Causes of arachnoiditis
In most patients with arachnoiditis, the predisposing factor is infectious diseases. In particular, these diseases include chickenpox, influenza, measles, viral meningitis, cytomegalovirus infection, and meningoencephalitis. The disease can also be provoked by chronic intoxication of the body, inflammatory diseases of the paranasal sinuses, and trauma. Arachnoiditis is often diagnosed in patients who experience reactive inflammation of a growing tumor.
Pathology can also occur due to acute or chronic purulent otitis media. In this case, inflammation is provoked by toxins and low-virulent microbes. Researchers also include various complications of purulent otitis (petrositis, labyrinthitis, sinus thrombosis), brain abscess, purulent meningitis and otogenic encephalitis as the causes of the disease.
In neurology, there are also a number of factors that are considered predisposing to the occurrence of the disease. Such factors include intoxication (for example, alcohol), frequent viral diseases, chronic overwork, hard work in an unfavorable climate, and frequent injuries. In 10% of all cases of the disease, it is impossible to establish the exact etiology.
Pathogenesis of arachnoiditis
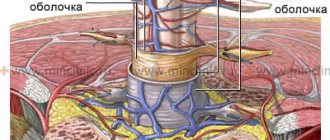
To understand the nature of the disease, it is necessary to become familiar with the anatomical features of the brain. The arachnoid membrane, which is affected by inflammation during arachnoiditis, is located between the soft and dura mater. Moreover, it is not fused with them, but simply fits tightly. Unlike the pia mater, the arachnoid membrane does not penetrate the cerebral convolutions. Small spaces filled with cerebrospinal fluid are formed under it.
All these spaces connect to the fourth ventricle. Through these spaces there is an outflow of cerebrospinal fluid from the cranial cavity. The mechanism of occurrence of arachnoiditis is as follows: due to the influence of various causes and provoking factors, the body activates the production of antibodies to the arachnoid membrane, which then provokes its inflammation. In patients with arachnoiditis, there is clouding and noticeable thickening of the arachnoid membrane, as well as the appearance of cystic expansions and connective tissue adhesions in it.
Classification of arachnoiditis
- Arachnoiditis of the meninges
- Optico-chiasmatic arachnoiditis
- Arachnoiditis of the posterior cranial fossa
- Arachnoiditis of the spinal cord membranes
This type of disease is also called cerebral. Cerebral arachnoiditis is localized in the posterior cranial fossa, on the convex surface of the brain and its base. The clinical picture of this disease is characterized by regular headaches and impaired circulation of the cerebrospinal fluid. In the most severe cases, the disease is accompanied by convulsive seizures, which can even lead to status epilepticus.
Arachnoiditis of the brain is often located in the central gyri and anterior parts of the cerebral hemisphere. Due to the resulting pressure on the sensory and motor centers, the patient may experience sensitivity and movement disorders. If the cerebral cortex is compressed or a cyst forms in it due to arachnoiditis, the patient may experience epileptic seizures.
This type of arachnoiditis is localized mainly in the chiasmal region. Frequent causes of this form of arachnoiditis are tonsillitis, malaria, syphilis, infectious diseases of the paranasal sinuses, and traumatic brain injuries. This type of arachnoiditis is characterized by the formation of adhesions in the area of the intracranial part of the optic nerves and the chiasm. In the most difficult cases, a scar may form around the chiasm.
As a rule, the disease provokes vision problems in the patient. In this case, the degree of decrease in the patient’s vision can vary from its minimal decrease to blindness. In most cases of optochiasmatic arachnoiditis, patients experience optic nerve atrophy. Visual symptoms are often severe, while hypertension symptoms are moderate.
It is the most common type of cerebral arachnoiditis. The severity of the symptoms of the disease depends on the location and nature of the inflammatory process, as well as its combination with hydrocephalus. The formation of cysts and adhesions usually leads to the closure of the openings of the cerebral ventricles, which provokes an increase in intracranial pressure. If intracranial pressure does not increase and is normal, the disease can last a long time.
The acute form of the pathology is characterized by all the symptoms of high intracranial pressure: nausea, dizziness, vomiting, bradycardia, severe headache localized in the back of the head. With a less acute course of the disease, signs of damage to the posterior cranial fossa become most pronounced. Patients may also experience symptoms such as unsteady gait and spontaneous nystagmus.
This is a spinal form of arachnoiditis, which occurs mainly due to purulent abscesses and furunculosis. Symptoms of the disease are similar to those of an extramedullary tumor: patients experience motor and sensory disorders, as well as radicular syndrome (limited mobility, parasthesia, trophic changes, pain in the heart, lower back and stomach, neck and limbs).
Spinal arachnoiditis is localized mainly at the level of the lumbar and thoracic segments, as well as on the posterior surface of the spinal cord. Typically, arachnoiditis of the spinal cord membranes is chronic.
- Anamnestic information: 1) etiological risk factors; 2) development gradually, gradually. At first, often astheno-neurotic symptoms, irritative (epileptic seizures), then hypertensive (headache, etc.). Gradual deterioration of the condition, sometimes temporary improvement.
- Neurological examination: general cerebral and local symptoms in varying proportions depending on the predominant localization of the process.
1) General cerebral symptoms.
It is based on a violation of liquorodynamics (cerebrospinal fluid circulation), most pronounced during obliteration of the foramina of Magendie and Luschka, much less often due to chorioependimitis. Clinical symptoms are caused by intracranial hypertension (96%) or CSF hypotension (4%). Hypertensive syndrome is more common and most pronounced in arachnoiditis of the posterior cranial fossa, when 50% of patients have congestive optic discs against the background of focal symptoms. Headache (in 80% of cases), often morning, bursting, pain when moving the eyeballs, physical stress, straining, coughing, nausea, vomiting. Also include: non-systemic dizziness, tinnitus, hearing loss, autonomic dysfunction, increased sensory excitability (intolerance to bright light, loud sounds, etc.), weather dependence. Neurasthenic manifestations (general weakness, fatigue, irritability, sleep disturbance) are common. Liquorodynamic crises (acutely occurring dyscirculatory disorders), manifested by increased cerebral symptoms. It is customary to isolate the lungs (short-term increase in headache, moderate dizziness, nausea); moderate severity (more severe headache, poor general health, vomiting) and severe crises. The latter last from several hours to 1-2 days and are manifested by severe headache, vomiting, general weakness, and impaired adaptation to external influences. Autonomic-visceral disorders are also common. Depending on the frequency, there are rare (1-2 times a month or less), medium frequency (3-4 times a month) and frequent (more than 4 times a month) crises.
2) Local or focal symptoms. They are determined by the predominant localization of organic changes in the membranes of the brain and adjacent structures. In general, focal symptoms are characterized by a predominance of irritation rather than loss. The exception is opticochiasmatic arachnoiditis.
- convexital arachnoiditis (in 25% of patients, more often of traumatic etiology). The predominance of local symptoms is characteristic (depending on the damage to the area of the central gyri, parietal, temporal). In the cystic form of arachnoiditis, usually mild or moderately expressed motor and sensory disturbances (pyramidal insufficiency, mild hemi- or monoparesis, hemihypesthesia). Epileptic seizures are typical (in 35% of patients), often the first manifestation of the disease. Secondary generalized partial seizures (Jacksonian) are common, sometimes with transient postparoxysmal neurological deficit (Todd's palsy). Polymorphism of seizures is characteristic due to the frequent temporal localization of the process: simple and complex (psychomotor), partial with secondary generalization, primary generalized, their combination. EEG reveals epileptic activity in 40-80% of patients (according to various sources), including peak-slow wave complexes. General cerebral symptoms are moderate, severe headaches, crisis states more often during exacerbation;
- basilar arachnoiditis (in 27% of patients) can be widespread or localized mainly in the anterior, middle cranial fossa, in the interpeduncular or optic-chiasmatic cistern. With significant spread, many cranial nerves at the base of the brain (I, III-VI pairs) are involved in the adhesive process, which determines the clinical picture of the disease. Pyramidal insufficiency is also possible. General cerebral symptoms are mild and moderate. Mental disorders (fatigue, decreased memory, attention, mental performance) are more often observed with arachnoiditis of the anterior cranial fossa.
The most distinct symptoms are in the case of opticochiasmatic arachnoiditis. Currently, it is rarely diagnosed, since in the vast majority of cases, chiasmatic syndrome is caused by other causes (see “Differential diagnosis”). More often it develops after a viral infection (flu), trauma, or against the background of sinusitis. General cerebral symptoms are mild or absent. Initial symptoms are the appearance of a grid before the eyes, a progressive decrease in visual acuity, often immediately bilateral, over 3-6 months. In the fundus there is first neuritis, then atrophy of the optic discs. The field of view is concentric, less often bitemporal narrowing, unilateral or bilateral central scotomas. Endocrine metabolic disorders are possible due to the involvement of the hypothalamus in the process;
- arachnoiditis of the posterior cranial fossa (in 23% of patients), usually post-infectious, otogenic. A severe, pseudotumorous course is often encountered due to severe disturbances in cerebrospinal fluid dynamics, damage to the caudal cranial nerves, and cerebellar symptoms. With predominant localization in the region of the cerebellopontine angle, damage to the VIII pair of cranial nerves (tinnitus, hearing loss, dizziness) appears earlier. Subsequently, the facial nerve suffers, cerebellar insufficiency and pyramidal symptoms are detected. The first symptom of the disease may be facial pain as a consequence of trigeminal neuropathy. Arachnoiditis of the cistern magna and adjacent formations is characterized by the greatest severity of hypertensive syndrome due to obliteration of the cerebrospinal fluid ducts and impaired outflow of the cerebrospinal fluid. Severe crises are frequent, cerebellar symptoms are pronounced. Complication is the development of a syringomyelitic cyst. Due to the serious condition of patients, it is sometimes necessary to resort to surgical intervention.
- Data from additional studies. The need for adequate assessment due to the difficulties and frequent errors in diagnosing arachnoiditis. It is incorrect to judge true (actual) arachnoiditis only on the basis of morphological changes detected on PEG, CT, MRI studies without taking into account the characteristics of the clinical picture, the course of the disease (progression of the first symptoms, the appearance of new symptoms). Therefore, it is necessary to objectify complaints indicating hypertensive syndrome, visual impairment, frequency and severity of crises, and epileptic seizures.
Only a comparison of clinical data and the results of additional studies provides grounds for diagnosing true current arachnoiditis and distinguishing it from residual stable conditions:
- Craniogram. Symptoms that are sometimes detected (digital indentations, porosity of the dorsum sella usually indicate a past increase in intracranial pressure (long-standing traumatic brain injury, infection) and cannot in themselves indicate current arachnoiditis;
- echo-EG allows you to obtain information about the presence and severity of hydrocephalus, but does not allow you to judge its nature (normotensive, hypertensive) and cause;
- Lumbar puncture. CSF pressure is increased to varying degrees in half of the patients. With exacerbation of arachnoiditis of the posterior cranial fossa, basal water levels can reach 250-400 mm of water. Art. lying down. A decrease in pressure occurs with chorioependimitis. The number of cells (up to several dozen in 1 μl) and protein (up to 0.6 g/l) increases in the case of active process, in other patients it is normal, and the protein content is even below 0.2 g/l;
- PEG has important diagnostic value. Signs of adhesive arachnoiditis, cicatricial changes, internal or external hydrocephalus, and an atrophic process are revealed. At the same time, PEG data can be the basis for the diagnosis of true arachnoiditis only if the clinical features and course of the disease are taken into account. They are often evidence of residual changes in the subarachnoid space and brain substance after injury, neuroinfection, and occur in patients with epilepsy without clinical signs of arachnoiditis;
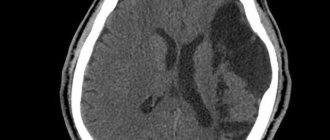
- CT and MRI make it possible to objectify the adhesive and atrophic process, the presence of hydrocephalus and its nature (aresorptive, occlusive), cystic cavities, and exclude space-occupying formations. CT cisternography allows us to identify direct signs of changes in the configuration of the subarachnoid spaces and cisterns. However, the information obtained has diagnostic value only with an adequate assessment of the lumbar puncture data (especially the state of liquor pressure) and the clinical picture of the disease as a whole;
- EEG reveals foci of irritation in convexital arachnoiditis, epileptic activity (in 78% of patients with epileptic seizures). These data only indirectly indicate the possibility of an adhesive process and do not in themselves constitute a basis for diagnosis;
- immunological studies, determination of the content of serotonin and other neurotransmitters in the blood and cerebrospinal fluid are important for judging the activity of the inflammatory meningeal process, the degree of involvement of the brain substance in it;
- ophthalmological examination is used for diagnostic purposes not only for opto-chiasmal, but also diffuse arachnoiditis due to the frequent involvement of the visual pathways in the pathological process;
- otolaryngological diagnosis is important primarily for determining the etiology of arachnoiditis;
- experimental psychological research allows us to objectively assess the state of mental functions and the degree of asthenia of the patient.
Symptoms of arachnoiditis
The first symptoms of the disease appear long after the exposure of the body to the provoking factor that caused its appearance. During this time, autoimmune processes occur in the patient's body.
The duration of this interval is directly related to which factor affected the body. For example, after a patient has had the flu, the first symptoms of arachnoiditis appear after a long period of time - from three to twelve months. After a traumatic brain injury, this period is reduced to 1-2 hours. At first, the patient is concerned about the symptoms characteristic of asthenia: sleep disturbance, weakness, fatigue, irritability. However, over time, more severe focal and cerebral symptoms of arachnoiditis may appear.
General cerebral symptoms of arachnoiditis
The cerebral complex of symptoms of cerebral arachnoiditis is characterized by liquor-hypertension syndrome. Most patients complain of a sharp headache, which is most active in the morning and can be aggravated by coughing, physical activity and straining. The consequences of increased intracranial pressure include such disorders as pain when moving the eyes, vomiting, nausea, and a feeling of strong pressure on the eyes.
Many patients turn to a neurologist with complaints such as decreased hearing, tinnitus, and attacks of dizziness. Therefore, during diagnosis, the doctor should exclude various ear diseases such as labyrinthitis, chronic otitis, cochlear neuritis, adhesive otitis. It is also possible that symptoms characteristic of vegetative-vascular dystonia may appear.
Patients with arachnoiditis occasionally experience liquorodynamic crises - attacks of headache accompanied by vomiting, nausea and dizziness. Rare crises are considered attacks with a frequency of no more than 1-2 times per month, average - 3-4 times, frequent - more than 4 times. Depending on the severity of symptoms during a crisis, its mild, moderate and severe forms are distinguished. The latter can last about two days.
Clinic of cerebral arachnoiditis
The disease develops acutely and quickly becomes chronic. Symptoms characterizing arachnoiditis can be divided into general cerebral and focal:
General cerebral symptoms are common to many neurological diseases
These include dizziness, general weakness, sleep disturbances, irritability, distracted attention and memory impairment. The main general cerebral symptom that is observed with inflammation of the arachnoid membrane is headache of varying severity.
Particularly severe headache attacks occur in the morning and may be accompanied by nausea and vomiting. Focal symptoms appear depending on the area of brain damage. With the convexital type, symptoms of cortical irritation and loss of some motor functions predominate. The leading manifestation is considered to be generalized and Jacksonian epileptic seizures. The development of pathology in the area of the base of the skull disrupts the functions of the nerves passing in this area. Decreased visual acuity and other disturbances in visual function indicate an inflammatory process in the area of the optic chiasm. A lesion near the cerebral peduncles manifests itself as symptoms of a disorder of the pyramidal system and oculomotor nerves.
Arachnoiditis near the cerebellopontine angle, in addition to headaches in the occipital region, is manifested by tinnitus, dizziness and, in rare cases, vomiting. When walking, the patient staggers, and the body tilts towards the affected side. The gait becomes ataxic in nature, dilatation of the veins of the fundus and horizontal nystagmus develop, in some cases pyramidal symptoms begin. Symptoms of damage to the trigeminal, abducens, facial and auditory nerves are common.
The development of arachnoiditis of the occipital cistern is an acutely developing process. The clinical picture includes fever, pain in the back of the head and neck, increased tendon reflexes, meningeal and pyramidal symptoms.
Focal symptoms of arachnoiditis
Focal signs of the disease occur depending on its location. Convexital arachnoiditis is characterized by mild to moderate disturbances in sensitivity and motor skills of the limbs. More than 35% of patients with this form of arachnoiditis experience epileptic seizures. After the attack ends, the patient experiences a neurological deficit for some time.
Basilar arachnoiditis, which is localized in the optic-chiasmatic region, occurs with serious impairments of attention and memory, as well as a decrease in mental abilities. In addition, patients with this form of pathology complain of a significant decrease in visual acuity and other visual disturbances. In rare cases, opticochiasmatic arachnoiditis is accompanied by inflammation of the pituitary gland, which provokes endocrine-metabolic syndrome, the symptoms of which are similar to those of a pituitary adenoma.
Arachnoiditis of the posterior cranial fossa is characterized by a very severe course. As a rule, patients show signs of facial neuritis and trigeminal neuralgia. Focal manifestations of arachnoiditis also include various cerebellar disorders: cerebellar ataxia, loss of coordination, nystagmus.
Classification
According to the nature of the course, the disease is divided into three forms: acute, subacute and chronic. Depending on the form in which the pathology occurs, one or another symptomatology will be visible.
According to the location in the brain, the following types are distinguished: localization of zones
- the spinal type occurs on the posterior surface of the spinal cord membrane, is formed as a result of injury, and may appear after some time.
- cerebral arachnoiditis, formed on the convex surface of the brain in the postcranial fossa/
Cerebral arachnoiditis, in turn, is divided into subtypes:
- arachnoid cyst of the posterior cranial fossa;
- arachnoiditis of the cerebellopontine angle.
- basilar;
- convexital;
Also, retrocerebellar arachnoiditis can be:
| Adhesive type | is a purulent inflammation of the lining of the brain with the formation of adhesions that cause severe pain. |
| Cystic-adhesive mixed type | with it, both adhesion of brain tissue and the formation of cystic growths are observed. |
| Cystic type | It is also characterized by inflammation of the lining of the brain, only with additional formation of cysts against the background of the disease. |
Diagnosis of arachnoiditis
Diagnosis of arachnoiditis involves a comprehensive assessment by a neurologist of the characteristics of the course of the disease and its clinical signs. One of the important stages of diagnosis is the collection of anamnesis, during which the neurologist pays attention to the nature and development of neurological symptoms, recent traumatic brain injuries of the patient and infections he has suffered. A study of the neurological status is also carried out, which makes it possible to detect mnestic and psycho-emotional disorders, as well as neurological deficits.
Since arachnoiditis is characterized by visual and auditory disturbances, a neurologist may need to consult an ophthalmologist and otolaryngologist for differential diagnosis. An otolaryngologist checks the degree and type of hearing loss using threshold audiometry. The degree of damage to the auditory analyzer can be determined using the study of auditory evoked potentials, electrocochleography and acoustic impedancemetry.
Instrumental techniques such as skull radiography, electroencephalography and echo-encephalography are not considered sufficiently effective in diagnosing arachnoiditis, since they provide limited information about the presence of the disease in the patient. However, with their help you can detect some symptoms of pathology. For example, cranial radiography detects symptoms of prolonged intracranial hypertension, echo-encephalography detects hydrocephalus, and electroencephalography detects epileptic activity.
More information about the disease can be collected using MRI and CT scans of the brain. Both of these studies are used to identify morphological changes in the brain (atrophic changes, the presence of adhesions and cysts) and the nature of hydrocephalus. These techniques are also used to exclude tumors, hematomas and brain abscess. The doctor obtains accurate information about intracranial pressure by performing a lumbar puncture.
Diagnostics
Inflammation of the arachnoid membrane of the brain is diagnosed by comparing the clinical picture of the disease and data from additional studies:
- plain radiograph of the skull (signs of intracranial hypertension);
- electroencephalography (changes in bioelectric parameters);
- tomography (computer or magnetic resonance imaging) of the brain (expansion of the subarachnoid space, ventricles and cisterns of the brain, sometimes cysts in the intrathecal space, adhesive and atrophic processes in the absence of focal changes in the brain substance);
- studies of cerebrospinal fluid (moderately increased number of lymphocytes, sometimes slight protein-cell dissociation, leakage of fluid under increased pressure).
Diagnosis of arachnoiditis includes a complete neurological examination. In the process of a full analysis, reflexes, vegetatives, and sensitivity are examined.
Treatment of arachnoiditis
The main goal of drug treatment for arachnoiditis is to eliminate the source of infection using antibiotics. The use of antihistamines and desensitizing medications (diazolin, histaglobulin, diphenhydramine, suprastin, pipolfen, tavegil, calcium chloride) is indicated. Drug therapy also involves improving metabolism and local circulation, as well as normalizing intracranial pressure.
Patients who experience increased intracranial pressure are advised to take diuretics and decongestants (furosemide, mannitol, glycerin, diacarb). To eliminate convulsive syndrome, antiepileptic medications (carbamazepine, finlepsin, keppra) are used. According to indications, the doctor may prescribe drugs from the following drug groups:
- absorbable (rumalon, lidase, pyrogenal);
- antiallergic (loratadine, tavegil, diazolin);
- neuroprotectors and metabolites (mildronate, nootropil, ginkgo biloba);
- psychotropics (tranquilizers, antidepressants, sedatives).
Symptoms of the disease
Of course, arachnoiditis is a very serious disease. And therefore it simply cannot be asymptomatic. There are a number of different signs that can make a doctor suspect arachnoiditis in a sick person:
- Headache
This symptom, to one degree or another, is inherent in all types of arachnoiditis without exception. However, those who suffer most from headaches are those who have the cerebral form of the disease. As a rule, they experience quite strong pain of a diffuse nature. However, although less frequently, there are still localized pain sensations.
The main distinguishing feature of a headache caused by arachnoiditis is its intensification with any, even the slightest, movement of the head. There is even a special test - the doctor asks a sick person to stand on his toes, and then suddenly shift his weight to his heel. If, at the moment when a person touched the floor with his heels, the pain intensified, one can suspect that he has arachnoiditis.
- Convulsive syndrome
If arachnoiditis affects the anterior parts of the brain, it is called convexital. This type of disease is characterized by disorders of both the motor system and various nerve receptors. A person’s movements become clumsy, sometimes it is quite difficult for him to even lift a cup.
The gait of a sick person is also specific - he may “sway” from side to side, he may bump into various objects. All this happens due to the fact that the cerebellum is affected to some extent. And the severity of movement coordination disorder directly depends on the degree of damage to the cerebellum.
Of course, all these changes greatly frighten both the sick person and his loved ones. But there is no reason to panic - in almost one hundred percent of cases, all these phenomena pass almost without a trace. The main thing is to seek medical help in time and receive adequate treatment.
In addition, a person often loses sensitivity, including pain. However, fortunately, sensitivity is only partially lost - complete loss is extremely rare, only in very severe cases. This form of the disease has another extremely unpleasant feature - it can often lead to the occurrence of convulsive syndrome - both focal and general. This is how arachnoiditis manifests itself in half of all patients.
- Decreased vision
In the event that a person develops arachnoiditis as a result of any injury, or as a result of the spread of the inflammatory process from the maxillary sinuses, the sick person may experience problems with the visual apparatus. A person may notice the appearance of blurry or bright spots before the eyes, then a gradual decrease in visual acuity begins in both eyes.
When examining the fundus of the eye, the ophthalmologist, as a rule, notes pronounced optic neuritis. However, if this happened to you or your loved ones, do not panic - after the arachnoiditis is cured, vision will gradually begin to recover. As a rule, over time it is restored in full, with rare exceptions.
- Increased intracranial pressure
In almost all cases of arachnoiditis, a phenomenon such as increased intracranial pressure can be observed. If such a phenomenon occurs, the doctor will most likely rule out the possibility of a disease such as arachnoiditis.
- Pain in the lumbosacral region
If arachnoiditis is localized in the spinal cord, the sick person may experience pain in the lumbar region, sacrum, or thoracic region, depending on the location. Moreover, these pains can be quite intense. In such a situation, it is very important to exclude osteochondrosis, radiculitis and acute pyelonephritis, which can disguise arachnoiditis.
Surgical intervention
If drug treatment does not produce the desired results, the patient experiences occlusive hydrocephalus or progressive vision loss, the doctor decides on surgical intervention. During the operation, adhesions are separated and cysts are removed. To reduce the manifestations of hydrocephalus, shunt operations are prescribed.
The prognosis for the patient is often favorable. Only arachnoiditis of the posterior cranial fossa, which is almost always accompanied by occlusive hydrocephalus, can pose a great danger. With frequent relapses of the disease, epileptic seizures and its optico-chiasmatic form, the labor prognosis for the patient may worsen.
Prognosis for arachnoiditis
In most cases, patients with arachnoiditis receive the third disability group. However, if they have severe visual impairment and frequent epileptic seizures, they may be assigned a second disability group. The first disability group includes patients with opticochiasmatic arachnoiditis, which caused complete blindness. Work in transport, at heights, near fire, in noisy rooms, in unfavorable climatic conditions, and with toxic substances is contraindicated for patients with arachnoiditis.