Rehabilitation after stroke
Recovery or rehabilitation after a stroke is a set of measures aimed at returning the abilities and functions of the body lost due to impaired blood circulation in the brain. Rehabilitation after a hemorrhagic stroke, as after an ischemic one, requires the involvement of specialized specialists. This allows you to restore lost abilities with minimal functional impairment. To rehabilitate people who have suffered a stroke, a group of doctors specializing in this issue works at the New Hospital. Our rehabilitation center in Yekaterinburg helps patients get back on their feet and return to a full life.
Symptoms
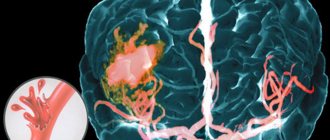
The term “stroke” in medical practice refers to a pathology in which there is a circulatory disorder in any part of the brain. After an attack, certain brain structures are damaged, causing the person to lose (partially or completely) certain skills. There are two types of this pathology:
- ischemic stroke - a circulatory disorder due to partial or complete blockage of a vessel;
- hemorrhagic stroke is a violation of the integrity of a vessel with subsequent hemorrhage in the brain.
Clinical manifestations of the pathology vary depending on which part of the brain was affected (left or right side, specific area), as well as the severity of the “impact” (the extent of damage to brain tissue). In most cases, rehabilitation after a hemorrhagic stroke is longer and more complex, since the nature of the lesions is more severe.
Lesions due to stroke
Severe vascular disorder leads to deterioration of various functions of the eye. Damage to the visual analyzer leads to disorders of peripheral (perception of the surrounding background), central (analysis of shapes of objects), binocular vision (recognition of volumes and reliefs), color and light perception (brightness).
The severity of the deviations is determined by the nature and location of the damage to the brain tissue. Among the symptoms from the ophthalmological system characteristic of a stroke:
- Loss or deterioration in image quality in both or one eye.
- Split image.
- Narrowing of the visual field, loss of images in certain areas.
- Visual hallucinations.
- Constant pain in the eyelids and temples.
- Decreased or complete loss of lateral vision.
- Strabismus, difficulty focusing the image.
- Protruding, trembling of the eyeball.
- Loss of visual movement control.
- Impaired coordination and accuracy of movements.
Stroke treatment
The promptness and correctness of treatment carried out after an attack directly affects the success and timing of rehabilitation, as well as life after a stroke in general. It doesn’t matter whether the stroke occurred on the left or right side, the type of pathology plays a role in treatment:
- Ischemic - all actions are aimed at restoring blood circulation and eliminating the causes of vascular obstruction. To do this, medications that thin the blood, dissolve blood clots are used, or non-invasive methods are used to destroy blood clots.
- Hemorrhagic - first of all, it is necessary to stop the hemorrhage with medication. The resulting blood clot is then surgically removed, and aspiration may be used.
Types of eye stroke
An ocular stroke can be localized in the venous or arterial bed of the retinal circulatory system. If the accident occurred in a venous vessel, they speak of retinal vein thrombosis. The blockage can occur in the central retinal vein (CRV) or in its branches (the superior temporal branch is affected in 82% of cases). A major role in retinal vein occlusion is played by disruption of the internal vascular epithelium, which predisposes to the formation of blood clots.
Obstruction of outflow leads to stagnation of blood and increased intravenous pressure. In this case, the liquid begins to seep through the walls of the vessel. Their rupture may also occur. Blood fills the eye space, swelling increases, and intraocular pressure increases even more. This is fraught with compression of small capillaries, which further limits the outflow of fluid and aggravates retinal hypoxia. This cycle of mechanisms of the pathological process is called a “vicious circle”.
Closure of the lumen of an arterial vessel is called arterial occlusion. There are occlusions of the central retinal artery (CRA), its branches and the cilioretinal artery. Often the blockage occurs in the CAS; the branches are affected with less frequency. The cause of artery blockage in most cases is cholesterol, fibrin thrombus or calcification embolism.
The embolus blocks the access of nutrition to the retina - ischemia develops. Clinical symptoms of visual impairment develop quickly. If medical assistance is provided within the first 40 minutes from the onset of symptoms, vision can still be fully restored. Delaying therapy threatens irreversible consequences.
Comprehensive program “Rehabilitation+”
This stroke rehabilitation program aims to return patients to as full a life as possible.
The main task of the specialists at the “New Hospital” is a separate approach to each patient. We use maximum opportunities to restore lost skills:
- restoration of vision;
- motor activity (recovery of arms and rehabilitation of legs after a stroke, fine motor skills);
- speech restoration;
- learning to tie shoelaces, wash dishes, etc.;
- restoration of driving skills.
As part of the program, our specialists try to restore not only the basic skills that were lost. We try to return the patient to a full life, focusing on the tasks that are necessary for a specific person.
Rehabilitation plan
In our stroke recovery center, an individual rehabilitation plan is developed for each patient.
It takes into account the degree of brain damage, the patient’s age, type of stroke, etc. The best specialists are working to create a plan, studying in detail the medical history, the patient’s life, and recording lost abilities. Thus, after an ischemic stroke of the brain, rehabilitation can be radically different for 2, 3, 5 or more patients. This is explained by the fact that the characteristics of the lesion are different in each case and must be taken into account when creating a plan.
Treatment
An ocular stroke is an absolute indication for emergency hospitalization and treatment under 24-hour observation.
Treatment of arterial and venous stroke does not differ significantly. The goal of treatment for these conditions is general; it is to cleanse the lumen of the vessel, strengthen the vascular wall, restore vision, eliminate intraocular hemorrhage (if any), and prevent relapse. Several groups of drugs are used for these purposes:
- Thrombolytics. Substances for resorption of blood clots. For the best effect, drugs are injected under the eye, under the conjunctiva or directly into the cavity of the eyeball.
- Drugs to dilate the lumen of the vessel. They can also reduce the sticking of red blood cells and platelets to the vessel wall, preventing blockages.
- Means for protecting and restoring the inner lining of blood vessels. They are used in treatment and as a prevention of a recurrent episode of pathology.
- Blood thinners. They help resolve blood clots and prevent relapse.
- For retinal edema, glucocorticosteroids are often added to treatment.
- Drugs to reduce intraocular pressure. If the pressure remains high, or it needs to be reduced as soon as possible, resort to puncture of the cornea.
If the blood density is high, hemodilution is performed - a method of thinning the blood by intravenous administration of solutions similar in composition to blood plasma. Surgical treatment is resorted to when conservative therapy is ineffective and in difficult cases (compression of the optic nerve head, retinal detachment, compression of a vessel from the outside).
In case of arterial occlusion, in the first 8 hours it is necessary to massage the eyeball. This helps displace the thrombus to the periphery. The head lies low. The eyelids are closed. You need to press your fingers on the eyeball over the upper eyelid for 3-5 seconds, first weakly, then harder. When pressing on the eye, intraocular pressure in the small arterioles increases, which slightly increases the blood flow to the eye.
When the pressure on the eyeball stops, the pressure drops sharply. Changes in pressure cause the clot to move, it moves, freeing up blood access. This is not a therapeutic measure, but a way to extend the time before starting therapy so as not to worsen retinal hypoxia.
For any type of stroke, treatment of the underlying disease that caused the embolism is necessary.
Restoration of motor functions
At the “New Hospital” in Yekaterinburg, rehabilitation specialists, neurologists and physical therapy doctors are involved in the restoration of motor functions. The tasks in this case are:
- stimulation of muscle activity;
- muscle strengthening;
- massage;
- stimulation of coordination between the brain and organs of the musculoskeletal system.
In this case, the main thing is to create a safe environment for the patient. To achieve the goal, special products for rehabilitation after a stroke are used (canes, walkers, exercise equipment, etc.).
Causes of vision loss
Loss of vision (amaurosis) can be a consequence of retinal detachment or ischemia and other eye diseases (for example, glaucoma or uveitis), damage to the optic nerves, or bilateral damage to the visual cortex. Patients with acutely developed visual impairment should be urgently hospitalized. At the same time, the information that the emergency doctor is able to collect about the development of vision loss is important and helps to quickly establish a diagnosis at the hospital stage. In this article we will look at what sudden loss of vision is and the causes of this disease.
Causes of vision loss and blindness
Sudden loss of vision in one eye usually results from damage to the retina and other structures of the eye or the optic nerve. One of its common causes is a transient circulatory disorder in the retina. Typically, patients complain of a veil that suddenly falls in front of the eye and sometimes covers only part of the field of vision. Sometimes sensory disturbances and transient weakness in opposite limbs are simultaneously observed. The duration of the episode ranges from several minutes to several hours.
In 90% of cases, the cause is retinal artery embolism from an ulcerated atherosclerotic plaque in the internal carotid artery, aortic arch, or from the heart (often with valvular disease or atrial fibrillation). Less commonly, the cause of vision loss is a drop in blood pressure in a patient with severe stenosis of the internal carotid artery. Sudden loss of vision in one eye is a harbinger of a stroke and should be a reason for active examination of the patient. The likelihood of developing a stroke can be reduced by constant intake of aspirin (100–300 mg per day) or indirect anticoagulants (for cardiogenic embolism).
Migraine as a cause of vision loss
In young people, retinal migraine may cause transient blindness in one eye. The loss of vision in this case is a migraine aura that precedes an attack of headache or occurs shortly after its onset. However, even with a typical history, it is advisable to exclude pathology of the carotid arteries and heart using a special study. The differential diagnosis is also made with a visual aura in the form of a migrating scintillating scotoma during an attack of classic migraine, but the visual aura usually involves the right and/or left visual fields in both eyes, and not one eye, in addition, it remains visible in the dark and when closing the eyes .
Vision loss due to ischemic neuropathy
Anterior ischemic optic neuropathy is caused by insufficient blood flow through the posterior ciliary artery, which supplies the optic disc. Clinically, it manifests itself as a sudden loss of vision in one eye, not accompanied by pain in the eyeball. The diagnosis of vision loss can be easily confirmed by fundus examination, which reveals swelling and hemorrhage in the area of the optic nerve head.
Most often it develops in patients with long-term arterial hypertension and diabetes mellitus, often in patients with vasculitis or polycythemia. In 5% of cases (especially often in patients over 65 years of age), neuropathy is associated with temporal arteritis and requires immediate corticosteroid therapy to prevent loss of vision in the second eye. The diagnosis of temporal arteritis is facilitated by identifying painful thickening and absence of pulsation of the temporal artery and signs of polymyalgia rheumatica.
Posterior ischemic optic neuropathy is less common. It is usually caused by a combination of severe anemia and hypotension and may cause retrobulbar nerve infarction. Sometimes posterior ischemic neuropathy occurs against the background of massive blood loss during surgery, gastrointestinal bleeding, or trauma. There are no changes in the fundus. In hypertensive crisis, a sudden drop in vision may be a consequence of spasm of the retinal arterioles or ischemic edema of the optic nerve head. An excessively rapid decrease in blood pressure can lead to optic disc infarction.
Causes of vision loss: optic neuritis
Optic neuritis, an inflammatory demyelinating disease, often involves the retrobulbar part of the nerve (retrobulbar neuritis), so pathology cannot be detected during the initial examination of the fundus. Most patients, in addition to acute loss of vision, experience pain in the eyeball, which intensifies with its movement. Vision loss often develops at a young age, can recur, and is often the first manifestation of multiple sclerosis. Intravenous administration of large doses of methylprednisolone (1 g per day for 3 days) accelerates recovery.
Loss of vision due to toxic neuropathy
Sudden blindness in both eyes may be a manifestation of toxic optic neuropathy. Toxic neuropathy may be associated with methyl alcohol, ethylene glycol (antifreeze), or carbon monoxide poisoning. A more gradual development of optic neuropathy with increasing atrophy without a disc swelling phase can be caused by a number of drugs - chloramphenicol (chloramphenicol), amiodarone, streptomycin, isoniazid, penicillamine, digoxin, ciprofloxacin, as well as lead, arsenic or thallium poisoning.
Loss of vision due to increased intracranial pressure
Blindness can also be a consequence of intracranial hypertension and the development of congestive optic discs (with benign intracranial hypertension or brain tumors). It is often preceded by short-term episodes of blurred vision in one or both eyes, occurring when changing body position and lasting several seconds or minutes. In case of persistent loss of vision, administration of methylprednisolone (250–500 mg intravenously) and urgent consultation with an ophthalmologist and neurosurgeon are necessary.
Infarction of the occipital lobes of the brain as a cause of vision loss
Acute blindness in both eyes can also be a consequence of bilateral infarction of the occipital lobes (cortical blindness) and occur as a result of blockage of the basilar artery (usually as a result of embolism) or prolonged systemic arterial hypotension. The source of embolism is usually atherosclerotic plaques in the vertebral arteries. Vision loss is often preceded by episodes of vertebrobasilar insufficiency with unilateral or bilateral paresthesias or paresis, ataxia, dysarthria, hemianopsia, dizziness, double vision. Unlike bilateral blindness caused by damage to the optic nerves, with cortical blindness, pupillary reactions remain intact. Some patients with cortical blindness develop anosognosia: such a patient denies the presence of blindness, claiming that the room is dark or he simply forgot his glasses.
Acute loss of vision as a symptom of hysteria
Acute loss of vision may be psychogenic in nature and be one of the manifestations of hysteria. Typically, such patients (usually young women) claim that everything around them is immersed in darkness (patients with organic cortical blindness often find it difficult to describe their visual sensations). The history often reveals other hysterical symptoms (lump in the throat, pseudoparesis, hysterical seizures, mutism, hysterical gait disturbances). Pupillary reactions are normal, there are no stem symptoms. Unlike those around them, whose obligatory presence and extreme concern can serve as an additional diagnostic criterion, patients are often not alarmed, but rather calm, and sometimes even smile mysteriously (“beautiful indifference”).
© Author: therapist Elena Dmitrenko
Stroke
Stroke, stroke treatment, stroke prevention, hemorrhagic stroke, ischemic stroke, International Center for Neurosurgery.
Definition
A stroke occurs when blood flow to part of the brain is stopped or significantly reduced. As a result, the brain does not receive enough oxygen and the nutrients it needs. Within minutes, brain cells begin to die.
Stroke is a medical emergency because prompt medical attention can minimize brain damage and possible complications.
The good news is that stroke can be treated and prevented. The key to preventing stroke is strict control of the main risk factors for stroke. These include: high blood pressure, smoking and high cholesterol.
Symptoms of a stroke
Look for the following symptoms if you think you or someone you know may be having a stroke. Also remember when these symptoms started, as how long they last may have an impact on treatment options.
Main symptoms:
- Walking disorder.
- Impaired speech and understanding of words.
- Paralysis or numbness on one side of the face or entire body.
You may feel sudden numbness, weakness, or paralysis on one side of your body. Try raising both arms above your head. If one arm begins to fall, you may have a stroke. Likewise, one side of the mouth may fall down when trying to smile. - Visual impairment on one or both sides.
- Headache.
A sudden, severe, “out of the blue” headache that may be accompanied by vomiting, dizziness, or confusion.
When should you see a doctor immediately?
If you notice any of the above signs, even if they change or disappear, call an ambulance immediately. In the event of a stroke, every minute counts. Don't wait, even if your stroke symptoms begin to subside. The later treatment for a stroke is started, the greater the likelihood of brain damage and disability. To ensure maximum effectiveness of stroke treatment, it is necessary to transport the patient to the hospital within 60 minutes of the first symptoms.
What can you do while waiting for an ambulance?
Causes of stroke
When a stroke occurs, blood flow through the brain is disrupted and brain tissue is damaged. There are two main types of stroke. The most common type is ischemic stroke, which results from blockage of blood flow through an artery. Another type, hemorrhagic stroke, occurs as a result of bleeding from a blood vessel in the brain. A transient ischemic attack (TIA)—sometimes called a mini-stroke—occurs when blood flow through the brain is temporarily interrupted.
Ischemic stroke
Almost 90 percent of strokes are ischemic strokes. They occur when the arteries in your brain become narrowed or blocked, resulting in a sharp reduction in blood flow to the brain (ischemia). The lack of blood flow deprives brain cells of oxygen and nutrients, and the cells can begin to die within minutes. The most common types of ischemic stroke are:
- Thrombotic stroke.
This type of stroke occurs when a blood clot (thrombus) forms in one of the arteries supplying blood to the brain. The clot usually forms in areas affected by atherosclerosis, a disease in which the arteries are clogged with fatty deposits (plaques). The process can occur in one of the two carotid arteries that run through the neck and carry blood to the brain, as well as in other arteries in the neck or brain. - Embolic stroke.
An embolic stroke occurs when a blood clot forms in blood vessels outside the brain—usually in your heart—and travels through the bloodstream into narrower arteries in the brain. This type of blood clot is called an embolus. The cause is an irregular heartbeat (atrial fibrillation). This abnormal heart rhythm can cause blood clots to form in the chambers of the heart, from where they travel to other parts of the body.
Hemorrhagic stroke
Hemorrhage is the medical term for bleeding. A hemorrhagic stroke occurs when a blood vessel in the brain leaks or ruptures. Brain hemorrhages can result from a number of causes affecting the blood vessels, including uncontrolled high blood pressure (hypertension) and weak spots in the walls of blood vessels (aneurysms). A less common cause of hemorrhage is the rupture of an arteriovenous malformation (AVM), which is a tangle of thin-walled blood vessels and is a congenital pathology. There are two types of hemorrhagic stroke:
- Intracerebral hemorrhage, with
this type of stroke, blood leaks from a blood vessel in the brain into surrounding tissue, damaging cells. Brain cells are also damaged due to impaired blood supply. High blood pressure is a common cause of this type of hemorrhagic stroke. With long-term hypertension, high blood pressure can cause small arteries inside the brain to crack and collapse, leading to hemorrhage. - Subarachnoid hemorrhage, in
this type of stroke, bleeding develops in the arteries near the surface of the brain, and the hemorrhage occurs in the space between the surface of the brain and the skull. Bleeding is often signaled by a sudden, severe headache. This type of stroke is usually associated with a ruptured aneurysm, which may be congenital or develop with age. After a hemorrhage, the brain's blood vessels may widen or narrow randomly (vasospasm), causing damage to brain cells, further restricting blood flow to parts of the brain.
Transient ischemic attack (TIA)
A transient ischemic attack (TIA)—sometimes called a mini-stroke—is a brief episode of symptoms similar to those of a stroke. A transient ischemic attack is caused by a temporary decrease in blood flow to part of the brain. Most TIAs last less than five minutes.
As with an ischemic stroke, in a TIA, a clot disrupts blood flow to part of the brain. But unlike a stroke, which is characterized by a longer-term lack of blood supply and often permanent tissue damage, a TIA does not cause significant damage because the blockage of the vessel is temporary.
Seek emergency medical help even if your symptoms begin to subside. If you have had a TIA, it means that the blood vessels leading to the brain are partially blocked or narrowed and you are at high risk of having a severe stroke. It is difficult to differentiate between a stroke and a TIA based solely on the presence of symptoms of the disease. Some symptoms go away even in the presence of a stroke with brain damage.
Risk factors
Many factors can increase your risk of stroke. Some of these factors also increase your risk of developing heart disease. Risk factors for stroke include:
- Have a personal or family history of stroke, heart attack, or TIA.
- Age 55 years and older.
- High blood pressure. The risk of stroke begins to increase as blood pressure rises above 115/75 mmHg.
- High cholesterol - total cholesterol levels above 5.2 mmol/L.
- Smoking cigarettes or passive smoking.
- Diabetes.
- Overweight (body mass index of 25 to 29) or obese (body mass index of 30 or higher).
- Lack of physical activity.
- Cardiovascular disease, including heart failure, heart disease, heart infection, or abnormal heart rhythm.
- Using birth control pills or hormone therapy that includes estrogen.
- Alcohol consumption.
- Drug use.
Because the risk of stroke increases with age and women tend to live longer than men, women are more likely to suffer and die from stroke.
Complications
A stroke can cause temporary or permanent disability, depending on how long the brain suffers from lack of blood flow and what part of the brain is affected. Complications may include:
- Paralysis or loss of muscle movement.
Sometimes a lack of blood flow to the brain can cause paralysis on one side of the body or loss of control of certain muscles, such as on one side of a person's face. Physical therapy may lead to improved muscle movement or decreased paralysis. - Speech or swallowing problems.
A stroke can cause loss of muscle control in the throat and mouth, making it difficult to speak, swallow, and eat in general. For a person, having aphasia can be a severe condition in which they experience difficulty expressing thoughts through language. Sessions with a speech therapist and psychotherapist can improve this condition. - Memory loss or difficulty understanding.
Typically, people who have had a stroke have some memory impairment. Others may have difficulty making decisions, reasoning, and understanding concepts. Improvement may be due to rehabilitation therapy. - Pain.
Some people who have had a stroke may complain of pain, numbness, or other strange sensations in parts of the body affected by the stroke. For example, if a stroke caused loss of sensation in your left arm, you may feel a tingling sensation in that arm. You may also become sensitive to temperature changes. This is called central stroke pain or central pain syndrome. The complication usually develops several weeks after the stroke and may subside over time. Sometimes requires treatment. - Changes in behavior and self-care.
People who have had a stroke may become more withdrawn and less socially active. They may lose the ability to care for themselves and often need outside care and daily care.
As with any traumatic brain injury, the success of treating these complications will vary from person to person.
Examination and diagnosis
To determine the most appropriate treatment, the emergency team must find out what type of stroke the patient has and what parts of the brain are affected. Other possible causes of symptoms, such as a brain tumor or drug reaction, must be ruled out. The doctor may use the following tests:
- Physical examination.
The doctor will ask you or a family member about your symptoms, when they started, medications you take, any head injuries, and your personal and family medical history. He will check your blood pressure, listen to your heart and sounds (murmurs) over your carotid arteries, which may indicate atherosclerosis. The doctor may also use an ophthalmoscope to check for signs of tiny cholesterol crystals or blood clots in the blood vessels at the back of the eye. - Blood tests.
Blood tests provide important information about how quickly your blood clots, what your blood sugar levels are, whether you have an infection, and what your blood chemistry levels are, which is important for deciding how to treat your stroke. - Computed tomography (CT).
An image of the brain that plays a key role in determining the presence of a stroke and its type. A CT angiography scan is a specialized test in which dye is injected into a vein and X-rays create a 3-D image of the blood vessels in the neck and brain. Doctors use this test for aneurysms and arteriovenous malformations to assess the degree of narrowing of the arteries. CT without angiography can provide an image of the brain and show hemorrhage, but provides less information about the blood vessels. - Magnetic resonance imaging (MRI).
In this type of examination, a strong magnetic field and radio waves create a 3-D image of the brain. MRI can reveal damage to brain tissue during an ischemic stroke. Magnetic resonance angiography (MRA) uses magnetic fields, radio waves and a dye injected into a vein to evaluate the arteries of the neck and brain. - Ultrasound examination of the carotid arteries.
This procedure may show narrowing of the arteries or the presence of blood clots in the carotid artery. - Arteriography.
- Echocardiography.
Ultrasound technology creates an image of the heart and allows the doctor to identify blood clots in the cavities of the heart.
Stroke treatment
Emergency treatment for stroke depends on its type - ischemic or hemorrhagic stroke.
Ischemic stroke
To treat an ischemic stroke, doctors must quickly restore blood flow to the brain.
Treatment with drugs.
Treatment with blood thinners should begin within 4.5 hours - the sooner the better. This improves the chances of survival and reduces stroke complications. For this use:
- Aspirin.
Aspirin is the most proven effective drug for the immediate treatment of ischemic stroke, reducing the likelihood of a recurrent stroke. The dose of the drug may vary.
Other blood thinners such as warfarin, heparin and clopidogrel may also be used, but not for emergency treatment.
- Administration of tissue plasminogen activator (tPA).
Some patients with ischemic stroke will benefit from early administration (within 4.5 hours of onset) of tissue plasminogen activator (tPA), which dissolves the clot and restores blood flow in the blocked artery. The administration of this drug is contraindicated for hemorrhagic stroke.
During treatment
ischemic strokes often require procedures that must be performed as quickly as possible. These are the following procedures:
- Using tissue plasminogen activator (tPA) delivered directly to the brain.
Doctors may use catheters to inject this drug into the brain. - Mechanical clot removal.
Doctors also use a catheter to maneuver into the brain to mechanically remove the clot.
Other procedures.
To reduce the risk of another stroke or TIA, your doctor may recommend procedures to open arteries narrowed by plaque. These may include:
- Endarterectomy of the carotid arteries
. In this procedure, the surgeon removes plaque blocking the carotid arteries in the neck. The blocked artery is opened and the plaque is removed. The procedure may reduce the risk of ischemic stroke. However, carotid endarterectomy itself can also cause a stroke or heart attack by promoting blood clot formation. To reduce the risk of stroke, special filters are used at strategic points in the blood flow. - Angioplasty and stenting.
Angioplasty is another method of widening the arteries leading to the brain, usually the carotid arteries. This procedure uses a catheter balloon that inflates to compress the plaque and dilate the arteries. More often, stenting is used with the placement of special metal tubes (stents) in the narrowed areas of the arteries, which remain in the artery, preventing its narrowing. Placing a stent in an artery in the brain (intracranial stenting) is similar to stenting in the carotid arteries.
Hemorrhagic stroke
Acute treatment of hemorrhagic stroke focuses on controlling bleeding and reducing pressure in the brain.
Emergency measures.
If you are taking warfarin or antiplatelet drugs to prevent clots, such as clopidogrel (Plavix), you may receive blood transfusions or medications to counteract the effects of warfarin or clopidogrel. You may need medications to lower your blood pressure. The use of aspirin and tissue plasminogen activator is prohibited because it may worsen bleeding.
Treatment for hemorrhage usually involves bed rest. If the bleeding area is large, surgery may be needed to remove the blood and relieve pressure on the brain.
Surgical reconstruction of blood vessels.
Surgery may be used to repair certain blood vessel abnormalities associated with hemorrhagic stroke. A doctor may recommend one of these procedures after a stroke or if there is a high risk of spontaneous rupture of an aneurysm or arteriovenous malformation (AVM):
- Aneurysm clipping.
Tiny clamps are placed at the base of the aneurysm, sealing it off from blood flow in the artery. This may keep the aneurysm from rupturing or prevent the aneurysm from bleeding again. The clip remains in place permanently. - Embolization of aneurysm.
This procedure is an alternative to aneurysm clipping. Surgeons use a catheter to maneuver inside the aneurysm. - Surgical removal of AVM.
Surgical removal of small AVMs in accessible parts of the brain can eliminate the risk of rupture and reduce the overall risk of hemorrhagic stroke. This does not apply to AVMs that are too large or deep inside the brain.
Recovery and rehabilitation
After initial measures, stroke treatment focuses on helping the patient regain strength, function, and return to independent living. The effect depends on the area of the brain damaged and the extent of the damage. Damage to the right side of the brain can affect movement and sensation in the left side of the body. Damage to the left side of the brain can affect movements on the right side and can cause speech disorders. In addition, stroke patients may have problems breathing, swallowing, balance, and hearing. Possible loss of vision, impaired bowel and bladder function.
People who have suffered a stroke need treatment using rehabilitation programs. Your doctor will help you choose a program based on your age, general health, and degree of disability. Lifestyle, interests and priorities, and the presence of other family members are also taken into account.
A rehabilitation program may begin before hospital discharge. It can continue in specialized rehabilitation departments, sanatoriums, and at home. The extent of recovery from a stroke varies from person to person.
Stroke Prevention
The key to preventing stroke is identifying risk factors, following your doctor's recommendations, and maintaining a healthy lifestyle. If you've had a stroke or TIA, these steps will also help prevent another. A healthy lifestyle includes:
- Controlling high blood pressure (hypertension).
If you have had a stroke, lowering your blood pressure will help prevent another transient ischemic attack or stroke. Managing stress, maintaining a healthy weight, and limiting salt and alcohol intake will help keep your blood pressure under control. Adding more potassium to your diet may also help. In addition to recommendations for lifestyle changes, your doctor may prescribe medications to treat high blood pressure, such as diuretics, calcium antagonists, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers. - Reduce cholesterol and saturated fat in your diet.
Diet adjustments and statin use are necessary to lower cholesterol levels. - To give up smoking.
Smoking increases the risk of stroke for smokers and nonsmokers exposed to secondhand smoke. Quitting smoking reduces risk several years after quitting. - Diabetes control.
Diabetes can be managed through diet, exercise, weight control and treatment. - Healthy weight support.
Excess weight contributes to other risk factors for stroke, such as high blood pressure, heart disease and diabetes. Losing weight can lower blood pressure and reduce blood cholesterol levels. - Maintain a diet rich in fruits and vegetables.
A diet containing five or more servings of fruits or vegetables may reduce the risk of stroke. - Physical activity.
Aerobic exercise reduces the risk of stroke in different ways. Exercise can lower blood pressure, increase high-density lipoprotein (“good” cholesterol) levels, and improve overall blood vessel and heart health. It also helps you lose weight, control diabetes and reduce stress levels. 30 minutes of activity - walking, running, swimming or cycling - gives good results.