Classification of pathology
All cysts localized in the cerebellum are usually divided into two large groups:
- primary – that is, congenital;
- secondary – acquired pathology.
There are several types of cysts. This classification is based on the causes and location of the pathological formation:
- Cystic-glial formations in the right half of the cerebellum. They arise as a result of previous TBI.
- Cystic-atrophic cysts in the right half of the cerebellum. This pathology is characterized by the presence of necrotic and atrophied areas.
- Cystic-glial formations in the left half of the cerebellum are characterized by severe symptoms.
- Lacunar cyst in the left half of the cerebellum. These are small formations, they are usually single. This form of the disease does not require treatment.
- A retrocerebellar cyst forms in the place where there is tissue necrosis.
- Cyst-like expansion in the subarachnoid space.
- Arachnoid cerebrospinal fluid cyst.
- Pseudocyst is a congenital formation of the cerebellum.
Arachnoid cysts
Arachnoid cysts (AC) are congenital, predominantly extracerebral formations, the walls of which are the arachnoid membrane, and the contents are cerebrospinal fluid (CSF). In children, arachnoid cysts, according to various sources, account for about 10% of all volumetric formations of the brain and in 7.4% of cases are found in children with hydrocephalus. The division of arachnoid cysts into two large groups is pathogenetically justified: 1. Cysts of the cerebral hemispheres: - lateral (Sylvian) fissure; - convexital surface of the brain; - parasagittal interhemispheric fissures).
2. Mid-basal cysts: - suprasellar; - intrasellar; - tentorial notch; — posterior cranial fossa (upper and lower retrocerebellar, cysts of the cerebellopontine angle).
The group of mid-basal cysts can also include mid-stem cysts (retrocerebellar), since they are identical in their pathogenetic mechanisms.
The most common locations of arachnoid cysts are the Sylvian fissure (lateral fissure), interhemispheric fissure and suprasellar cistern. However, they can occur anywhere where the arachnoid membrane is located. Morphologically, the inner and outer walls of the cyst consist of thin layers of arachnoid cells and are often connected to the unchanged arachnoid membrane. Cysts can be congenital (primary) or acquired (secondary). Unless there is a history of trauma or inflammation, the cysts are considered congenital. Currently, there are several theories about the occurrence of arachnoid cysts. The first is the “intraarachnoid cyst theory,” in which cyst formation is the result of splitting and duplication of the arachnoid membrane. The second is the “subarachnoid cyst theory,” which explains the occurrence of middle cranial fossa cysts as a result of agenesis of the temporal lobe. The formation of arachnoid cysts occurs at the stages of embryogenesis during the formation of the membranes of the brain. Under pathological conditions, mainly with subarachnoid hemorrhage caused by hypoxia, infection, intoxication, etc., it becomes possible to form microcavities in the arachnoid membrane, which subsequently increase in size, turning into arachnoid cysts.
Most arachnoid cysts remain undiagnosed during life. The patient’s condition can remain compensated for a very long time, and the course of the disease is asymptomatic. The first manifestations can be noticed in adulthood. The timing of referral of children with congenital arachnoid cysts to neurosurgical departments, as a rule, depends on the location and size of the cysts. It is known that cysts of the tentorial notch cause more severe neurological symptoms. Common symptoms, which, however, manifest themselves to varying degrees in cysts of different localizations, include: - volumetric effect on the surrounding structures of the brain; — presence of an asymptomatic period; - no signs of inflammation in the membranes of the brain.
Positive meningeal symptoms are usually observed only when the disease is complicated by subarachnoid or intracystic hemorrhage. Hyperthermia and inflammatory changes in the blood are not typical for arachnoid cysts. — the severity of compensatory mechanisms and the absence of gross neurological manifestations in the presence of significant morphological changes, which is especially typical for hemispheric cysts. The clinical picture of arachnoid cysts is determined in most cases by three symptom complexes: hypertensive-hydrocephalic, focal neurological symptoms and damage to the brain stem. Signs of damage to the brainstem only in cysts of the cerebral hemispheres should be regarded as dislocation; in cysts of mid-basal localization, they can also be caused by the direct effect of the cyst on the brainstem. The uniqueness of the clinical picture of cysts in individual locations is determined by the duration of the asymptomatic period, the severity and characteristic coloring of the three leading neurological syndromes. It is believed that children with intracranial arachnoid cysts that have a mass effect should be operated on, because the volumetric effect of the cyst can lead to a delay in the development and formation of the brain, and rupture of the cyst is usually accompanied by intracystic and subdural bleeding. These complications justify the risk of surgical intervention. A direct indication for surgical treatment is progressive hydrocephalus that occurs when a cyst blocks the cerebrospinal fluid circulation pathways.
Currently, effective methods of surgical treatment of arachnoid cysts, including in the Department of Neurosurgery of the Russian Children's Clinical Hospital, are: perforation of the walls of the cyst with excision of its walls using the microsurgical method (through a small trefination window), as well as the neuroendoscopic method. CSF shunt operations are used extremely rarely.
Etiology
The causes of this pathology depend on which group it belongs to. The etiological factors for primary and secondary cysts are different.
Causes of primary formations:
- Anomalies of intrauterine development of the fetus.
- Asphyxia of the child during childbirth. In this case, necrotic areas of tissue are formed that have died from oxygen starvation.
Reasons for the development of secondary cysts:
- Traumatic brain injuries (skull fractures, concussion and bruises).
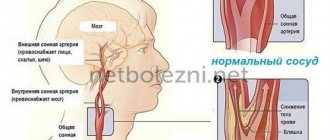
- Acute cerebrovascular accident (hemorrhagic and ischemic stroke).
- Inflammation in brain tissue.
- Surgical intervention.
- Tissue death as a result of stroke.
- Viral diseases of the brain (meningitis, encephalitis, meningoencephalitis).
- Hemorrhages from formed hematomas.
- Neuroinfections.
Causes
Due to their formation, they are divided into primary and secondary (acquired):
Primary: these are disorders that arose in the prenatal period and tissue necrosis (death of tissue in a living body) due to birth complications.
There are more secondary reasons:
- Past acute inflammatory process.
- Stroke.
- Brain surgeries.
- TBI.
- Parasitic diseases.
- Virus infection.
- Hematomas.
- Deterioration of blood circulation in the cerebral vessels.
- Replacement of cerebral cells with cystic tissue.
- Identifying the cause of the formation of the tumor is a primary task, since without its elimination, the cerebellar cyst will grow.
Clinical picture
Primary cysts most often do not manifest themselves in any way and do not interfere with a person’s life. As a rule, this pathology is not treated.
Symptoms of a secondary formation depend on its size and etiology. Small brain cysts do not have pathological symptoms; they are characteristic of large specimens. However, experts have identified several common signs of the disease:
- Severe pain in the head that is not relieved by painkillers.
- Dizziness, in some cases there is loss of consciousness.
- Bursting and pulsating sensations in the head area.
- Periodic nausea. Sometimes it ends in vomiting, which, in turn, does not bring relief.
- Disturbance of sleep and biological rhythms of patients.
- Cramps, tremor of fingers.
- Neurological symptoms.
- In children under one year of age, bulging and pulsation of the large fontanel and frequent regurgitation, in some cases vomiting, are observed.
- Coordination of movements worsens, gait changes.
- Partial or complete paresis and paralysis of the upper and lower extremities occur.
- Some areas of the skin may lose sensitivity.
- Pathological changes in hearing, vision, and speech are possible.
It is also necessary to note individual symptoms of cerebellar cysts depending on their type:
- hallucinations are characteristic of a retrocerebellar cyst;
- when the right half of the cerebellum is damaged, a person becomes quickly fatigued, both physical and mental;
- paralysis is more often observed with the development of pathology in the left half of the organ;
- hydrocephalus is a sign of cyst-like expansion of the subarachnoid space.
Indications for the study
The presence of a retrocerebellar cyst can be suspected by some characteristic symptoms:
- Severe headaches that do not go away even after taking painkillers;
- Unreasonable loss of consciousness or fainting state;
- Sensation of squeezing and pulsation in the head;
- Deterioration of hearing or vision;
- Arterial hypertension;
- Numbness of the limbs;
- Impaired coordination of movements;
- Epileptic seizures.
Magnetic resonance imaging is required if surgical intervention in the brain area is necessary.
Note that the clinical picture and severity of symptoms depend on the exact location and size of the retrocerebellar cyst.
Diagnostics
When a patient seeks medical help, it is necessary to carry out a number of diagnostic measures to make an accurate diagnosis. First of all, anamnesis is collected (patient complaints, previous injuries, diseases). After which the patient is sent for diagnostic studies:
- Magnetic resonance imaging and ultrasound examination. These methods help to clarify the location and size of the formation, as well as to identify its nature. They should be carried out periodically to monitor the dynamics of the pathology.
- Electroencephalography. With its help, convulsive readiness is revealed.
- NSG (neurosonography). This study is only carried out on children under two years of age.
- Histology determines the nature of the formation (cyst, benign or malignant tumor).
- Laboratory examination of cerebrospinal fluid. The analysis is carried out to detect inflammation and infection.
Treatment
Treatment of this disorder is aimed at eliminating the cause and symptoms, and it is also necessary to stop the growth of the pathological formation.
In this case, two treatment methods are used:
- medicinal – in patients with small cysts;
- surgical – in the presence of large cysts.
Medicines are prescribed only by a doctor, therapy is carried out under the control of laboratory blood parameters:
- Medicines for resolving adhesions and scars (“Longidaza”).
- Antibacterial drugs to eliminate infection.
- Immunomodulators to restore the body's defenses.
- Nootropics provide better nutrition and gas exchange of brain cells.
- It is also necessary to take a number of medications, the action of which is aimed at reducing blood cholesterol, normalizing blood pressure levels and thinning the blood.
Indications for the operation:
- Development of hydrocephalus and hypertension.
- Worsening of focal symptoms.
- The presence of hemorrhage in the brain tissue.
- Cramps.
- Severe loss of coordination and balance.
In modern medicine, three types of operations are used:
- Endoscopic. This method is preferred by neurosurgeons. The operation is minimally traumatic and is performed under visual control. Complications are minimal and are not always detected. The outcome is favorable.
- Microneurosurgical operation.
- Shunting.
The last two types of surgical treatment are performed with mandatory craniotomy, which provides access to the brain.
Consequences
Any consequences are possible if the cyst grows rapidly or ruptures. That is why it is necessary to constantly monitor the condition of this formation and carry out timely therapy.
Consequences of the pathology:
- Impaired blood circulation and movement of cerebrospinal fluid.
- The appearance of tumors at the site of the cyst.
- Disorders of speech, movement, touch and vision.
- Patient death is extremely rare.
If the cyst bursts, quite dangerous complications arise:
- Blood poisoning (sepsis).
- The purulent contents of the cyst enter the cerebrospinal fluid, which leads to inflammation.
- Bleeding inside the skull.
- Complete paralysis.
- Death of the patient.
Forecast
The prognosis depends on the severity of the pathology. If a formation in the cerebellum is detected in the early stages of development before its growth accelerates, then the prognosis is favorable. In this case, patients are cured, complications and cyst ruptures are not observed.
A fatal outcome is possible if the pathology is diagnosed too late or if proper treatment and control are lacking. Rapid growth and rupture of education occur, and pathological changes in the corresponding psychological functions are observed.
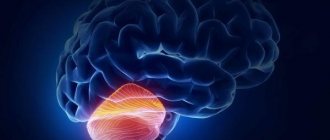
Symptoms of a cerebellar tumor - diagnosis and treatment
A large number of neoplasms of this part of the brain are known. Some of them can metastasize to the cerebellum, for example, in lung or breast cancer. Other types of tumors arise directly in this part of the brain, such as medulloblastoma and cerebellar astrocytoma. The following describes the symptoms of a cerebellar tumor, characteristic of various types of neoplasms.
Cerebellar astrocytoma
This type of disease develops from astrocytes located in this part of the brain. Cerebellar astrocytoma usually grows relatively slowly and rarely spreads to other areas. However, there are known cases of this type of tumor spreading to other parts. With this disease, symptoms usually include morning sickness and headache, which can last for weeks or months. Sometimes signs of cerebellar damage such as ataxia and dysdiadochokinesia are observed. Features of their manifestation can provide information about the specifics of the neoplasm and its location in this part of the brain. With this disease, the following signs of a neoplasm usually develop:
- headache, observed mainly at night and in the morning;
- nausea and vomiting;
- severe apathy;
- confusion and loss of orientation.
Sometimes this type of neoplasm is also accompanied by the following signs of a cerebellar tumor:
- numbness or weakness in the limbs;
- blurred, blurred or double vision;
- speech problems;
- memory loss;
- clouding of consciousness.
Medulloblastoma
Symptoms of a cerebellar tumor in young children may be mild and in some cases limited to behavioral changes, lethargy and an increase in head circumference. Sometimes irritability and indifference are observed. Vomiting may occur in infants, but it is more common in older children.
Sometimes patients with this malignancy have a prominent anterior fontanelle and dehiscence of the skull sutures on physical examination. In older children, lethargy may be accompanied by pathological head tilt, static ataxia and gait disturbance. Pathological tilt of the head means paralysis of the trochlear nerve or the approach of the tumor to the foramen magnum. Protrusion of the cerebellar tonsils into the foramen magnum due to pressure from the neoplasm can be life-threatening. Symptoms of a cerebellar tumor in this type of cancer depend on the location of the tumor, growth rate and size.
The progression of symptoms in medulloblastoma is characterized by rapid dynamics. For this reason, monitoring of symptoms before diagnosis is usually limited to two months. Manifestations of this type of neoplasm in children beyond infancy also include severe migraines and vomiting in the morning. This is due to increased intracranial pressure caused by blockage of cranial fluid caused by rapid tumor growth. With medulloblastoma, during the period preceding treatment, the symptoms of a cerebellar tumor intensify in the early stages.
In patients characterized by increased intracranial pressure, fundus examination often reveals papilledema. Palsy of the 4th or 6th cranial nerve is also sometimes observed, as well as complaints of diplopia caused by pressure from the tumor. Symptoms of a cerebellar tumor in older children may be due to swelling of the optic nerve, leading to blurred vision. However, severe visual impairment is usually not observed with this. Patients who have not yet been treated may occasionally present with speech impairment.
Medulloblastoma is most often seen in midline structures (eg, the midline cerebellum). In such cases, nystagmus, gait disturbance, and trunk ataxia are often observed. Sometimes manifestations of this disease include impaired writing and the development of clumsiness. Cerebellar tumor symptoms among adults with medulloblastoma are often characterized by unilateral presentation, such as dysmetria.
Brain hemangioblastoma
Hemangioblastoma is a fairly rare type of tumor noted for the blood vessels of the brain. Neoplasms of this type can develop in any part of the brain, but are most often present in the cerebellum and posterior cranial fossa. Although hemangioblastomas are benign tumors, if they are located near vital structures they can pose a serious threat and may be difficult to treat. This type of tumor usually comes into contact with the soft tissue surrounding the brain. Manifestations of this disease include:
- headache,
- gait disturbance,
- vomiting
- double vision,
- dizziness,
- decreased visual acuity,
- pain and discomfort in the neck,
- mental changes,
- noise in the head
- anorexia,
- lethargy
- weakness in the limbs,
- speech disorder,
- pain in the eyes,
- fainting states.
With this disease, the symptoms of a cerebellar tumor may increase sharply or gradually. They usually progress sharply in the event of a rapid increase in intracranial pressure or bleeding. The manifestation of this disease is mainly determined by the influence of tumor growth. Manifestations with this type of tumor sometimes include subarachnoid hemorrhage. Hemangioblastomas are rare in childhood, and among men they are observed 2 times more often. This disease is usually diagnosed in the age group of 20–40 years.
Dysplastic cerebellar gangliocytoma
This disease is a benign neoplasm caused by abnormal development of the cerebellar cortex. Patients suffer from migraines, dizziness, vomiting, nausea and macrocephaly. Sometimes symptoms of a cerebellar tumor in this disease include seizures, orthostatic hypotension, or subarachnoid hemorrhage. Patients with Cowden syndrome suffering from dysplastic cerebellar gangliocytoma are usually characterized by thyroid disease, meningiomas, oral papillomatosis, gastrointestinal polyps and other pathologies.
Preventive actions
Any unpleasant symptoms should not be ignored. Therefore, if the patient exhibits the above symptoms, it is necessary to seek advice from specialists (neurologist or neurosurgeon).
If a person is diagnosed with a cerebellar cyst, it is important to follow several recommendations that will help avoid complications:
- You need to visit your doctor periodically. This is necessary to monitor the patient’s condition and monitor the formation over time.
- Undergo diagnostic tests prescribed by a specialist.
- Carry out prevention against infectious diseases. You should increase the body's defenses: take vitamins, provide adequate nutrition, and healthy sleep.
- Prevent hypothermia of the body. A person should dress according to the season, avoid drafts, and keep his feet warm.
- Give up bad habits (drinking alcohol, smoking).
- It is necessary to monitor blood counts. If cholesterol or platelet levels increase, you should take medications prescribed by the doctor (prevention of blood clots, ischemia of brain tissue, and so on).
- Monitor blood pressure levels. If hypertension is observed, then constant medication is needed. This will help avoid strong pressure surges.
- If your health worsens, it is important to inform your doctor about it in order to adjust your treatment.