrhagic stroke occurs suddenly. There are clear general cerebral and focal symptoms:
- Loss of sensitivity, paralysis of individual muscle groups;
- Severe nausea with spasmodic vomiting;
- Strong headache;
- Loss of consciousness, convulsions, coma.
Precursors of cerebral ischemia are mild general cerebral symptoms:
- Deterioration of hearing, “congestion in the ears”;
- Violation of the psycho-emotional state (overexcitation or inhibition);
- Darkening of the eyes, fainting.
Headache does not always accompany ischemic infarction.
Symptoms of hemorrhagic and ischemic stroke
The clinical picture of any stroke includes general cerebral and focal neurological symptoms. The symptoms are very diverse and depend on the part of the brain in which the disaster occurred.
General cerebral symptoms:
- Drowsiness, drowsiness or agitation, disturbance or loss of consciousness;
- Pain in the eyeballs, aggravated by eye movement;
- Headache;
- Nausea;
- Autonomic disorders: vomiting; increased sweating, dry mouth, feeling hot, irregular heart rhythm, breathing;
- Memory loss.
Focal symptoms:
- Hemiplegia (inability to perform voluntary movements) or paralysis on the opposite side relative to the localization of the lesion;
- Hemiparesis (partial weakening) of muscles. The patient has a smile, weakened muscle tone of one half of the body;
- Aphasia (speech impairment), sensory aphasia (lack of understanding of speech) are caused by localization of the lesion in the left temporal lobe of the brain;
- Dysarthria (blurred speech). The cause may be either localization of ischemia in the left temporal lobe or paralysis of the facial muscles;
- Diplopia, double image, complete or partial blindness;
- Hearing loss;
- Dizziness, gait disturbance, difficulty swallowing, hiccups;
Clinical picture of ischemic stroke:
- Transient (temporary) ischemic attacks. The attacks are characterized by small focal disturbances. They disappear completely within 24 hours;
- Small stroke (micro-stroke). Prolonged ischemic attacks with complete restoration of brain function in the period from 2 days to 3 weeks;
- Progressive ischemic stroke. With this form, symptoms increase over 2-3 days. Subsequently, the victim’s neurological functions are not fully restored;
- Completed ischemic stroke. A cerebral infarction zone is formed, as a result of which neurological symptoms remain stable or are only partially restored.
Hemorrhagic stroke develops very quickly and the first harbinger of an upcoming brain catastrophe is a headache, a feeling of fullness in the head, vomiting, and impaired consciousness. After a few minutes, paresis and loss of consciousness may occur. The time during which medical workers can provide assistance and prevent the death of a patient is very short and ranges from 3 minutes to several hours.
Hemorrhagic and ischemic stroke have fairly similar symptoms. The difference between them is that with the hemorrhagic form of the disease, the symptoms are more pronounced and the patient’s condition is assessed more seriously.
Make an appointment
First aid and treatment
An ambulance should be called immediately at the first suspicion. Until she arrives, you will need to provide assistance yourself:
- lay the victim down and raise his head;
- make sure that his clothing does not restrict breathing;
- make sure that your tongue does not sink;
- do not give anything to drink or eat;
- ventilate the room;
- cool your head with compresses;
- when vomiting, make sure that he does not suffocate; his head should be turned to the side;
- If necessary, perform chest compressions or artificial respiration.
Please note: no medications should be used without consulting a doctor; in this condition, taking them can be extremely dangerous.
There are several stages in the treatment of stroke:
- first aid;
- hospital treatment;
- rehabilitation.
It is very important to provide first aid correctly, because it is the first hours of a stroke that are most often decisive: if time is lost, death is very likely. If everything went well, then intensive therapy is carried out in the hospital, with the help of which they try to ensure that the brain is damaged as little as possible, and also to prevent a recurrent stroke.
Gradually, the intensity of therapy decreases, but it continues for several weeks and sometimes months - the patient’s health must be carefully monitored during this time.
Diagnostics
Experienced neurologists at the Yusupov Hospital determine the localization of the pathological process thanks to a well-collected medical history, specific symptoms, and the results of additional studies.
To diagnose a stroke and determine the type of cerebrovascular accident, our doctors use modern diagnostic equipment. The knowledge and experience of doctors allows for quick differential diagnosis and prescribing effective treatment.
Diagnostics is supplemented by:
- Clinical and biochemical analysis of blood and urine;
- Cardiogram, electroencephalogram;
- Angiography of cerebral vessels;
- Computed tomography;
- MRI;
- Ultrasound examination;
- Examination by specialized specialists (otolaryngologist, ophthalmologist, therapist, endocrinologist).
Any course of acute cerebrovascular accident, regardless of the type of stroke, is always a life-threatening condition for the patient. It is capable of negative dynamic progress with possible death.
Ischemic and hemorrhagic stroke: differences
Doctors at the Yusupov Hospital make a diagnosis of stroke based on a thorough examination of the medical history, identification of risk factors and analysis of neurological symptoms.
Hemorrhagic and ischemic stroke have different symptoms. Manifestations of acute cerebrovascular accident depend on its nature and location of the pathological focus. Focal neurological symptoms of stroke are manifested by the occurrence of the following disorders:
- motor (complete and incomplete paralysis of one, two or four limbs, pathologically sudden involuntary movements in the limb, dysfunction of the cranial nerves);
- speech (impaired pronunciation, difficulty or inability to pronounce words while maintaining the pronunciation of individual sounds and understanding speech, impaired understanding of speech while maintaining the ability to speak);
- sensitive (abnormally low sensitivity to pain, lack of ability to distinguish between cold and heat, impairment of deep and complex types of sensitivity;
- coordinator (vestibular or cerebellar violation of the coordination of movements of various muscles in the absence of muscle weakness, loss of the ability to stand and walk);
- visual (the appearance of a blind spot in the visual field, not associated with its peripheral boundaries, bilateral blindness in half of vision, partial or complete blindness, not accompanied by visible damage and deficiencies of the organ of vision itself);
- cortical functions (astereognosis, apraxia);
- memory (time disorientation, fixation amnesia).
General cerebral symptoms are manifested by a decrease in the level of wakefulness from subjective feelings of “vagueness,” “fogginess” in the head and mild stupor to deep coma, headache and pain along the spinal roots, nausea and vomiting.
Neurologists at the Yusupov Hospital identify meningeal symptoms in stroke patients:
- tension in the posterior cervical muscles;
- positive symptoms of Kernig, Brudzinsky - lower, middle, upper, and ankylosing spondylitis.
For hemorrhagic and ischemic strokes, there are no symptoms unique to this type of circulatory disorder. Neurologists at the Yusupov Hospital take into account the following combination of signs to make a diagnosis of hemorrhagic stroke:
- the presence of high blood pressure and evidence of previous hypertensive cerebral crises;
- acute onset of the disease, often in the morning or afternoon, during vigorous activity;
- rapidly progressive deterioration of the patient's condition;
- development of coma in the first minutes or hours of the disease;
- the predominance of general cerebral symptoms over focal ones;
- severe autonomic disorders (pallor or flushing of the face, increased body temperature, sweating, greasiness of the skin;
- early onset of symptoms caused by displacement and compression of the brain stem.
At the onset of the disease, single or repeated vomiting and a generalized convulsive seizure are possible. The following signs are characteristic of an ischemic stroke:
- data that the patient suffers from coronary heart disease, diabetes mellitus, suffered a myocardial infarction or transient ischemic attack;
- slow progression of symptoms of acute cerebrovascular accident;
- development of an acute disorder;
- the predominance of focal symptoms over cerebral manifestations.
The disease debuts against the background of normal or low blood pressure numbers.
Can an ischemic stroke turn into a hemorrhagic stroke? This is possible if, against the background of high blood pressure in patients suffering from ischemic stroke, a cerebral artery ruptures. Make an appointment
Clinical picture
A major stroke occurs with damage to a large area of the brain. The clinical picture is pronounced, and the damage poses a danger to the patient’s life. It is important to seek emergency help if the victim exhibits the following symptoms:
- a sharp decrease in hearing and vision, impaired coordination of movements, inability to concentrate;
- acute headache, dizziness;
- nausea and vomiting;
- redness of the skin and mucous membranes or their pallor;
- decreased skin sensitivity, often on one side of the face or torso, muscle paralysis;
- the appearance of memory lapses;
- fainting.
With a major stroke, there is still a risk of developing coma. This is a condition in which the victim does not respond to any external stimuli, but his breathing and heartbeat continue. The coma can last for a long time, and the chances of further recovery depend on this.
What examinations are needed
In order to determine the type of stroke, doctors at the Yusupov Hospital examine patients using the latest equipment from leading companies in the world.
Ischemic and hemorrhagic stroke. Differences. Table No. 1.
| Examination method | Hemorrhagic stroke | Ischemic stroke |
| ECG | Hypertrophy of the heart | Ischemic, post-infarction changes in the myocardium, rhythm disturbances |
| Ocular fundus | Hemorrhages, altered blood vessels | Vascular changes (vasculitis, atherosclerosis) |
| Magnetic resonance imaging of the brain | Allows you to obtain an image of hemorrhage and hematoma, identify signs of cerebral edema and blood entering the cerebrospinal fluid pathways and their displacement. | Allows you to obtain an image of the area of necrosis (infarction), including in the area of the trunk, to identify signs of perifocal edema and displacement of the liquor-dynamic pathways. |
| ECHO-encephaloscopy | M-Echo is mixed towards the unaffected hemisphere, signs of intracranial hypertension and cerebral edema, signals from a limited hematoma may be observed | M-Echo in most cases is not displaced; in the first days of a stroke there may be interhemispheric asymmetry of up to 2 mm |
Computed tomography of the brain in the first hours of brain disease allows us to establish an ischemic stroke in 60%, and a hemorrhagic stroke in 100%.
Before a planned neurosurgical intervention to confirm the pathology of cerebral vessels at the Yusupov Hospital, patients undergo X-ray contrast angiography. Modern examination methods that allow distinguishing ischemic stroke from hemorrhagic stroke are ultrasound examination of the arteries of the head, duplex scanning, and transcranial Doppler sonography. In case of hemorrhagic stroke, echocardiography determines dilatation of the heart cavities and hypertrophy of the heart walls, and in the case of ischemic stroke, signs of myocardial pathology, heart defects, and the presence of blood clots in the cavities of the heart.
Any course of acute cerebrovascular accident, regardless of the type of stroke, is always a life-threatening condition for the patient. It is capable of negative dynamic progress with possibly frequent death.
Call and they will make an appointment with a neurologist. Doctors at the Yusupov Hospital use modern diagnostic equipment to diagnose stroke and determine the type of cerebrovascular accident. The knowledge and experience of professors and doctors of the highest category allow for quick differential diagnosis and prescribing effective treatment.
The most dangerous stroke
Hemorrhage or blockage of blood vessels in the brainstem and cerebellum is the most dangerous form of stroke. Mortality occurs in 85% of cases: either within a matter of days or in the first hours after the impact. If this is a young man or woman who was taken on time to a clinic that specializes in operations for pathologies of this type, the chance of recovery is 15–20%.
In the affected area there are nerve centers that control vital functions: the functioning of the cardiovascular system and breathing. Special external signs: impaired swallowing, complete paralysis. Symptoms of this insidious disease:
- Precursor: weakness and dizziness - it is difficult to stand, walk and even sit. Possible sudden fall. Occurs in 60–70% of patients.
- Paralysis: spreads both to half the body and throughout the entire body, immobilizing the person completely. He understands this if he is conscious.
- Dysphagia: inability to swallow food. It is observed in 60% of patients.
- Dysarthria: speech disorders. Appears in 30–40%.
- Ptosis, eye disorders.
- Distorted face.
- Respiratory failure, bradycardia, low blood pressure, high temperature are harbingers of a disappointing prognosis. Most likely, the patient will die.
Editorial: How to get out of depression after breaking up with your loved one
A person may fall into a coma, while the eyeballs continue to move. Based on external manifestations, we can conclude that the affected area is the brain stem. The exact diagnosis is confirmed using CT or MRI.
Subarachnoid hemorrhage
Subarachnoid bleeding occurs spontaneously, in 50% of cases the cause is a rupture of an arterial aneurysm. High blood pressure provokes 30% of such attacks. The third source of apoplexy is traumatic brain injury. In other cases (7–10%) there are other factors: tumor, pathology of the spinal cord vessels, etc.
The average age of those affected by this disease is 45 years. Occurs in adults aged 30 - 60 years. The disease affects, according to various statistics, from 6 to 16 people out of 100 thousand. Most of the symptoms coincide with hemorrhagic manifestations of the disease. The following reasons lead to the disease:
- cocaine addiction;
- sickle cell anemia usually affects children;
- poor blood clotting;
- smoking;
- chronic alcoholism, or one-time consumption of alcohol, but in large volumes;
- blood pressure problems;
- overweight, obesity.
How does a subarachnoid stroke occur? During hemorrhage, blood enters under the arachnoid membrane and fills the basal cisterns and sulci of the hemispheres. ACVA can be focal or cerebral, covering the entire space. Vascular spasm occurs, which increases gradually. Patients get worse within 3-4 days.
This is an antispasmodic consequence of hemorrhage, the peak of which occurs after a week or two. If urgent surgery is not performed, a person will die with a massive cerebral infarction. In 20–25% of patients, hemorrhage recurs, after which in 70% of cases death is inevitable.
Characteristic symptoms:
- Bursting (burning sensation) sharp pain in the head.
- Fainting or loss of consciousness may occur for several days.
- There is a fear of light and noise, stiffness of the neck muscles, etc.
- Body temperature rises.
- Involuntary motor activity is observed.