Drug treatment
There is no need for therapy if the tumor is small in size and does not cause discomfort to the patient.
It is enough to simply undergo periodic preventive examinations. But if the cyst begins to grow, then at first it is necessary to carry out drug treatment. According to ICD-10, the disease is coded G93. The patient is prescribed drugs that promote the resorption of adhesions. Tablets or injections are used to lower cholesterol levels.
Natalya Schneider, neurologist, Doctor of Medical Sciences, talks about the use of nootropic drugs:
In order for the functionality of brain cells to be maintained at the required level, they need to be supplied with glucose and oxygen. To do this, the patient uses nootropic substances: Nistenon, Picamilon. Naturally, it is also desirable to protect cells from the negative effects of changes in intracranial pressure. In this case, the patient is prescribed antioxidants.
During treatment, immunomodulators, anti-inflammatory, and antibacterial agents will be needed. Typically, patients are treated with tablets for 10-12 weeks. The treatment course is repeated after about six months. Therapy is prescribed only by a doctor. He also decides on the advisability of its extension. You can also use folk remedies, but it is also necessary to coordinate their use.
Treatment
If a patient is diagnosed with a frozen cerebrospinal fluid cyst with clinical compensation, then treatment is not indicated for him. In this case, the patient must be monitored by a neurologist with a mandatory annual MRI.
With a progressive cyst in the stage of clinical subcompensation, the patient is prescribed conservative therapy aimed at reducing intracranial pressure. If it is ineffective, surgical intervention is indicated. The choice of surgical method in each specific case is made by a neurosurgeon, taking into account the characteristics of the disease, the patient’s age, and the presence or absence of concomitant pathology.
Currently, the following surgical techniques are most commonly used:
- Complete excision. The indication for surgery is capsule rupture or hemorrhage into the cavity of the formation. The intervention is quite traumatic, and the recovery period is long.
- Endoscopic fenestration. A small hole is made in the bones of the skull using a milling cutter. Through it, puncture and aspiration of the liquid contents of the neoplasm are performed, followed by the creation of holes between its cavity and the subarachnoid space or ventricles of the brain. After this, the cavity in the arachnoid membrane is no longer filled with fluid and therefore the disease does not progress.
- Cystoperitoneal shunting. The essence of this operation is that a path is created for the outflow of cystic contents into the abdominal cavity, where it is absorbed into the blood.
Mysterious pineal gland with a cyst in it
A special type of cystic formation in the brain is considered to be a pineal gland cyst, which is better known to us as the pineal gland. What mission is assigned to the pineal gland in the human body is still not exactly clear. Scientists say that she:
- Produces melatonin, which is involved in the regulation of circadian (daily) biorhythms, so that a person does not get confused with sleep and wakefulness;
- Contributes to the process of puberty;
- Affects the growth of tumors (in some places it accelerates, in others it slows down).
Diagnosing a cyst of this small gland has become possible thanks to the advent of modern neuroimaging methods (for example, MRI). Previously, it was considered a rather rare pathology and accounted for only 1.5% of all brain diseases. Now many authors note that it was simply not found due to its asymptomatic course. Even now, not everyone does MRI every day, so in many cases, a pineal gland cyst is registered as an accidental finding, and in those who do not complain and are not specifically examined, it is considered that it does not exist at all.
A benign cystic formation of the pineal gland, located in one of the lobes of this mysterious organ, as a rule, does not cause much harm to it, does not affect functional abilities and is usually not prone to rapid growth. An epiphysis cyst, like other formations of a similar kind, as a rule, does not give specific signs, and if symptoms appear, they can easily be attributed to other brain diseases:
- A headache that occurs without a reason and has no system; the patient never knows when he will have a headache;
- An attack of cephalgia can be so strong that it causes nausea and then vomiting;
- There may be a lack of coordination of movements, which noticeably affects the patient’s gait;
- The reaction of the organs of vision to attacks is especially significant: it hurts to roll your eyes up, blurred pictures, double vision and fog make it difficult to see surrounding objects.
In rare cases, a cyst can also “show its character.” This happens when it grows rapidly and, reaching a critical size, begins to put pressure on neighboring areas of the brain, blocking the movement of cerebrospinal fluid and manifesting symptoms of hydrocephalus with the ensuing consequences.
Why did the cystic formation begin its journey in the pineal gland? Today there are two main reasons for its appearance there:
- For various reasons, the excretory canal closes and blocks the movement of the secretion of the gland, which remains and forms a place for itself;
- With the blood flow, a parasite, echinococcus, enters the pineal gland, which “settles in and settles in” in a new place, forming a capsule that protects itself from attacks by the immune system. The parasite releases the products of its vital activity within its “home,” thereby expanding its domain.
“House” for parasite larvae
Life cycle of Echinococcus. The parasite infects the brain, liver, lungs and other human organs
Echinococcus is a representative of helminths, the larvae of which, having entered the human body, which is the intermediate host, settle in it, forming cysts in various organs. The latter are more often localized somewhere in the liver or lungs, causing discomfort primarily to these areas, but sometimes they reach the brain through the bloodstream and settle in it. Often an attractive place for the parasite is the pineal gland, where it waits out the larval stage and forms cysts for this. True, once in the human body, which is a dead-end branch for the parasite, the helminth stops its development due to the impossibility of relocating to a permanent host.
A pineal cyst formed by echinococcus gives more vivid symptoms; mental disorders (depression, delirium, dementia) and convulsive seizures are added to the clinical manifestations that make one suspect a cyst.
Echinococcal cystic formations are diagnosed using the same methods as other brain cysts (CT, MRI, biopsy, if questions remain), however, a complete blood count can be useful here, which shows a noticeable increase in eosinophils (eosinophilia) and ESR.
Removal of a cyst, whether echinococcal or another nature, is carried out surgically, if the need arises:
- Hydrocephalus develops;
- Other brain structures and vascular beds suffer.
If the cyst behaves calmly, does not show a tendency to grow, does not give symptoms, the patient is monitored, which consists of an annual MRI and a visit to a neurologist.
GBOU "NIKIO im. L.I. Sverzhevsky" of the Moscow Department of Health
Nasal liquorrhea is the leakage of cerebrospinal fluid from the nasal cavity due to damage to the bones of the base of the skull and dura mater when the tightness of the subarachnoid space is broken.
Due to communication between the external environment and the cranial cavity, untreated liquorrhea leads to purulent meningitis in 10-25% of cases. In addition, a progressive decrease in intracranial pressure as a result of liquorrhea leads to the development of atrophic processes in the brain.
In 80-90% of cases, nasal liquorrhea occurs as a result of road traffic or other traumatic brain injuries; in approximately 15% of cases, this disease is iatrogenic. It should be noted that iatrogenic nasal liquorrhea largely depends on the surgeon’s experience and knowledge of anatomy. Spontaneous liquorrhea is rare - in 3-4% of cases. Spontaneous nasal liquorrhea can be divided into primary (idiopathic), the obvious cause of which cannot be established, and secondary, when extra and intracranial pathology leads to the formation of a liquor fistula. This is chronic intracranial hypertension, which sometimes leads to bone resorption, intracranial neoplasms and meningeal defects. Extracranial diseases include chronic diseases of the SNP, tumors of the SNP and respiratory infections.
The main symptom of the disease is considered to be the discharge of a clear, light-colored fluid, usually from one half of the nose when the head is tilted down. If cerebrospinal fluid (CSF) is released along with blood, then the classic “Halo” test is used to recognize liquorrhea. In this case, a characteristic light yellow rim forms on the gauze or bed linen around the central bloody spot. The “handkerchief” symptom has a certain meaning. This symptom is explained by the presence in the cerebrospinal fluid (CSF) of a large amount of protein, which is not present in catarrhal discharge during rhinitis. The handkerchief into which a patient with liquorrhea blows his nose becomes denser and harder. With obvious nasal liquorrhea, a symptom such as night cough may also occur due to the entry of cerebrospinal fluid into the trachea and bronchi in the long-term position of the patient on his back. There are various forms of the disease. In this case, nasal discharge can be obvious or scanty, constant or periodic, cerebrospinal fluid can be released from one half of the nose or both.
In itself, the discharge of cerebrospinal fluid from the nose causes obvious inconvenience for the patient, since it limits both physical and social spheres of activity. However, the main danger lies in the complications that the disease can cause. This primarily concerns meningitis, which develops due to the spread of the inflammatory process from the nasal cavity to the cranial cavity. It is believed that the longer liquorrhea lasts, the more likely the process is to spread to intracranial formations. Meningitis is an inflammation of the membranes of the brain, which often disables the patient and can even lead to death. Other serious complications of nasal liquorrhea include pneumocephalus, when air gets inside the skull, bronchitis and pneumonia when cerebrospinal fluid enters the respiratory tract, and gastritis - if cerebrospinal fluid accumulates in large quantities in the stomach.
Diagnosis of overt nasal liquorrhea is quite simple. After tilting the head down, a clear, light liquid begins to drip from one half of the nose. If you manage to collect about 1 ml. these secretions, it is necessary to determine the glucose level in them. This can be done in any clinical laboratory. Elevated glucose levels indicate liquorrhea, otherwise the diagnosis may lean toward vasomotor or allergic rhinitis. To determine the location of damage, a fairly large set of special diagnostic techniques is used. This includes computed tomography of the paranasal sinuses and cranial cavity, computer and magnetic resonance cisternography, radionuclide cisternography.
Diagnosis of nasal liquorrhea includes:
– test for beta2-transferrin in nasal discharge,
– CT scan of the SNP and anterior cranial fossa with reconstruction
– MRI of the brain to verify meningoencephalocele and fistula
– endoscopic examination of the nasal cavity
In difficult cases, it is also recommended to perform radionuclide scintigraphy. The sensitivity of the CT method for a cerebrospinal fluid fistula is quite high and amounts to 87-88%, but the exact localization of a rupture of the dura mater and nasal liquorrhea can only be determined by endoscopic examination of the nasal cavity and paranasal sinuses.
Treatment
The main goal in the treatment of a cerebrospinal fluid fistula or encephalocele is to restore the barrier between the nasal cavity and the SNP and the intracranial space with the least risk of developing intracranial infection.
Endoscopic endonasal access for plastic surgery of intraoperative complications of the dura mater was first used by Wiegand in 1981. The predecessor of endoscopic endonasal surgery for cerebrospinal fluid fistulas was a much more traumatic transcranial approach associated with known complications and adverse events - frontal lobe injury, hyposmia, anosmia, long-term disability. According to the literature, when intracranial access is used, relapse of liquorrhea occurs in 27% of cases during the first operation and 10% after a second operation.
The clear advantage of the endonasal approach is its high efficiency, visual control of the manipulations performed, minimal trauma for patients and the absence of skin incisions.
For the repair of cerebrospinal fluid fistulas, various biological and synthetic materials are used: free and pedicled flaps of the nasal mucosa, fragments of fat, fascia, muscle, tachocomb, hydroxyapatite, etc. The effectiveness of the operation for small defects of the skull base (up to 1 cm in size) is not depends on the plastic material used. For large defect sizes, 2-3 layer plastic surgery using biological adhesives (Bioglue, Tissucol, etc.) is recommended.
We have developed:
- layer-by-layer plastic surgery of the defect area with tachocomb, sealant (Duraseal Bioglue, Tissucol), tachocomb and hemostatic sponge and/or surzhecel napkin;
- stump of the middle turbinate (free mucosal flap of the inferior turbinate), mucoperiosteal flap of the nasal septum, sealant (Duraseal Bioglue, Tissucol), tachocomb and hemostatic sponge and/or surjecel napkin.
In order to monitor the closure of the cerebrospinal fluid fistula, patients after plastic surgery of the skull base may undergo instrumental (radionuclide, CT or MR cisternography) or laboratory tests (tests for β2-transferrin or β-trace protein) for hidden liquorrhea. Instrumental diagnosis of liquorrhea in patients in the immediate postoperative period is associated with objective difficulties. Thus, carrying out scintigraphy, CT and MR cisternography requires endolumbar administration of a contrast agent and then positioning the patient on his stomach, preferably with a slight downward tilt of the head end of the gurney to fill the cisterns of the base of the brain for 30-40 minutes. The very preparation for the study can provoke a recurrence of liquorrhea and potentially, in the early postoperative period, does more harm than good. Tests for β2-transferrin or β-trace protein are highly sensitive (sensitivity - 96 - 97%) and non-traumatic.
Types of brain cysts
K»Ã°ÃÂÃÂøÃÂøúðÃÂøàðÃÂðÃÂýþøôðûÃÂýààúøÃÂà÷ðòøÃÂøÃÂ:
- Ã] ²²Pa · ãâtely · ãâte ¸.
- ÃÂàÃÂÃÂúÃÂÃÂÂÃÂ: ÿÃÂþÃÂÃÂþù (ø÷ úûõÃÂà¾Ãº ðÃÂðÃÂýþøôðûÃÂýþù þñþûþÃÂÃºà ¸) øûø ÃÂûþöýþù (ÃÂüõÃÂø ð ÃÂðÃÂýþøôðûÃÂýÃÂàúûõþú ø ôÃÂÃÂà ³Ã¸Ã ÃÂúðýõù).
- ÃÂàÃÂÃÂõÿõýø ÃÂð÷òøÃÂøÃÂ: ÿþûþÃÂÃÂà ¸, ÃÂòõûøÃÂøòðÃÂÃÂøõÃÂàò ÃÂð÷üõÃÂð àøûø ÿÃÂõúÃÂà°ÃÂøòÃÂøõ ÃÂþÃÂÃÂ.
From the editor: Features of obstructed venous outflow
ÃÂÃÂòðõàø ÿþ üõÃÂÃÂàþñÃÂð÷þòðý øÃÂ: ðÃÂðÃÂýþøôðûÃÂýðà(ýð ÿþòõàÃÂýþÃÂÃÂø üþ÷óð), ÃÂõÃÂÃÂþÃÂõà»ÃµÃ±ÃµÃ»Ã»ÃÂÃÂýðà(ò óûÃÂñøýõ ÃÂõÃÂþà³Ã¾ üþ÷óþòþóþ òõÃÂõÃÂÃÂòð).
ÃÂõÃÂÃÂþÿþûþöõýøõ úøÃÂàò óþû þòýþü üþ÷óõ:
- ÷ðôýÃÂàÃÂõÃÂõÿýðàÃÂüúð;
- ÿÃÂðòðàòøÃÂþÃÂýðàôþûÃÂ;
- ûõòðàòøÃÂþÃÂýðàôþûÃÂ;
- ÃÂõûàüõöôàÿþûÃÂÃÂðÃÂøÃÂüø;
- ûþñýðàÃÂðÃÂÃÂÃÂ;
- ÃÂõüõýýðàÃÂðÃÂÃÂÃÂ;
- üþ÷öõÃÂþú;
- ÃÂøÃÂúþòøôýðàöõûõ÷ð.
ÃÂÃÂðÃÂýþøôðûÃÂýðàúøÃÂÃÂð üþöõà A ÷óþòþü úðýðûõ, ýð úþýÃÂõ ýõà VALUE The úÃÂõÃÂÃÂÃÂð.
How can traditional medicine help?
The task of folk remedies is the same as traditional ones - to improve blood circulation, metabolism, and eliminate symptoms. Properly selected recipes will help cope with annoying headaches and can even slow down the growth of the cavity.
In folk medicine it is common to use:
- Hemlock. The crushed seeds of the plant can be infused in half a liter of olive oil. You need to mix and leave the product for three weeks in a cool place. It is recommended to instill this oil solution 2 drops into the nose 2-3 times a day.
- Dioscoreim Caucasian (root). 4 parts of the root need to be crushed and poured with vodka (1400 ml). The infusion is poured in stages. First, take half the roots and pour 700 ml of vodka in a glass container. You need to leave it for 5 days. Then you need to drain all the liquid and pour a fresh portion of vodka (700 ml) over the roots. Leave again for 5 days. The infusion should be taken one teaspoon three times a day.
- Decoctions of raspberries, licorice, wormwood, elecampane, chamomile, and calendula will help reduce intracranial pressure.
For some reason, many people believe that folk remedies are safe. This is wrong. To avoid unpleasant consequences, you should definitely ask your doctor whether you can use them specifically. It is the doctor who must select the folk remedy. Otherwise, it may not only not help, but also seriously harm. In addition, some medications are incompatible with herbs or alcohol.
When is a consultation with a neurosurgeon necessary?
Newborns today are almost universally examined using neurosonography (ultrasound examination of the brain). During this test, infants often have some type of cyst. If the cyst is large, specialists will likely recommend an MRI. If not, they will watch. A rapidly enlarging cyst, or a cyst causing epileptic seizures or other neurological symptoms, requires consultation with a neurosurgeon.
If, at the age of several months, a previously healthy child shows signs of increased intracranial pressure and a cyst is detected during examination, surgical treatment is necessary.
When an older child is examined for a traumatic brain injury and a cyst is accidentally found, we are NOT talking about surgical treatment.
If an examination is prescribed due to speech delay or developmental delay, then the cyst found is a reason to consult with a surgeon to understand whether this cyst is associated with these symptoms.
When a school-age child is examined due to the appearance of severe headaches, the cyst found should be discussed with a neurosurgeon. Perhaps surgery will help eliminate the cause of these pains.
If a child who practices martial arts or boxing undergoes a mandatory MRI (young athletes are required to undergo examinations before competitions), during which a cyst is accidentally discovered, it is necessary to obtain advice from a neurosurgeon about the possibility of practicing these sports. A cyst without additional symptoms in older children is usually not life-threatening. But it has contraindications for engaging in traumatic contact sports, primarily martial arts and boxing, and to a lesser extent football and hockey. This cyst does not require surgical treatment.
MRI diagnostics for arachnoid cyst
Despite the fact that CT allows you to accurately determine the size and location of the cyst, MRI provides the most accurate and complete information about the formation. Typically, to diagnose an arachnoid cyst, an MRI scan is performed with the injection of contrast into the patient's bloodstream. At the same time, brain tumors tend to accumulate contrast, and cysts do not absorb it from the blood vessels, which is very clearly visible on MRI.
Also, MRI scanning allows you to distinguish a cyst from hemorrhages, hematomas, hygromas, abscesses and other diseases with similar symptoms. In addition, MRI makes it possible to identify a cyst even in cases where the patient does not yet have any symptoms, and the cyst itself measures only a few millimeters.
Get an MRI of the brain in St. Petersburg
Basic signs
Acquired and congenital vertebral cysts are classified according to the place of their formation. Symptoms of the pathology are largely related to the location of the pseudotumor, its type, size, and stage of growth. Sometimes the neoplasm develops for a long time, without giving obvious signs, and sometimes it causes pain to the patient in the early stages. The severity of pain is determined by the pressure of the cyst on the spinal roots and its proximity to the nerve ganglia.
There are main signs that develop in all types of benign vertebral tumors:
- Sharp and dull pain, concentrated in the area of the cystic capsule, which disturbs the patient even at rest, intensifying with movement. Usually there is a return of pain (irradiation) to the thoracic and pelvic region, buttocks and limbs.
- Radicular syndrome, which develops with the growth of spinal cysts localized near the spinal nerve root and ganglia (nerve plexuses), which are compressed as the tumor grows and moves. It manifests itself:
- pain and shooting in completely different parts of the body - neck, arms, legs, lower back, sacrum, behind the sternum, in the esophagus, stomach, which is determined by which nerve node is irritated;
- muscle weakness and atrophy (shrinkage);
- impaired sensitivity in the legs and arms, as well as in the area of the affected root.
- If a spinal cord cyst has formed, then as it enlarges, neurological manifestations of varying severity occur:
- increasing weakness in the lower extremities, gradual atrophy of muscles controlled by the affected spinal nerves;
- impaired skin sensitivity to pain, cold and heat due to damage to cells that perceive pain and temperature fluctuations;
- burning sensation, cold goosebumps, tingling, numbness in the arms, legs, fingers;
- headaches, sound hearing impairment (noise, ringing), dizziness, feeling of pulsation in the head, increased blood pressure;
- double vision, blurred vision, spots and threads before the eyes;
- sudden loss of consciousness, seizures;
- disruption of the intestines and genitourinary system;
- the appearance of lameness, loss of coordination of movements, balance, changes in gait.
Symptoms
Clinical manifestations of cerebrospinal fluid cystic formation include general cerebral and focal symptoms:
| Group of symptoms | Description |
| General cerebral | Their development is associated with an increase in intracranial pressure. The patient develops persistent headaches that are bursting in nature. They usually get worse at night and early in the morning. At the height of a painful attack, nausea occurs, and there may be repeated vomiting. Mental disorders may develop (psychomotor agitation, impaired critical abilities). When examining the fundus, congestion is revealed. |
| Focal | Caused by local damage to certain brain structures. When the formation is localized in the area of the frontal lobes, motor function suffers to a greater extent and the patient develops muscle hypertonicity, instability appears when walking, and speech disorders may occur. Lesions of the parietal lobe are characterized by disturbances of perception and sensitivity. Signs of damage to the temporal lobe are hallucinations, seizures, and defects in auditory perception. Localization of the cerebrospinal fluid cyst in the region of the occipital lobes causes dysfunction of the visual analyzer. With this form of the disease, the patient experiences symptoms such as cortical blindness, visual agnosia, and visual illusions. |
Causes
If the appearance of cysts was preceded by a difficult pregnancy in the expectant mother, experts call such tissue defects primary. Provoking factors are:
- uncontrolled use of medications by a woman;
- alcohol abuse;
- past infectious diseases;
- abdominal injuries.
If the formation of a tumor occurred in the postneonatal period of life, then the reasons may be:
- neuroinfections - for example, meningitis, or encephalitis, tuberculosis or syphilis;
- surgical interventions on brain structures;
- agenesis of the corpus callosum – absence of an anatomical unit or its replacement with a cyst;
- traumatic brain injuries;
- helminthic infestations;
- intracerebral bleeding.
From the editor: Causes of headaches after alcohol
Sometimes an arachnoid vesicle is identified as a result of examinations that were performed for other indications. The reasons for such formations are not reliably known - the person himself does not remember what could have been the impetus for the formation of the intracerebral cavity.
Features of therapy
As a rule, treatment of a cyst is prescribed only after a full diagnostic examination, which is performed using computed tomography or magnetic resonance imaging, which allows you to see the clear contours of the formations, determine their size, as well as the degree of impact on surrounding tissues.
It should be borne in mind that the presence of such cavities is not necessarily associated with cancer and usually responds well to treatment. During a magnetic resonance imaging study, the patient is injected with a special contrast agent, which makes it possible to determine what exactly is in his brain: a cyst or a malignant tumor. MRI is recommended to be performed repeatedly to constantly monitor the dynamics of the disease.
Methods for treating a brain cyst are selected based on the reasons as a result of which it arose. Emergency assistance is usually needed in the following cases:
- constantly recurring seizures;
- hydrocephalus;
- rapid increase in cyst size;
- hemorrhages;
- damage to brain structures located next to the cyst.
As a rule, non-dynamic brain cysts do not require intervention, while dynamic ones are treated using medicinal and surgical methods.
Traditional treatment involves the use of various medications, the main purpose of which is to eliminate the causes of the disease. Doctors may prescribe medications to patients that resolve adhesions, such as caripain or longidase. In order to restore blood circulation, they prescribe medications aimed at reducing cholesterol concentrations, normalizing blood pressure and blood clotting.
You can provide brain cells with the necessary amount of oxygen and glucose with the help of nootropics, for example, picamilon, pantogam, instenon. Antioxidants will help make cells more resistant to intracranial pressure. In addition, immunomodulatory, antibacterial and antiviral agents are sometimes used, which are necessary in case of detection of autoimmune and infectious diseases.
The appearance of arachnoiditis signals, first of all, that the patient’s immunity is greatly weakened, which is why it is necessary to actively restore the defenses. In order to select a consistent and safe course of immunomodulatory and anti-infective treatment, you need to take a blood test. As a rule, all medications are prescribed in courses lasting about three months, repeated twice a year.
Do they take you into the army with a cyst?
The Medical Commission uses the provisions of Article 23 of the Schedule of Diseases. Paragraph “d” describes in detail the examination of conscripts with congenital brain abnormalities. A congenital pathology that does not manifest itself in any way, does not cause pain and does not impair functions, allows the commission to consider the guy fit for service in the “B-4” category. He will repay his debt to his homeland in a certain branch of the military.
Severe damage to the nervous system gives the right to receive a fitness category of “D” or “B”. The conscript receives release, the army does not shine for him.
The secondary nature of the neoplasm is considered under Article 25 of the Schedule of Diseases, on the basis of which the following fitness categories are assigned:
- "D": not fit for service.
- “B”: limited eligibility, receiving a military ID without serving, not conscripted in peacetime. Obtaining this category is possible only if the person is registered, carries out the necessary medical procedures and the treatment does not help.
With or without a cyst, life goes on. A person’s well-being depends only on a responsible attitude towards it. What prevents you from undergoing a medical examination on time, a couple of times a year? The consequences of negligence can be costly. Time is one of the main factors in detecting tumors.
Cavity formation in the brain
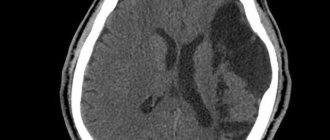
Fig2. General view of an intracerebral brain tumor with volumetric effects
1. In the photographs, the tumor is characterized by a volumetric component in the process of growth with an increase in its own mass, the so-called “plus tissue” sign.
Fig3. General view of a brain tumor in the frontal lobe on CT
2. Brain tumors have a mass effect, due to the volumetric influence of their own stroma, displacing and expanding the normal anatomical structures of the brain.
Fig4. An example of the volumetric effect of a tumor on the corpus callosum, shown on an MRI image
3. For benign brain tumors, it is typical to have clear boundaries on MRI and CT, since they have a capsule that separates them from brain tissue, a so-called expansive growth pattern (as a result of an increase in size, adjacent parts of the brain are displaced, pushed aside), relatively slow growth rates and absence of metastasis.
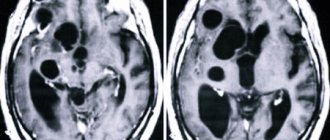
Fig5. example of a benign tumor (indicated by an asterisk), with a capsule, expansive growth and volumetric effect on MRI
4. For malignant brain tumors, the absence of clear contours and boundaries is typical; on the contrary, their edges are not visible, they are characterized by an infiltrative type of growth (that is, they spread their cells between the cells of healthy tissue - infiltration), necrotic decay (in the center the tumor begins to devour itself due to lack of nutrition, which leads to self-digestion of the central areas of the tumor), high rates of growth and development (short-term dramatic outcome) and metastasis (spread of the tumor to neighboring areas of the brain along the membrane and through the cerebrospinal fluid).
Fig6. Malignant tumor of the left frontal lobe with edema, necrotic decay and without distinct boundaries
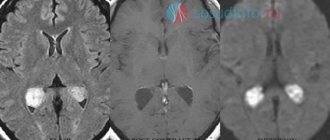
5. In MRI and CT images, brain tumors in most cases accumulate contrast agent after intravenous contrast enhancement, which is a sign characteristic of tumors, although some tumors do not accumulate contrast, but this is more typical for the initial stages of formations.
6. The tumor changes the MR signal, becoming brighter or darker in the brain substance, since it consists of a separate type of tissue, although there are tumors that are “not visible” on imaging or not visible without contrast. Almost all brain tumors are visible on MRI, but can be missed on CT.
Fig7. An example of a change in brightness (MR signal) on a tomography in a region of the brain affected by a tumor
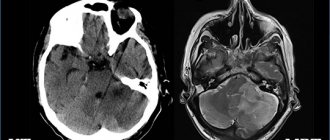
7. Perifocal edema is a feature not only of a brain tumor, but is very characteristic of tumor formations affecting the substance of the brain. Edema increases the mass effect of the tumor, leads to increased intracranial pressure and can cause displacement of brain structures or their pinching in anatomically narrow places (herniation).
Fig8. Severe perifocal edema of the brain substance surrounding the tumor on an MRI image
Due to the fact that brain tumors are not always represented by ovoid, round formations, as patients are accustomed to perceive them, and other pathological processes in the body tissues can lead to exactly this kind of shape, diagnosis becomes quite difficult and sometimes requires extraordinary knowledge and experience.
Cysts in the brain are benign neoplasms, which are a bubble with liquid contents inside. Young children and adults face a similar problem. Not everyone knows what a cyst is.
From the editor: Causes, types, symptoms and treatment of strokes with hemorrhage
They are localized both in the left hemisphere and in the right. The clinical picture of the disease largely depends on this. Congenital cysts most often appear between the ages of 30 and 50 years. The growth of these tumors can be fast or slow.
In the latter case, wait-and-see tactics are often used. A cyst in the brain can be arachnoid (located in the area of the arachnoid membrane) and intracerebral. Depending on the location, the following types of neoplasm are distinguished:
- pineal gland;
- dermoid;
- choroid plexus;
- colloidal.
Classification
There are several classifications of arachnoiditis. Based on the established cause, arachnoiditis can be post-traumatic, infectious (rheumatic, post-influenza, tonsillitis) and toxic, depending on the type of changes - cystic, adhesive-cystic, limited and diffuse, single-focal and multifocal.
Depending on the clinical picture and course, acute, subacute and chronic arachnoiditis are distinguished, but for diagnosis it is most important to determine the location of arachnoiditis and predict the pattern of exposure and consequences of membrane lesions.
Depending on the predominant location and structures involved in the pathology, arachnoiditis can be of various types: cerebral, basal, opto-chiasmal, pontocerebellar, precerebellar, spinal, etc.
Cerebral arachnoiditis
The cerebral type of arachnoiditis usually covers the membranes of the brain of the anterior parts of the cerebral hemispheres and areas of the central gyri, affecting not only the archnoid endothelium, but also the structures of the soft medulla with the formation of adhesions between them. As a result of the adhesive process, cysts with liquor-like contents are formed. Thickening and compaction of cysts can lead to xanthochromic tumor-like formations containing large amounts of protein, which can manifest as the development of status epilepticus .
Arachnoid cyst of the brain
Optico-chiasmatic arachnoiditis
It is most often localized in the chiasmal region and affects the base of the brain, involving the optic nerves and their chiasm in the pathology. This is facilitated by traumatic brain injuries (concussion or contusion), infectious processes in the paranasal sinuses, as well as diseases such as tonsillitis, syphilis or malaria . Its result can be irreversible vision loss, which begins with pain behind the eyeballs and visual impairment, which can lead to unilateral and bilateral temporal hemianopia, central scotoma , concentric narrowing of the visual fields.
The development of pathology is slow and not strictly local; it can spread to areas distant from the chiasm, usually accompanied by the formation of multiple adhesions, cysts, and even the formation of a scar membrane in the chiasm area. A negative effect on the optic nerves causes their atrophy - complete or partial, which is ensured by mechanical compression by adhesions, the formation of congestive nipples and blood circulation disorders ( ischemia ). In this case, initially one of the eyes suffers more, and after a few months the second one is also involved.
Spinal arachnoiditis
In addition to these well-known causes, spinal arachnoiditis can be caused by furunculosis and purulent abscesses of various locations. In this case, cystic limited formations cause symptoms similar to an extramedullary tumor, symptoms of compression of spinal cord structures, as well as radicular syndrome and conduction disorders, both motor and sensory.
Chronic inflammatory processes cause protein-cell dissociation of the cerebrospinal fluid and most often affect the posterior surface of the thoracic, lumbar or cauda equina spinal cord. They can spread to several roots or, in case of diffuse lesions, to a large number, changing the lower limit of the sensitivity disorder.
Spinal archnoiditis can be expressed as:
- in the form of tingling, numbness, weakness in the legs, unusual sensations in the limbs;
- the occurrence of leg cramps, muscle spasms, spontaneous twitching;
- in the form of a disorder (increase, loss) of such reflexes as knee, heel;
- attacks of severe shooting pain like electric shocks or, on the contrary, aching pain in the lower back;
- disruption of the pelvic organs, including decreased potency .
Irritation and compression of the cortex and nearby parts of the brain during arachnoiditis can be complicated by the formation of cysts of various types - retrocerebellar, cerebrospinal fluid, left or right temporal region.
Retrocerebellar arachnoid cyst
A retrocerebellar cyst is formed when the choroid plexus of the fourth ventricle is displaced upward and backward from the intact vermiform part of the cerebellum. To identify this type of cyst, CT and MRI are approximately equally informative.
Arachnoid cerebrospinal fluid cyst
It is customary to distinguish between intracerebral and subarachnoid cerebrospinal fluid cysts, the former are more common in adults, and the latter are more typical for pediatric patients, which is very dangerous and causes mental retardation.
Liqueur cysts are formed by arachnoid endothelium or scar collagen and filled with cerebrospinal fluid. They can be congenital or formed during the resorption of intracerebral hemorrhages, foci of bruises and crush injuries of the brain, in the zone of ischemic softening after injuries. They are characterized by a long-term remitting course, initiating epileptic seizures of different structure, duration and frequency.
A cerebrospinal fluid cyst can also occur as a result of subarachnoid hemorrhage or reactive adhesive leptomeningitis.
Arachnoid cyst of the right temporal region
A cyst in the right temporal region can cause headaches, a sensation of pulsation, squeezing of the head, noise in the ear, attacks of nausea, convulsions , and uncoordination of movements.
Arachnoid cysts are frozen, stable and most often do not cause discomfort or cerebral disorders. An asymptomatic course can lead to the formation being detected only during a brain tomography if arachnoiditis is suspected.
Arachnoid cyst of the left temporal lobe
If the left temporal lobe cyst is progressive, then it can gradually increase focal symptoms due to pressure on the brain. It is usually located in the left temporal lobe and looks like an extension of the external cerebrospinal fluid space.
When a patient learns about a cyst in the left temporal region, it often turns out that it is not fatal and may not cause negative symptoms. However, in some cases there is a risk of developing speech disorders (sensory aphasia ), loss of visual fields, sudden spasms of the limbs or the whole body.
Other types of brain cysts
The following types of cysts are also common:
- Cyst of the epiphysis of the brain, the symptoms of which are severe headaches, drowsiness, disorientation, double vision. It also makes walking difficult. At the initial stage of the disease, drug treatment is used. A neglected cyst that increases in size is removed surgically.
- Vascular plexus cyst is a benign neoplasm that manifests itself at certain stages of fetal development in the womb. Such a brain cyst in a child most often resolves on its own. In some cases, a brain cyst in a newborn occurs as a result of complications during pregnancy and childbirth. Infectious infection of the fetus can also lead to it. In rare cases, this formation leads to pathological changes in other body systems. A congenital brain cyst is determined using a procedure called neurography. It is absolutely harmless to the child's health. Diagnosis of such a cyst in adults is made using ultrasound examination.
- Pseudocyst of the brain in newborns occurs in 1% of premature infants. It is detected by ultrasound in the first 24 hours of a child’s life. This fetal brain cyst occurs as a result of hemorrhage of the germinal matrix. It can be unilateral or bilateral. Pseudocysts are the safest health consequence of childbirth. They do not require special treatment. As a rule, by the first year of a child’s life they completely resolve.
- A cerebrospinal fluid cyst is a neoplasm that arises between the meninges. Its formation is promoted by inflammatory processes (meningitis, stroke), trauma and surgery. It is diagnosed in adulthood, since in the early stages its symptoms are practically not expressed. Symptoms of a liquor cyst: nausea, vomiting, mental disorders, loss of coordination, convulsions, paralysis of the limbs.
- A subependymal cyst occurs in newborns after a cerebral circulatory disorder or during hypoxia (insufficient oxygen supply to the brain). This disease requires medical supervision.
- Porencephalic cyst of the brain is a formation that occurs in its tissues due to melting of the affected area. It leads to very serious consequences such as hydrocephalus and schizencephaly.
- A lacunar cyst forms in the area of the pons, in the cerebellum, subcortical ganglia, and optic thalamus. Most often it occurs as a result of age-related changes and atherosclerosis.
- Colloidal cyst is of congenital origin. It appears as a result of embiogenesis. A person can have it all his life, but it does not cause him any problems. It is believed that it is hereditary. This cyst blocks the flow of fluid. It is often accompanied by headache, epileptic seizures, weakness in the legs and high intracranial pressure. The symptoms of this disease manifest themselves most clearly in adulthood. Sometimes this disease causes hydrocephalus and cerebral hernia. In rare cases, it is fatal.
Colloidal cyst
Cysts of different parts of the brain
In some cases, doctors diagnose the following diseases:
- A pituitary cyst of the brain is a benign formation. It appears mainly in people aged 30-40 years. There are practically no pituitary cysts in children and adolescents. This disease is dangerous because the tumor affects the central nervous system. Most often, such a cyst is removed surgically.
- A cerebellar cyst can occur for a number of reasons. Most often, its treatment is aimed at resolving adhesions. If the cyst is formed as a result of autoimmune processes or infection, anti-inflammatory therapy will be needed. Surgical intervention is performed if there are signs of hemorrhage, convulsions, or loss of coordination of movement. In most cases, this disease is completely curable.
Diagnosis and treatment of cerebrospinal fluid cyst
An accurate diagnosis of a cerebrospinal fluid cyst is only possible using instrumental research methods, since there are either no symptoms at all, or they correspond not only to a cyst, but also to any other space-occupying process, occlusive hydrocephalus and other disorders in the skull. The neurologist prescribes:
- CT and/or MRI;
- electroencephalography for seizures;
- Ultrasound of the brain and its vascular system (more often in children of the first year of life).
MRI with contrast is one of the best ways not only to diagnose a cyst, but also to exclude a tumor, hemorrhage, or abscess. Ultrasound, or echoencephalography, is usually used in children and is performed through a fontanel that has not yet closed.
A small cerebrospinal fluid cyst is subject only to observation; treatment is not carried out due to the absence of symptoms. Every year, such patients undergo a brain tomography to make sure that the cyst is not growing or to record its changes.
A large cerebrospinal fluid cyst, causing hydrocephalus or compressing brain tissue, not amenable to conservative treatment, and also actively growing, requires surgical treatment , which includes several methods of decompression of the skull:
- Shunt operations;
- Fenestration;
- Needle aspiration of excess fluid.
shunting to drain excess cerebrospinal fluid
Open trepanation has recently been increasingly replaced by endoscopic interventions, which are less traumatic and have a lower risk of complications. Open trephination is necessarily performed in cases where blood has leaked into the cavity of the cerebrospinal fluid cyst.
Fenestration is a neuroendoscopic intervention to remove excess fluid from a cerebrospinal fluid cyst in the brain. During fenestration, a connection is created with the ventricles of the brain or subarachnoid space.
Shunt operations for a cerebrospinal fluid cyst with occlusive hydrocephalus are aimed at removing fluid, which is redirected into the abdominal cavity or pleura through a specially installed shunt system.
Symptomatic treatment of a cerebrospinal fluid cyst includes anticonvulsants, nootropics, and diuretics. Vascular agents, neuroprotectors, as well as antidepressants and tranquilizers are prescribed.
All ages are submissive: cysts in infants
In newborns, cystic formations formed either during intrauterine development or appeared as a result of birth trauma. The same reasons precede the appearance of cysts in infants, and, in addition, new prerequisites are added, for example, infectious and inflammatory processes or hematomas resulting from injuries, which result in cerebral circulatory failure, leading to hypoxia and ischemia, and, consequently, to the death of neurons in some part of the brain (the place where the cyst forms).
Subsequent degeneration of the nervous tissue, its necrosis, will serve as a good place for the formation of a cavity, which will begin to accumulate fluid, enlarge and compress neighboring areas and liquor-conducting pathways. This will most likely result in hydrocephalus and give certain neurological symptoms, delayed growth and development of the child.
A cyst in a child’s head can form anywhere; therefore, the main types of cystic formations localized in the brain are distinguished:
- Arachnoid cyst resulting from trauma and inflammatory processes. The habitat can be any part of the brain, characterized by rapid growth, manifested by hydrocephalus with its characteristic symptoms.
- The most severe forms of the cystic process include the subependymal cyst. Its cause is circulatory failure in the brain followed by ischemia. Such a cyst requires increased attention to itself and constant monitoring of the child (MRI annually to avoid excessive growth)
- A choroid plexus cyst, which develops in the fetus and by the time the baby is born, usually disappears safely.
Choroid plexus cysts (pictured) - in most cases, a phenomenon that does not require concern
The cystic process is diagnosed in early infancy using neurosonography (ultrasound), and the cyst is removed surgically.
Types of spinal cysts
Based on their origin, spinal cysts are divided into:
- congenital,
- acquired.
Depending on the morphological features (wall structure), the cyst can be:
- true (there is an epithelial lining inside the cystic formation)
- false (no epithelial lining)
- Ganglionic. This formation does not have a synovial membrane inside the cavity layer of endothelial cells. As the tumor grows, it gradually separates from the bone.
- Periarticular cyst.
The size, location and shape of a spinal cyst vary depending on the genesis of the formation.
Spinal cysts are divided into morphological types:
A periarticular cyst of the spine forms in the area of the intervertebral (facet) joints. Often formed due to injury or degenerative disorders (in older people). Most often, it forms in the facet joints of the lumbar and thoracic spine. Once formed, the periarticular cyst extends beyond the facet joint cavity. Periarticular cyst of the spine is the cause of radicular syndrome in almost 1% of cases. Depending on the presence of synovial epithelium, the periarticular cyst is divided into: ganglion and synovial.
Perineural cyst of the spine.
Perineural cyst of the spine is found in almost 7% of cases of all cystic formations. Often this cyst is of congenital origin, due to a violation of the development of the spine in the embryonic period - there is some protrusion of the spinal cord in the lumen of the spinal canal. If this is a small protrusion, then it does not manifest itself clinically. If the protrusion is large, then compression of the spinal nerves occurs with corresponding symptoms, which can appear in childhood.
Aneurysmal cyst.
An aneurysmal cyst of the spine is a cavity formation inside the bone tissue of the vertebra, which gradually increases and is filled with venous blood. This serious pathology is quite rare, is associated with tumor-like diseases and often leads to severe vertebral fractures. The cyst develops more often in childhood, mainly in girls. The formation of an aneurysmal cyst is usually caused by trauma.
Arachnoid cyst. An arachnoid cyst of the spine (Tarlov cyst) is a cavity formation, the walls of which are lined with the arachnoid membrane of the spinal cord. With dimensions greater than 15 mm, it can have a compressive effect on the nerve roots and spinal cord, which will manifest itself with characteristic symptoms.
CSF cyst of the spine
A spinal cerebrospinal fluid cyst is a cavity containing cerebrospinal fluid fluid, this fluid that circulates in the space of the spinal cord. Clinically, a cerebrospinal fluid cyst will manifest itself depending on the level of its location in the spine, and the neurological deficit below the level of localization of the cyst.
Cysts in the lumbar and sacral region. When small in size they do not appear clinically. As the size increases, symptoms and functional neurological deficits occur, depending on which root is compressed.