Toxoplasmosis on MRI of the brain Magnetic resonance imaging is a painless and informative way to study the brain. Layer-by-layer MR scanning allows you to examine in detail all parts of the organ and evaluate their structure. Using certain sequences, it is possible to study in detail the white and gray matter, blood vessels, and ventricular system.
MRI is considered an effective method for identifying focal brain lesions. These include limited areas with a disturbed structure inside the substance of the organ. Such changes are often accompanied by mass effect, swelling, and deformation of the surrounding areas. Lesions in the brain on MRI appear as areas of change in the MR signal. Based on specific features, location, size and degree of influence on surrounding structures, the radiologist can make assumptions about the nature of the pathology. Using the information listed, the doctor makes a diagnosis, makes a prognosis for the patient and selects treatment.
Lesions on MRI of the brain: what does it mean?
The result of magnetic resonance imaging is a series of layer-by-layer images of the area under study. In the images, healthy tissue appears as alternating light and dark areas, depending on the concentration of fluid in it and the pulse sequence used. Based on the sections, the radiologist evaluates:
- development and position of individual structures;
- compliance of the MR signal intensity with the norm;
- condition of the gyri and grooves;
- size and structure of the ventricular system and subarachnoid space;
- parameters of the ear canals, orbits, accessory sinuses;
- structure of the vascular bed;
- structure of cranial nerves and cerebral membranes;
- the presence of signs of pathology (focal changes, swelling, inflammation, damage to the walls of arteries and veins).
Lipoma of the quadrigeminal cistern on MRI (circled)
MRI is prescribed if the patient has neurological abnormalities due to damage to brain tissue. Symptoms may include:
- headache;
- impaired coordination of movements;
- dysfunction of the organs of hearing or vision;
- disturbances in concentration;
- memory disorders;
- sleep problems;
- psychoemotional disorders;
- paresis/paralysis of the limbs and/or facial muscles;
- sensory disorders;
- seizures, etc.
Magnetic resonance imaging of the head allows the doctor to accurately determine the location of focal changes and find out the nature of the patient’s poor health. At the Magnit DC, specialists are armed with the latest MR scanning devices, which allow them to conduct research with high reliability.
Classification of the disease
In modern medicine, it is customary to distinguish the following types of insufficient blood supply to the brain:
- Binswanger's disease. This type of vascular circulation disorder leads to insufficient blood supply to the white matter of the brain. With this disease, the destruction of neurons occurs, which will soon lead to senile dementia - dementia. The first alarming symptom is severe pressure drops within one day. Then memory begins to deteriorate greatly.
- Pathological processes in the great vessels. Such disorders include narrowing of the lumens, strong bends, and thrombosis of blood vessels, which lead to a lack of circulating blood.
- Consequences of micro-strokes. When small vessels are blocked, there is a clear deterioration in the nutrition of the gray or white matter of the brain. This process cannot happen for a person without consequences. The patient may experience both general signs of the disease and disruptions only in certain body functions.
Types of lesions on MRI of the head
The color of the resulting image of normal brain structures and pathological changes depends on the program used. When scanning in angio mode, including using contrast, a branched network of arteries and veins appears on the images. Focal changes are of several types; based on their characteristics, the doctor can guess the nature of the foci.
With pathology of the medulla, the properties of the affected foci are disrupted, which is manifested by a sharp change in the MR signal compared to healthy areas. The use of certain sequences (diffusion-weighted, FLAIR, etc.) or contrast allows for more clear visualization of local changes. That is, if a radiologist sees a single lesion on the MRI results, different scanning modes or contrast will be used to study it in more detail.
When comparing changes with healthy areas of the brain, hyper-, hypo- and isointense zones are identified (bright, dark, and the same color as adjacent structures, respectively).
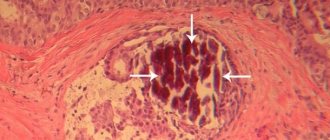
Brain abscess on MRI (indicated by arrow)
Hyperintense lesions
Identification of hyperintense, i.e. foci that clearly stand out on MR scans makes the specialist suspect a brain tumor, including of metastatic origin, hematoma (at a certain moment from the onset of hemorrhage), ischemia, edema, vascular pathologies (cavernomas, arteriovenous malformations, etc.), abscesses , metabolic disorders, etc.
Brain tumor on MRI (indicated by arrow)
Subcortical lesions
Damage to the white matter of the brain is usually characterized as changes in subcortical structures. Subcortical lesions identified by MRI indicate that the damage is localized just under the cortex. If multiple juxtacortical lesions are detected, it makes sense to suspect a demyelinating process (eg, multiple sclerosis). With this pathology, destructive changes occur in various areas of the white matter, including directly under the cerebral cortex. Periventricular and lacunar lesions are usually detected during ischemic processes.
Foci of gliosis
When brain tissue is damaged, compensatory mechanisms are activated. Destroyed cells are replaced by glial structures. The latter ensures the transmission of nerve impulses and is involved in metabolic processes. Due to the structures described, the brain recovers from injuries.
Identification of glial foci indicates previous destruction of the cerebral substance due to:
- birth trauma;
- hypoxic processes;
- hereditary pathologies;
- hypertension;
- epilepsy;
- encephalitis;
- intoxication of the body;
- sclerotic changes, etc.
By the number and size of altered areas, one can judge the extent of brain damage. Dynamic observation allows you to assess the rate of progression of the pathology. However, by studying the zones of gliosis, it is impossible to accurately determine the cause of the destruction of nerve cells.
Foci of demyelination
Some diseases of the nervous system are accompanied by damage to the glial membrane of the long processes of neurons. As a result of pathological changes, the conduction of impulses is disrupted. This condition is accompanied by neurological symptoms of varying degrees of intensity. Demyelination of nerve fibers can be caused by:
- multifocal leukoencephalopathy;
- multiple sclerosis;
- dissimulating encephalomyelitis;
- Marburg's disease, Devic's disease and many others.
Typically, demyelination lesions appear as multiple small areas of hyperintense MR signal located in one or more parts of the brain. Based on the degree of their prevalence, duration and simultaneity of occurrence, the doctor judges the scale of development of the disease.
Focus of demyelination on MRI
Focus of vascular origin
Cerebrovascular insufficiency causes ischemia of the cerebral substance, which leads to changes in the structure and loss of function of the latter. Early diagnosis of vascular pathologies can prevent stroke. Focal changes of discirculatory origin are found in most patients over 50 years of age. Subsequently, such zones can cause degenerative processes in the brain tissue.
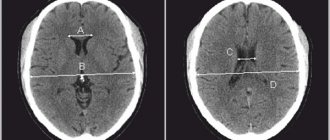
Lacunar cerebral infarction on MRI (indicated by arrow)
Cerebral circulation disorders can be suspected by focal changes in the perivascular Virchow-Robin spaces. The latter are small cavities around the cerebral vessels, filled with fluid, through which tissue trophism and immunoregulatory processes occur (blood-brain barrier). The appearance of a hyperintense MR signal indicates expansion of the perivascular spaces, since they are normally not visible.
Sometimes an MRI of the brain reveals multiple lesions in the frontal lobe or in the deep parts of the hemispheres, which may indicate damage to the cerebral vessels. The situation is often clarified by MR scanning in angio mode.
Foci of ischemia on MRI
Foci of ischemia
Cerebral circulation disorders lead to oxygen starvation of tissues, which can provoke necrosis (infarction). Ischemic lesions on T2-weighted sequences appear as areas with moderately hyperintense signal of irregular shape. At a later stage, when performing MRI in T2 VI or FLAIR mode, a single lesion takes on the appearance of a light spot, which indicates a worsening of destructive processes.
Gliosis: causes and mechanisms of development
Glial tissue is one of three types of brain tissue (along with neuronal and ependymal), which is essentially connective tissue; normally it makes up about 40% of the brain volume.
Its function is to preserve the very structure of the brain, ensure the supply of nutrients to the main cells of the brain - neurons, as well as physically protect neurons and give them a certain position. As neurons die from natural or pathological causes, they are replaced by glial tissue. Gliosis is the pathological proliferation of glial tissue, the appearance of large single or multiple foci of connective tissue (they look like scars) in the structures of the brain. Gliosis cells, although they replace dead neuron cells, cannot fully perform their functions, therefore, as a result of a lack of mechanisms for transmitting nerve impulses, neurological symptoms develop. The appearance of gliosis foci leads to disruption of the normal functioning of the brain - the patient’s attention and memory weaken, mental processes are disrupted, speech and movements become uncertain.
Such disorders are inevitable as a result of the natural aging of the body, but there are cases of premature pathological growth of glial foci in the brain structures of young and middle-aged people. In extremely rare cases, a person may experience congenital replacement of neurons with glial cells.
The nature of the occurrence of gliosis changes in the brain can be different. Brain diseases such as epilepsy, encephalitis, multiple sclerosis can lead to accelerated death of neurons and proliferation of connective tissue; vascular disorders, hypertension, anemia, trauma and cerebral edema can also cause gliosis. Provoking factors are: heredity, old age, excessive consumption of fatty foods and poor lifestyle in general.
What do white and black spots mean on MRI images?
Zones of altered MR signal may indicate:
- tissue ischemia;
- edema;
- necrosis;
- purulent melting;
- tumor transformation;
- metastatic lesion;
- gliosis;
- demyelination;
- degeneration, etc.
The radiologist describes the signal intensity, size and location of the lesion. Taking into account the information received, the patient’s complaints and data from previous examinations, the specialist can assume the nature of the pathological changes.
Acute disseminated encephalomyelitis on MRI
Reasons for development
The direct causes of the development of meningiomas have not been reliably studied to date. However, there are a number of factors that can provoke their occurrence:
- Most often, brain meningioma is diagnosed in mature patients, after 40 years;
- It is known that women are more susceptible to developing brain meningioma than men. This is due to the fact that tumor growth is greatly influenced by female sex hormones;
- the occurrence of various tumors in the brain is often associated with high doses of ionizing radiation;
- the influence of such negative factors as chemicals and toxic substances, trauma, exposure to a mobile phone and others;
- A significant role in the development of meningioma belongs to genetic diseases, one of which is neurofibromatosis type 2, which causes multiple malignant meningiomas.
Treatment
Meningioma very often causes the development of edema of surrounding tissues, which affects the appearance of various negative symptoms. Steroid drugs are prescribed to relieve swelling. Treatment for meningioma depends on the type and size of the tumor, its location, the patient's health and age.
According to medical statistics, in 90% of cases, brain meningiomas are benign tumors, which are characterized by slow development and the absence of concomitant damage to vital organs.
Malignant tumors are characterized by rapid growth and the presence of metastases in any other organs of the human body.
Tumor removal
Removal of meningioma is not always carried out. Most often, a benign tumor is monitored. Surgery is required if the meningioma is malignant and increases in size.
The main treatment method for growing benign and malignant tumors is surgery to remove brain meningioma. It is very important to perform competent removal of the tumor. The consequences of incorrect surgical intervention, which damaged the surrounding brain tissue or venous sinuses, can be very dire. Such an operation can cause a significant decrease in the patient’s quality of life, so neurosurgeons often leave part of the cancerous tissue, constantly monitoring its growth.
Malignant meningiomas tend to recur, requiring repeated surgery.
Make an appointment
Consequences of the operation
Depending on the location of the tumor and its size, complications may develop after the operation: deterioration or loss of vision, partial or complete memory loss, paresis of the limbs, impaired concentration, changes in character, personality, cerebral edema, bleeding.
Radiation therapy
Treatment of brain meningioma without surgery involves the use of radiation therapy methods, which are used when it is not possible to effectively remove the tumor surgically. Pathological cells are destroyed under the influence of high doses of X-ray radiation. The use of standard radiation therapy is inappropriate for the treatment of patients diagnosed with large cerebral meningioma. However, treatment without surgery in such cases is ineffective.
When the tumor is localized in a place that is difficult for a neurosurgeon to reach, or when there are areas close to it, damage to which can lead to disruption of vital functions, specialists at the Yusupov Hospital give preference to stereotactic methods. This type of therapy can be used to treat large tumors. Stereotactic radiosurgery is based on targeted irradiation of a tumor formation with beams located at different angles.
Often, the stereotactic method is combined with surgical treatment - if there are contraindications for removing tumors in the usual way.
Chemotherapy is not used to treat benign brain meningiomas.