What does migraine with aura mean?
Migraine with aura is a disorder characterized by recurrent episodes of reversible local neurological symptoms (aura), usually increasing over 5-20 minutes and lasting no more than 60 minutes.
“Aura” is a term by which doctors mean the following:
- Visual impairment
. These can be lines, lights, spots, flickering. In severe cases, loss of vision. All manifestations are reversible. - Sensory perception disorders
. It seems that goosebumps are crawling all over the body, the person feels tingling, and there may be areas of numbness. All this is also reversible. - Speech disorders
, which also go away along with the attack.
In 73% of migraine attacks with aura, the headache begins not after the end of the aura, but during the aura itself and can be accompanied by other migraine symptoms - nausea (51%), photophobia (88%) and phonophobia (73%) i Morozova O.G. Migraine: new international criteria for diagnosis and principles of therapy based on evidence-based medicine and our own clinical experience / O.G. Morozova // International Neurological Journal. — 2021. — No. 3 (81). — pp. 131-138. . It happens that a panic migraine develops. Its complications are fear, anxiety, etc.
Migraines with and without aura are the same. A person usually feels a throbbing pain in one side of the head. Often it is concentrated in the eyeball. The pain intensifies with movement, sound and light stimuli. It can last from 4 hours to 3 days. At this time, it is impossible to lead a normal lifestyle. A person wants to be left alone in a dark and cool room, freeze, hide under the blanket. Typically, patients describe the pain as “bursting,” “splitting,” “about to burst,” “every sound like a hammer on the head.” And even after an attack, the consequences persist. The person is apathetic, tired and overwhelmed. It takes more than one day to recover.
Eye pain: is it a migraine?
Pain in the eyeballs is another symptom often referred to as ocular migraine. In fact, it can occur with various diseases, such as an acute attack of glaucoma, cluster headaches, sinus infections, etc.
In order to understand the real causes of eye pain during migraines, you need to visit a doctor and undergo an examination. Sometimes this symptom hides serious illnesses.
People who:
- over 50 years old;
- have never suffered from migraine attacks before;
- have chronic cardiovascular diseases.
The doctor deals with such patients especially carefully. It is imperative to exclude other, more dangerous possible causes: retinal detachment, blockage of the lumen of a vessel by a blood clot, pituitary tumor.
Symptoms of ocular migraine do not require treatment; as a rule, vision returns to normal within a few minutes. To prevent attacks, you need to avoid triggers - factors that usually provoke them. Your doctor may prescribe medications to relieve headaches.
Experienced doctors at the Neurology Center at the Medica24 International Clinic will examine you, prescribe an examination, reliably identify the causes of your symptoms and prescribe adequate treatment. You can make an appointment by phone. Call anytime.
The material was prepared by Natalya Yurievna, a neurologist at the international clinic Medica24, Candidate of Medical Sciences Lasch.
Differences from migraine without aura
Migraine without aura is called “classic”. Approximately 80% of patients suffer from it. A migraine without an aura manifests itself as throbbing pain at one point. It is not preceded by any visual, auditory or sensory impairment. Sometimes people don’t even realize that it’s a migraine, but think that they just have a headache. For this reason, patients do not go to the doctor, which is fraught with consequences.
You have migraine without aura if the following symptoms are present:
- 5 episodes of pain.
- The attacks last from 4 to 72 hours if you do not take medication.
- The pain throbs and is concentrated on one side of the head. The forehead, neck, and then the face or back of the head may hurt.
- With any physical activity the pain gets worse.
- There may be nausea, fear of light, sounds, voices.
What are the characteristics of migraine with aura?
About 20% of patients experience an aura. But only a few say that it occurs with every attack. The most common symptom of an aura is visual disturbances. Less commonly – sensory organ disorders (tingling, numbness, goosebumps). Aura symptoms are divided into positive and negative. In the first case, something is felt, and in the second, the fields of vision disappear or the hands go numb. Another property of the aura is dynamism. That is, a gradual increase in symptoms, and then their gradual decline. Usually the aura is replaced by a headache, but sometimes the aura appears on its own.
Migraine with aura is characterized by the following symptoms:
- Two episodes of migraine without aura.
- The presence of an aura for 1 hour or more before pain occurs. In this case, the following neurological symptoms appear - one or more:
- visual disturbances – photophobia, blinking, black spots in the field of vision, flickering arches, lines, zigzags, incorrect perception of objects in the field of vision;
- sound disorders, mainly intolerance to any sounds;
- speech problems;
- sensory disturbances – tingling, burning, numbness, etc.;
- impairment of motor abilities, such as sudden weakening of muscles on one side of the body.
Causes of migraine
The mechanisms of migraine development are not fully understood. A predisposing factor in the development of the disease is hereditarily determined dysfunction of vasomotor regulation. Approximately 70% of migraine patients have close relatives with a history of migraine-like headaches i Morozova O.G. Migraine: modern ideas about classification, diagnosis, therapy and prevention (part I) / O.G. Morozova // Emergency Medicine. - 2012. - No. 4 (43). — P. 32-41. .
There are two groups of factors that influence the course of migraine: those that worsen the course of migraine as a whole and those that provoke an attack.
Factors that worsen the course of migraine . In a patient with migraine, factors such as emotional stress, frequent consumption of alcoholic beverages, and other environmental influences can cause a long-term (over several months or years) worsening of the disease in the form of an increase in the frequency and/or intensity of attacks.
In patients with migraine, precipitating factors increase the likelihood of attacks; their effects usually appear within less than 48 hours. Despite the fact that migraine triggers have been well studied in a number of epidemiological studies (for example, the influence of menstruation i Koreshkina M.I. Modern aspects of diagnosis and treatment of migraine / M.I. Koreshkina // Neurology, neuropsychiatry, psychosomatics. - 2013. - P. 92-96.) and clinical (the effect of aspartame, chocolate, etc.) studies, in each individual case it is not always easy to establish a direct causal relationship between the provocateur and a migraine attack.
Factors provoking migraine paroxysms (migraine triggers) i Morozova O.G. Migraine: modern ideas about classification, diagnosis, therapy and prevention (part I) / O.G. Morozova // Emergency Medicine. - 2012. - No. 4 (43). — P. 32-41. :
- dietary: hunger, irregular nutrition, some foods (chocolate, cheese, nuts, alcohol (red wine), creams, yogurt, chicken liver, avocado, citrus fruits, bananas, concentrated soups, fried pork, sausages, pizza, coffee, cola, tea);
- hormonal: menstruation, ovulation, estrogen replacement therapy, oral contraceptives;
- psychological: emotional stress, anxiety,
- depression, fatigue;
- weather changes;
- exercise stress;
- lack or excess of night sleep;
- stuffiness, odors (smell of perfume);
- visual stimuli (flickering or bright light);
- cold;
- noise;
- staying on top.
Causes
Currently, the mechanism of migraine development is not well understood. Researchers have identified several phases in the pathogenesis of a migraine attack:
- Spasm of the cerebral arteries. Causes short-term hypoxia of the medulla, which is associated with the development of an aura.
- Subsequent dilation of cerebral vessels. Dilatation of the veins and arteries of the brain occurs unevenly after their previous narrowing, which determines the occurrence of throbbing pain.
- Swelling of the vascular walls. The swollen walls of the veins/arteries prevent the vessels from contracting back, which explains the duration of the headache.
- Recovery phase. At this stage, the swelling of the blood vessels subsides, their diameter returns to its original value, and the patient develops post-migraine syndrome, characterized by weakness, fatigue, and lethargy.
The exact causes of migraine pain have not been established, but a number of provoking factors have been identified:
- Nutritional factors. Consumption of certain foods and drinks (low alcohol, chocolate, etc.), eating disorders (skipping meals), poor nutrition or strict diets.
- Hormonal factors. The change in phases of the menstrual cycle occurs under the influence of certain hormones, in particular progesterone, so attacks often develop in women on the eve of menstruation, during the ovulatory phase, when using oral contraceptives and hormones for the treatment of gynecological diseases, in the postpartum and lactation periods, and in premenopause.
- Environmental factors. Radical climate change, big difference in time zones.
- External factors. Extraneous noises, loud sounds, flickering lights/flashes, bright artificial lighting, unpleasant, persistent or intense odors, smoking, including passive smoking.
- Factors associated with sleep disorders. Insomnia, lack of sleep or oversleeping (weekend migraine), late falling asleep and waking up, restless, interrupted sleep.
- Psychophysiological factors. Significant emotional stress at the end of a stressful situation (passing an exam, signing a contract), anxiety, prolonged tension, stress, excessive physical activity in sedentary people, nervous breakdowns. It is noted that the listed triggers often provoke attacks in people with ambitions and perfectionists.
- Medications. In addition to taking hormones, an attack can be caused by taking nitroglycerin, ranitidine, reserpine and a number of other drugs.
Types and symptoms of migraine auras
Let's look at the main types of auras and how they manifest themselves.
Visual or ophthalmological
This aura is called “classical”. With it, visual images appear - flashes of light, curved or straight lines, flickering objects, white or golden figures, spherical images, etc.
Symptoms develop over 5-30 minutes. Positive ones can be replaced by negative ones. The duration of the aura can reach 1 hour. The image usually appears in the center of the visual field. It gradually increases and moves to the periphery. A scotoma remains behind him
– dark, “blind” area. During the aura or within an hour after its appearance, pain occurs. When the attack ends, any disturbances go away without consequences.
Retinal
With such an aura, scotomas or blindness in one eye occur. Symptoms persist for up to 1 hour. The headache comes after scotomas in about an hour, but can also occur before them. This is a rare type of aura. There is an assumption that the symptoms appear due to spasm of the central retinal artery. In most patients, retinal migraine attacks alternate with migraine attacks with or without classic aura.
Auditory
Auditory auras are hallucinations with sound. Ringing in the ears may occur, and patients sometimes hear music or voices. Doctors associate this aura with epileptic activity in the cerebral cortex, in its temporal region.
Speech
It manifests itself as a speech disorder because it affects the speech centers of the brain. Before an attack of pain, for a few minutes, no more, it is difficult or impossible for a person to speak. He can rearrange syllables in words, letters, repeat the same thing. At the same time, the consciousness is absolutely pure.
Vestibular
This is an aura in the form of movement disorders - dizziness. A fairly common phenomenon that can be hidden or obvious. In the second case, a person “sicks” even with small loads. In the first, violations can only be detected within the framework of an examination. According to the ICD, 2 forms of vestibular migraine are distinguished:
- Basilar
- occurs rarely, mainly in teenage girls. The attack begins with visual disturbances, followed by dizziness, tinnitus, sensory disturbances, etc. Then, in 25% of cases, confusion occurs. Neurological symptoms persist for 20-30 minutes, then pain in the back of the head occurs. Without treatment, throbbing pain may persist for 2-3 days. - Paroxysmal dizziness of younger children
(benign). Occurs in children 1-4 years old. It manifests itself as short – from a few seconds to a few minutes – attacks of dizziness. The child loses stability, becomes anxious, and vomits. He may turn pale and sweat profusely. No headache. Attacks may recur over several months or years.
Vegetative
Often such auras are manifested by a feeling of heat, chills, cold, trembling; the face and neck may turn red or pale. Goosebumps may appear, and hairs may even rise on the skin. During an attack, the size of the pupil may change, and asymmetrically. Usually such an attack is part of a complex attack, and not an independent phenomenon.
Treatment
Migraine is a disease that responds poorly to therapy. Treatment is designed to eliminate the formation of attacks or alleviate the course of the migraine itself. The most common use of such drugs is:
- Analgesics and antidepressants;
- anticonvulsants;
- ergot medicines;
- serotonin agonists;
- calcium channel blockers.
Magnesium and other vitamins are used for systemic use. Despite this, no treatment can protect one hundred percent from the occurrence of migraine attacks, but with its help, the number of migraines is reduced and the general condition of the patient improves.
Diagnosis of migraine with aura
The diagnosis is made by a neurologist, and it is he who should be contacted with such a problem as soon as possible. The doctor must rule out cysts, tumors, encephalitis and vascular pathologies that cause similar symptoms. Therefore, a neurological examination, CT or MRI of the brain is performed, and the patient is sent for a consultation with an ophthalmologist for examination and determination of visual fields.
An EEG (electroencephalography) is required, which provides information about the functional activity and characteristics of the brain biorhythm of a particular patient. Based on the EEG results, the doctor then selects medications for therapy.
Diagnostics
In order to determine the disease and make a diagnosis of ocular migraine, it is necessary to contact not only a neurologist, but also an ophthalmologist. Ocular migraine symptoms are similar to some serious pathologies. In addition to collecting an anamnesis, you will need to conduct an examination of various parts of the eyes and assess the condition of the pupils. To exclude brain diseases, which the disorder often resembles, instrumental techniques are used to visualize brain structures. Most often, magnetic resonance imaging is indicated for this purpose.
When contacting an ophthalmologist, it is important to accurately characterize the visual changes that occur during an attack. To exclude the presence of eye pathologies, the following studies are carried out:
- external examination of the eyes, which allows us to exclude the presence of inflammation and injury;
- study of the reaction of the pupils to light and other irritations;
- assessment of eyeball mobility;
- assessment of the volume of the eyeballs;
- determination of the boundaries of the field of view;
- ophthalmoscopy;
- Ultrasound of eye vessels;
- general vision test.
After pathologies from the visual system are excluded, an examination is carried out aimed at identifying structural changes in the brain. To do this, the patient is given a referral for diagnostic procedures, which will be:
- magnetic resonance or computed tomography;
- X-ray of the head;
- electroencephalography.
Based on examination results, symptoms and medical history, the doctor makes a diagnosis and prescribes the necessary treatment.
Features of migraine manifestations in children and pregnant women
In childhood, the peculiarity of an attack is its short duration, from 30 minutes to several hours, and bilateral pain. It becomes one-sided in adolescence. Most often, children experience pain in the temples, forehead, and periorbital area. The nature of the pain is also not the same as in adults. The pain is squeezing, pounding, slightly throbbing. Children describe the latter extremely rarely.
It is difficult for a child to talk about his feelings, so the intensity of pain is assessed using VAS - a visual analogue scale with points from 0 to 10. Scales with emoticons can be used - from smiling to crying.
During pregnancy, migraines can occur even in those who have not previously suffered from them. In 25% of cases it is migraine with aura. It is much more difficult to tolerate, and there is almost nothing to eliminate the pain due to the delicate position. The approved drugs - No-Shpa, Citramon or Paracetamol - do not help. During pregnancy, aura most often manifests itself as photophobia, withdrawal, intolerance to sounds and strong odors, very severe nausea and the urge to vomit. The main causes of pain during pregnancy:
- consumption of “dangerous” foods – cheese, chocolate, citrus fruits;
- lack of water in the body;
- constant lack of sleep because the stomach makes it very uncomfortable to sleep;
- stress, frequent worries;
- large weight gain;
- violation of metabolic processes.
Migraine during pregnancy
Migraine is a hereditary disease that is expressed as a sharp pain sensation. The headaches are unbearably strong, they are too tough for ordinary pills, such as No-Shpa, Paracetamol, etc. Migraine in pregnant women is accompanied by certain factors called “auras”. This:
- Fearful attitude towards light.
- Intolerance to strong smells and loud sounds.
- Closed state.
- Unbearable nausea and even vomiting.
Very often, pregnant women accept all these symptoms as a normal malaise, and use Citramon, or apply a cool compress.
How to treat migraine with aura and how to relieve pain effectively and quickly
Since it is almost impossible to avoid an attack if there is a trigger, you need to know ways to improve the condition, because migraine is not a death sentence.
The final diagnosis is made by a neurologist. He will tell you what to do, how to treat the disease, how to increase the intervals between attacks.
Treatment for migraines is based on eliminating the pain and making it happen as little as possible or go away altogether. NSAIDs or specific medications, most often triptans, may be used. Intravenous infusion therapy is also used to treat migraines. The effectiveness of pain relief is directly proportional to the time of taking the drugs. You can stop an attack when it has just begun. Unfortunately, many people miss this moment with the thought “what if it doesn’t hurt.” However, at the peak of an attack, the tablets have almost no effect, because with migraine gastrostasis in the intestines, the absorption of any substances is very difficult.
Alternative ways to alleviate the condition are physical activity, exercise therapy, physiotherapy, and psychotherapy. Massage of the collar area is especially useful, because muscle spasm in this area can provoke an attack. Recently, migraines have been successfully treated with injections of botulinum toxin type A. The injections make remission last longer, and in some cases relieve pain for a very long time.
Treatment of migraines using traditional medicine
Many traditional medicine methods can provide relief from pain.
Ginger root
Ginger has the ability to block prostaglandins, thereby reducing the severity of pain. The same principle applies to most NSPVs. Ginger tea is prepared at home. Ginger root is crushed, then added to boiling water and simmered for 10 minutes over low heat. Next, the tea is filtered and drunk plain or with lemon and honey.
Chamomile
Has an anti-inflammatory and calming effect. You need to take two tablespoons of chamomile in a glass of water and cook the mixture for 5 minutes over low heat. Next, you need to strain the broth and drink it plain or with lemon and honey.
Lavender
Lavender oil is used for inhalation. The solution is prepared as follows: a teaspoon of oil is diluted in three glasses of boiling water. Breathe over the resulting solution for 15 minutes. Lavender oil can be mixed with peppermint oil and apply the mixture to the temples, gently massaging it a little. It is best to combine massage and inhalation.
What happens if migraine is left untreated?
Migraine is not a harmless disease. The disease is identified by the World Health Organization as a risk factor for cerebral strokes. Numerous epidemiological studies have revealed correlations between migraine and stroke, especially in young women suffering from migraine with aura i Ashina M. Vascular changes have a primary role im migraine / M. Ashina // Cephalalgia. - 2012. - 32. - 5. - P. 428-430. . Migraine is associated with a 16-fold increase in the risk of stroke in pregnancy and the overall risk of cardiovascular events in women. Migraine can be a risk factor not only for stroke, but also for “silent” heart attacks and damage to the white matter of the brain. These changes most often occur in women suffering from migraine with aura, and are associated with severe and frequent migraine attacks i Hadjikhani N. Mechanism of migraine aura revealed by functional MRI in the visual cortex / N. Hadjikhani // Proc. Natl. Acad. Sci USA. - 2001. - 98. - P. 4687-4692. .
You shouldn’t treat the attacks as “survived and are fine”, you need to see a doctor and get treatment.
MIGRAINE IN WOMEN (the role of sex hormones)
The newsletter was prepared by the Secretary of the AGE, Ph.D. L.M. Ilina based on articles by T.G. Voznesenskaya (RMJ, 1999), O.V. Vorobyova (RMJ. Neurology, 2004), T. Vincent et al. (Headache, 2006;46 (1 and 3), L. Brookes (Medscape Cardiology, 2006;10 (2), etc.
MIGRAINE IN WOMEN (the role of sex hormones)
Migraine is one of the most common types of headaches. In women, migraine occurs three times more often (in approximately 27% of women during reproductive age) than in men, and exceeds the incidence of diseases such as diabetes, osteoarthritis and bronchial asthma. In more than 50% of women, the disease occurs for the first time before the age of 20, often during puberty. As a rule, visits to doctors for migraine increases at 20-25 years of age and remains at this level until approximately 40 years of age. The frequency and nature of manifestations of the disease are significantly influenced by hormonal changes that occur in the dynamics of the menstrual cycle, during pregnancy, perimenopause, when taking combined oral contraceptives (COCs) and hormone replacement therapy (HRT). In addition to a sharp decrease in quality of life, migraine has an important medical and social significance, since in women suffering from certain forms of it, after the age of 45, the risk of ischemic stroke increases.
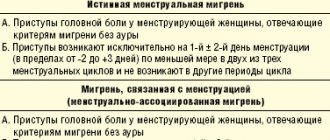
Classification. Migraine with aura (classic migraine) is less common (in approximately 20% of all migraine patients) than migraine without aura (simple migraine). In most patients, the aura that precedes an attack of headache and lasts from 5 to 20 minutes is visual and manifests itself in the form of flashes of light, blind spots (scotomas) or hemianopsia (loss of one of the two fields of vision). Less commonly observed are transient neurological symptoms such as paresthesia, numbness of the tongue, cognitive impairment (usually aphasia), panic disorders (“panic” migraine), etc. Menstrual migraine. According to the International Headache Society, menstrual migraine (MM) is migraine without aura and is divided into two subgroups. 1. “true MM” - headache attacks occur exclusively on perimenstrual days (2 days before menstruation and the first three days after its onset); 2. “migraine associated with menstruation” - in 2/3 of menstrual cycles, headache attacks occur on perimenstrual days, but can also occur on the remaining days of the cycle. In the population, MM occurs in approximately 3% of cases, but among women suffering from migraine, this percentage is much higher: according to various sources, migraine associated with menstruation - in 35% - 51% of cases, and true MM - in 7% - 19% of cases .
Etiopathogenesis. It has been shown that vascular, nervous and endocrine-humoral mechanisms are involved in the genesis of a migraine attack. Most authors point to a hereditary predisposition to this disease, since 50-60% of patients had parents who suffered from true migraine or various forms of autonomic-vascular disorders. Central neurovascular dysregulation manifests itself in the development of endothelial dysfunction, disruption of the metabolism of the most important brain monoamines (especially serotonin) and the endogenous opioid system, etc. Sex hormones have a pronounced modulating effect on these mechanisms. MM appears to result from an “inappropriate” CNS response to “normal” changes in sex hormone levels, as there were no differences in absolute sex hormone levels compared to women with non-menstrual cycle migraine. In a number of studies carried out back in the 70s of the last century, it was convincingly shown that it is the decrease in estrogen levels in the late luteal phase (less than 45-50 pg/ml) that is the initial link in the chain of other neurohumoral changes and plays the role of a triggering factor for an attack MM. Intramuscular administration of estrogens (but not progesterone) immediately before the onset of menstruation, as well as the administration of estrogens in the form of a patch or gel on perimenstrual days, stops an attack of MM. For most women, the course of migraine improves in the second and third trimesters of pregnancy, as well as with increasing duration of postmenopause. However, with migraine with aura, some women may experience an increase in the frequency and severity of headache attacks during pregnancy, which is characterized by high, stable levels of estrogen, as well as when using COCs containing the highly active synthetic estrogen ethinyl estradiol. Thus, with moderate and high estrogen levels, the frequency of migraine attacks without aura may decrease and, conversely, the course of migraine with aura may worsen. The trigger mechanisms for the two migraine subtypes appear to be different. Of course, a sharp decrease in estrogen levels is not the only pathogenetic link in MM. It is known that the level of prostaglandins (PG) in the endometrium increases 3 times by the end of the luteal phase of the cycle (the maximum concentration is observed in the first 48 hours of menstruation). The entry of a significant amount of PG into the general bloodstream during this period can initiate, in addition to headaches and pain in the lower abdomen, nausea, vomiting and other symptoms. Some researchers believe that low magnesium levels may also play a role as a precipitating factor, since magnesium ions are involved in the functioning of cerebral vessels and the central nervous system, due to the release of the most important vasodilator of nitric oxide, serotonin, as well as inhibiting the passage of calcium ions through membrane channels, in addition, they are cofactors for many essential enzymes. There is evidence of relief of an attack of MM when magnesium supplements are prescribed 15 days before the expected menstruation. It is believed that a decrease in the level of sex hormones during the perimenstrual period (late luteal and early follicular phases), which contributes to an increase in the activity of the “excitatory” neurotransmitter glutamate and, conversely, a decrease in opioid, GABAergic and serotonergic tone, as well as an increase in the concentration of PG and magnesium deficiency play a major role in the pathogenetic mechanisms of MM and increase the body’s sensitivity to the effects of provoking factors. The appearance of migraine with menarche, the presence of MM and premenstrual syndrome during reproductive age, and the development of pronounced vasomotor symptoms in peri- and postmenopause indicate an increased “sensitivity” of such women to changes in the level of sex hormones.
MANAGEMENT OF PATIENTS WITH MIGRAINE Lifestyle changes: regular, adequate sleep (both insufficient and excess sleep must be avoided); regular meals, eliminating or reducing the consumption of foods containing tyramine (chocolate, cocoa, nuts, citrus fruits, beans, tomatoes, celery and cheeses), alcoholic beverages (including dry wine, especially red, champagne, beer) regular exercise (swimming , skiing, walking, cycling), which should be fun. It must be remembered that a good mood, positive emotions, the ability to relax and resist stress prevents the development of migraine attacks.
Drug treatment. Migraine treatment is divided into two parts: 1. relief of an already begun migraine attack; 2. preventive measures during the interictal period. 1. In most patients with migraine, treatment is limited to stopping attacks. It should be noted that attacks of MM are more difficult to treat than those not associated with the menstrual cycle. When choosing a specific dosage form to relieve a migraine attack, it is advisable to start with simple or combined analgesics, as well as non-steroidal anti-inflammatory drugs (ibuprofen, paracetamol, metamizole, etc.). The latter have a local (inhibition of pain mediators at the level of the endings of sensory nerves) and a central effect, inhibiting the enzyme cyclooxygenase, they inhibit the synthesis of PG in the central neuronal synapses involved in the transmission of nociceptive (pain) impulses. For MM, non-steroidal anti-inflammatory drugs are prescribed 2-3 days before the expected menstruation + all menstrual days. Such therapy can be classified as preventive, while the powerful local effect of these drugs at the local level also helps to relieve dysmenorrhea and reduce blood loss. If there is no effect from the above drugs, you should proceed to the prescription of ergotamine drugs (dihydroergotamine, dihydroergotamine mesylate). The initial dose is 1-2 mg of ergotamine, if necessary, the dose can be repeated after 30 minutes, the total dose should not exceed 5 mg per attack or 10 mg per week. The effectiveness of ergotamine drugs is higher when using parenteral agents (rectal suppositories, nasal spray). It should be remembered that diseases such as coronary heart disease, arterial hypertension and peripheral vascular disease are contraindications for the use of these drugs. In severe cases, a headache specialist prescribes selective serotonin agonists: sumatriptan at a dose of 50 mg (no more than 3 tablets per day with an interval of at least an hour); naratriptan in a dose of 2.5 mg, in the absence of effect, the subsequent dose is used no earlier than 4 hours later, the maximum daily dose is 5 mg, for the prevention of MM - in a dose of 2.5 mg 1 time per day on perimenstrual days. It should be emphasized that the need for frequent use of these potent drugs indicates incorrectly selected preventive therapy. 2. Preventive treatment is prescribed only for frequent and severe migraine attacks or in the presence of comorbid psychopathological syndromes (anxiety, depression, etc.). As a rule, the minimum effective doses of drugs are selected, which in the case of MM can be increased on perimenstrual days. Pharmacotherapy in the interictal period includes: beta-blockers, calcium channel blockers, psychotropic drugs (lerivon, fluoxetine, coaxil citalopram, etc.), as well as atypical benzodiazepine tranquilizers (clonazepam, alprazolam). The prescription of psychotropic drugs is especially effective for so-called “panic” migraines. Preventive treatment with antidepressants should be carried out for at least 1.5 months, and optimally within 2-3 months, taking into account that the clinical effect, as a rule, develops no earlier than 2 weeks from the start of treatment. For migraine with aura, courses of vasoactive drugs (Trental, Sermion, Vasobral, etc.) in generally accepted dosages are recommended. When prescribing preventive treatment for older women, lower doses of drugs are used.
Hormonal treatment of menstrual migraine Only if there is no effect from non-hormonal therapy, you can move on to hormonal treatment of migraine, the essence of which is to prevent a sharp decrease in estrogen levels in the late luteal phase. In women with a regular ovulatory cycle, 2-3 days before the expected menstruation, you can use a kind of “add-back therapy” and select one of the transdermal forms of estrogens - one Klimara patch, designed for a week and releasing 0.05 mg of estradiol per day, or gels with estradiol: Divigel (0.5 mg estradiol per day) or Estrogel (0.75 mg estradiol per day) daily for 7 days. During a normal ovulatory cycle, endogenous progesterone is sufficient to neutralize the possible proliferative effects of such a small dose of estrogen. Of course, this treatment method is not used in women who have contraindications for hormonal therapy. In a number of women, headache attacks occur during a 7-day break when taking even microdose COCs, since a shift in estrogen levels can exceed the permissible “threshold” in “sensitive” women and provoke an attack. In such cases, you can use: 1. prolonged cycles of COCs - continuously for 2-4 months with a 7-day break; 2. transdermal estrogens (see above), which “smooth out” approximately half the shift in estrogen levels on the days of COC withdrawal.
Risk of strokes in migraine with aura (choice of contraceptive method). According to various data, the use of COCs increases the risk of ischemic strokes in women with migraine with aura by 5 to 17 times (the more significant, the higher the dose of ethinyl estradiol), in women who smoke - by 34 times. Given the important role of the vascular component in the genesis of migraine, the selection of a contraceptive method in women with migraines requires taking into account several factors. Taking into account the low absolute risk of ischemic stroke in women under 45 years of age (5-10 cases per 100,000 women/years), as well as the low incidence of this kind of complications when using microdose COCs (ethinyl estradiol content no more than 20 mcg) during reproductive age, migraine without aura in young, healthy and non-smoking women is not a contraindication for their use. However, women suffering from migraine with aura should choose another method of contraception (mini-pill, Mirena IUD, etc.). It should be remembered that unfavorable heredity (early heart attacks and strokes in first-degree relatives), as well as the presence of spontaneous miscarriages, premature birth, fetal malnutrition, severe gestosis, thromboembolism in the anamnesis, may indicate possible disorders of the hemostatic system (factor V Leiden, increased prothrombin level, etc.) in a given woman.
Migraine and menopause (effect of HRT). The influence of menopause on the clinical course of migraine varies significantly according to different data: in 8-36% its course improves, in 9-42% it worsens, in 27-64% it remains unchanged. In 8-13% of cases, migraine attacks can occur de novo, usually with the onset of severe menopausal disorders, apparently due to the commonality of some pathogenetic mechanisms. Ovariectomy, especially performed in women of reproductive age, always contributes to exacerbation of the disease or the development of migraine attacks (in 38-87% of cases) due to a sharp decrease in estrogen levels. If it is necessary to prescribe HRT to relieve severe climacteric disorders and increased manifestations of migraine against the background of switching off ovarian function, HRT can be effective, especially if the migraine attacks were not associated with the menstrual cycle. However, in women who suffered from MM during reproductive age, when oral forms of HRT are prescribed in a cyclic regimen, the course of migraine may worsen (usually from the third month of therapy, an increase in the frequency and duration of attacks, as well as the number of analgesics used). In such cases, it is preferable: 1. to use transdermal forms of drugs (see above), in which an adequate level of estrogen is achieved with minimal fluctuations in hormones in the blood during the day. In women with an intact uterus, treatment regimens with the addition of natural progestogens in a cyclic mode (utrozhestan and dydrogesterone) are used; 2. switch as quickly as possible from a cyclic to a continuous regimen of therapy with low-dose drugs (Femoston, 1/5). In women with a tendency to fluid retention and hypertension, preference should be given to the drug Angelique, which contains 1 mg of estradiol, and as a progestogen component, drospirenone, a spironolactone derivative with antialdosterone and antiandrogenic activity. As when prescribing COCs, special caution when prescribing HRT should be observed in women who smoke with migraines, have risk factors for ischemic stroke, as well as unfavorable heredity, as mentioned above. In women suffering from migraine with aura, if there are significant indications for HRT (severe menopausal syndrome, osteoporosis), it is advisable to prescribe only parenteral forms of not only estrogens, but also progestogens (Mirena, patches, gels, vaginal suppositories). The patient should be warned about the need to urgently consult a doctor if migraine attacks become more frequent and/or the nature of clinical manifestations changes (the appearance of neurological symptoms, for example, an aura before a headache attack).
Migraine prevention
Prevention involves taking the medicine daily for a certain period of time. Which one is prescribed by a neurologist individually. This medicine will act not on the symptoms, but on the cause of the disease, preventing attacks from developing. However, drug prevention is not indicated for everyone. It is prescribed if:
- number of attacks – up to 8 per month or 2 per week;
- Even specific anti-migraine medications - Zomig, Relpax and other triptans - hardly help the patient;
- Triptans and analgesics cannot be taken due to contraindications;
- The patient has hemiplegic migraine, a rare hereditary disease that leads to stroke.
Migraine during pregnancy. How to treat?
Anti-migraine medications should be used with great caution and only after consulting a doctor. During pregnancy, a woman's body can react differently to one drug or another, so you need to be extremely careful about what you take. Only qualified doctors can determine what is possible for migraines during pregnancy, since they have the necessary knowledge and practice.
Having figured out what kind of phenomenon migraine is in pregnant women and how to treat it, a few words need to be said about prevention. It is best to build a daily routine and stick to it, yoga for pregnant women will not harm anyone to keep your body in good physical condition. A head and neck massage will be helpful, and most importantly, eat what your body requires and drink plenty of water.
Clinical Brain Institute Rating: 3/5 — 7 votes
Share article on social networks
Migraine classification ICD-10
Migraine is coded G43: Diseases of the nervous system => Episodic and paroxysmal disorders => Migraine.
| Code | Disease |
| G43.0 | Migraine without aura (simple) |
| G43.1 | Migraine with aura (classic) |
| G43.2 | Migrainous status |
| G43.3 | Complicated migraine |
| G43.8 | Other migraine |
| G43.9 | Migraine, unspecified |
Sources:
- Ashina M. Vascular changes have a primary role in migraine / M. Ashina // Cephalalgia. - 2012. - 32. - 5. - P. 428-430.
- Hadjikhani N. Mechanism of migraine aura revealed by functional MRI in the visual cortex / N. Hadjikhani // Proc. Natl. Acad. Sci USA. - 2001. - 98. - P. 4687-4692.
- Esin O.R. Migraine: Basic principles of treatment and prevention / O.R. Esin [et al.] // Clinician. - 2011. - No. 4. - P. 10-16.
- Koreshkina M.I. Modern aspects of diagnosis and treatment of migraine / M.I. Koreshkina // Neurology, neuropsychiatry, psychosomatics. - 2013. - pp. 92-96.
- Morozova O.G. Migraine: new international criteria for diagnosis and principles of therapy based on evidence-based medicine and our own clinical experience / O.G. Morozova // International Neurological Journal. — 2021. — No. 3 (81). — pp. 131-138.
- Morozova O.G. Migraine: modern ideas about classification, diagnosis, therapy and prevention (part I) / O.G. Morozova // Emergency Medicine. - 2012. - No. 4 (43). — P. 32-41.