More information about other types of diseases starting with the letter “N”: Sleep disturbance; Narcolepsy; Hereditary cerebellar ataxia of Pierre-Marie; Spinal circulatory disorders; Trigeminal neuralgia; Neuralgia of the submandibular and sublingual nodes; Neuralgia of the glossopharyngeal node; Neuralgia of the ear ganglion; Neurasthenia; Neural amyotrophy of Charcot-Marie-Tooth; Acoustic neuroma; Neuroma; Optic neuritis; Pharyngeal neuritis; Neuritis of the facial nerve; Neuritis; Obsessive-compulsive neurosis; Pharyngeal neurosis; Neuroses; Neurosis-like stuttering; Femoral nerve neuropathy.
General concept
Neural amyotrophy of Charcot-Marie-Tooth is a chronic disease of the body that has a hereditary type of formation. A characteristic indicator is damage to the peripheral nervous system. Abnormal processes are manifested in the formation and changes in structure in muscle areas, for example: a decrease in the size of areas at the beginning of the lower extremities, and then the upper ones. In combination with this type of anomaly, the patient may experience hypoesthesia and a decrease in the reflex ability of the tendons, twitching of different parts of the muscles.
Doctors resort to various options for examining a patient with this disease, these include: electromyography, electroneurography, genetic testing, DNA testing, biopsy of nerves and muscle areas. There are no radical treatment methods, but there are methods aimed at ridding a person of symptoms. Doctors prescribe a variety of vitamin complexes, anticholinesterase methods, metabolic techniques, microcirculatory analogues, exercise therapy, physiotherapy, etc.
Treatment of Charcot's disease
All methods of treating Charcot-Marie-Tooth disease are not radical. Symptomatic treatment includes drug therapy, physical therapy, treatment by an orthopedist, etc.
Physiotherapeutic treatment of Charcot-Marie-Tooth disease includes exercise therapy, massage, electrophoresis, diadynamic therapy, therapeutic mud therapy, various types of baths, etc.
Drug therapy is aimed at improving the nutrition of muscle fibers. For this purpose, cocarboxylase, glucose, adenosine triphosphate, etc. are prescribed. Antioxidants, drugs that improve microcirculation, and vitamins are also widely used. Well-proven drugs that inhibit the activity of acetylcholinesterase and increase the level of acetylcholine, for example, prozerin, galantamine.
Further development of new drugs aimed at radical measures is a world without Charcot-Marie-Tooth disease. The progression of Charcot-Marie-Tooth disease does not affect how long patients live.
At the Yusupov Hospital, specialists have been helping patients keep their disease under control for many years. The minimal severity of symptoms and slow progression are the result of the work of doctors. In comfortable rooms, on new simulators, in well-equipped offices - this is where Charcot-Marie-Tooth disease is treated. Don’t delay treatment, sign up for a consultation.
Useful information
Neural amyotrophy Charcot-Marie-Tooth (CMT) is included in the list of chronic diseases (polyneuropathies) of a genetic nature that manifest themselves in increased progression. These include:
- Roussy-Lévy syndrome.
- Hypertrophic neuropathy Dejerine-Sotta.
- Refsum's disease and other rarer pathological processes.
According to the average statistical data, scientists state that almost 83% of cases are caused as a result of a person’s hereditary predisposition. Adverse effects in the body occur mostly in men; women are less susceptible to the described disease. Referring to numerous data, neural amyotrophy CMT is diagnosed with a frequency of two to thirty-six cases per hundred thousand of the planet's population. Usually, it is of a family nature. However, among members of the same family, clinical symptoms may be expressed differently. At the same time, doctors also observe sporadic variants of CMT. Medical staff note a clear relationship with Friedreich loss of coordination. Some patients in different situations experience typical symptoms of one or another disease. Sometimes, over many years, the symptoms of one anomaly may be replaced by the symptoms of another.
Causes
Genetic diseases are determined by the combination of genes for a particular trait that are found on chromosomes received from the father and mother.
A person who receives one normal gene and one disease gene is a carrier but usually does not show symptoms.
- The risk for two carrier parents of passing the defective gene to their children is 25%.
- Having a child who is a carrier -50%.
- The chance for a child to receive normal genes is 25%.
The risk is the same for men and women.
Dominant genetic disorders occur when only one copy of the abnormal gene is needed to cause the disease. The abnormal gene may be inherited from either parent or be the result of a new mutation (gene change).
The risk of passing the abnormal gene from the affected parent to the offspring is 50% for each pregnancy, regardless of the sex of the child.
X-linked dominant genetic disorders are caused by an abnormal gene on the X chromosome. Men with the abnormal gene are more severely affected than women.
Hereditary neuropathy is divided into several types called CMT1, CMT2, CMT3, CMT4 and CMTX.
CMT1
It is the dominant form of the disorder in which nerve conduction velocities are slow. More common than CMT2. Caused by abnormal genes that are involved in the structure and function of myelin. Further subdivided into CMT1A, CMT1B, CMT1C, CMT1D, CMT1X based on specific abnormalities.
- CMT1A occurs due to duplication of the PMP22 gene, which is located on chromosome 17 at 17p11.2. Is the most common type.
- CMT1B is caused by abnormalities in the MPZ gene on chromosome 1 at 1q22.
- CMT1C arises from abnormalities of SIMPLE, located on chromosome 16 at 16p13.1-p12.3.
- CMT1D abnormality of EGR2 located at 10, at 10q21.1-q22.1.
- CMT1X arises from mutations in GJB1 (Xq13.1). It encodes the junction protein connexin32.
Find out more What is Sheehan syndrome?
CMT2
Is an autosomal dominant form of the disorder in which nerve conduction velocities are usually normal or slightly slower than normal. Caused by abnormal genes involved in axonal structure and function. Further subdivided into CMT2A-2L based on mutations.
- CMT2A, is the most common and is caused by errors in MFN2, located on chromosome 1, at 1p36.2.
- CMT2B from RAB7 mutations on chromosome 3 at 3q21.
- CMT2C is caused by an unknown gene on 12 – 12q23-34.
- CMT2D GARS errors, on 7 – 7p15.
- CMT2E from NEFL located at 8 – 8p21.
- CMT2F HSPB1 gene errors.
- CMT2L mutations of HSPB8.
Dominant intermediate DI-CMT. It is so named because of the "intermediate" conduction velocity, the uncertainty as to whether the neuropathy is axonal or demyelinating. Dominant mutations in DMN2 and YARS are known to cause this phenotype.
CMT3
Also called Dejerine-Sottas disease, individuals with this disorder have a mutation in one of the genes responsible for CMT1A, CMT1B, CMT1D, CMT4.
CMT4
An autosomal recessive form of the condition. It is divided into CMT4A, CMT4B1, CMT4B2, CMT4C, CMT4D, CMT4E, CMT4F.
- CMT4A is caused by abnormalities of GDAP1. The gene is located on chromosome 8 at 8q13-q21.
- CMT4B1 is an abnormality of MTMR2 on 11 – 11q22.
- CMT4B2 from SBF2/MTMR13 anomalies, at 11 at 11p15.
- CMT4C errors KIAA1985, on chromosome 5 – 5q32.
- CMT4D mutations NDRG1, on chromosome 8 – 8q24.3.
- CMT4E, also known as congenital hypomyelinic neuropathy. Occurs from EGR2 abnormalities, on 10 – 10q21.1-q22.1.
- CMT4F PRX abnormalities, on chromosome 19 – 19q13.1-q13.2.
- CMT4H FDG4 errors.
- CMT4J mutations FIG4.
However, most cases of CMT2 are not caused by mutations in these proteins, so many genetic causes have not yet been discovered.
CMTX
It is an X-linked dominant form of the disorder. CMT1X accounts for about 90% of cases. The specific protein responsible for the remaining 10% of CMTX has not yet been identified.
Autosomal recessive CMT2 occurs due to mutations in LMNA, GDAP1.
Structural alignment with secondary structure elements on top. The ten mutations causing CMT are indicated by vertical arrows. (Click to enlarge)
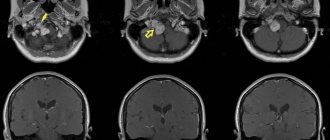
Pathogenesis of neural amyotrophy Charcot-Marie-Tooth
In medicine at the moment there is no accurate and reliable information about the origin and mechanism of neural amyotrophy. According to the experiments, it became clear only that in almost 75% of patients with this diagnosis who underwent genetic consultation, a repetition of a certain zone of the 17th chromosome was identified. It is already known that the disease has several groups, caused by various gene mutations. For example, during a study of a patient with CMT, which manifests itself due to a mutation in the MFN2 gene protein, mitochondria particles begin to appear. As a result, a person experiences a disruption in the movement of these elements along the axon.
A large number of forms appear due to damage to the myelin outer layer of fibers. Much less often you can notice forms with deviations from the norm of axons - objects of axial direction that pass in the central part of the nervous structure. Abnormal processes can affect the condition of the anterior and posterior processes of the spinal cord, neurons of the anterior horns, Gaulle's pathways and Clark's columns. Again, due to problems with the functioning of the peripheral region, muscle insufficiency begins to form.
Varieties and classification
In the neurological direction of medicine, neural amyotrophy of Charcot-Marie-Tooth is divided into two clear groups, which are clinically quite similar to each other, but have a list of features that allow such a distinction to be made:
- Neural amyotrophy type I - causes a decrease in the speed of nerve impulses.
- ON type II - speed is adversely affected to a lesser extent, neurite deviation is manifested.
How to diagnose CMT?
The doctor will ask about your family history and look for signs of muscle weakness - decreased muscle tone, flat feet, or high arches (cavus).
Nerve conduction studies measure the strength and speed of electrical signals that travel through nerves (electromyography). Electrodes are placed on the skin and deliver mild electric shocks that stimulate the nerves. A delayed or weak response suggests a neurological disorder, and possibly CMT.
With electromyography (EMG), a thin needle is inserted into the muscle. When the patient relaxes or contracts the muscles, electrical activity is measured. Testing different muscles will show which one is suffering.
Genetic testing is done using a blood sample that can show whether a patient has gene mutations.
What are the manifestations of Charcot-Marie-Tooth neural amyotrophy?
With the described disease in humans, the first thing that begins is the formation of similar muscle necrosis in the lower extremities. The first manifestations, as a rule, occur at the age of twenty (much less often, doctors can diagnose symptoms in adolescence from 16 years, and also up to 30 years). Such manifestations consist mainly of a high degree of fatigue of the legs during a long stay in an upright position. The so-called “trampling” syndrome has been noticed, that is, in order for the patient to relieve discomfort, he begins to walk in place. In some rare situations, AN manifests itself as a disorder of the sensitivity of the same parts, most often - paresthesia is formed in the form of crawling goosebumps.
A typical early sign of cervical mastication is the complete absence of Achilles and patellar tendon reflexes. As a result, the patient develops a drooping arch, an inability to walk on his heels, and an abnormal gait that is similar to that of a horse. Subsequently, the harmful process increases the degree of progression further and affects the muscles and flexors. The maximum level of necrosis can lead to complete deformation of the legs with a high arch, similar to the Friedreich foot type. Gradually, CMT moves to the proximal areas, which include the legs and lower thighs. The patient begins to develop serious deformities: drooping feet, legs becoming abnormally shaped. Next, the hands are affected, the hand becomes like a monkey's paw.
It is worth knowing that harmful lesions never affect the muscles of the cervical perimeter, torso and shoulder area. In addition to the above symptoms, the patient may experience the following problems:
- Faint twitching.
- Hypertrophy of the compensatory nature of muscle areas.
- Sensory impairments.
- Possibility of cyanosis and swelling of the skin.
CMT typically develops symptoms slowly. The period of development of the process of reduction in the size of the legs and arms can take up to ten years. Even with such serious deformations of the body, the patient is able to maintain working capacity for a long time and normally perform various household duties. The following factors may precipitate symptoms:
- Entry of infectious agents into the body.
- Long stay in the cold.
- Head injuries.
- Damage to the back and spinal cord.
- Lack of vitamins in the body.
Symptoms of CMT in adults
- Weakness in the muscles of the legs and ankles;
- Curvature of toes;
- Difficulty lifting the foot due to weak ankle muscles;
- Numbness in the arms and legs;
- Change in the shape of the lower leg, with the leg becoming very thin below the knee, while the thighs retain normal muscle volume and shape (stork leg);
- Over time, the arms become weaker and patients find it difficult to perform daily tasks;
- Pain in the muscles and joints appears, and it is difficult for a person to walk. Neuropathic pain occurs due to damaged nerves;
- In severe cases, the patient may need a wheelchair, while others may use special shoes or other orthopedic devices.
Diagnostic options
To diagnose Charcot-Marie-Tooth AN, medical workers rely on such manifestations as:
- The age at which the first signs of the disease appeared.
- Standard clinical picture.
- Similar nature of destruction of the body.
- Slow degree of development of atrophies.
- Increased risk of symptoms.
During a visit to a specialist’s office, a person will undergo a full examination of the body to identify the presence of muscle weakness in the feet and legs, changes, absence or serious decrease in the level of reflex abilities of the Achilles and knee region, hypoesthesia. In order to distinguish CMT from other neuromuscular disorders, doctors create a series of examinations that the infected person will need to undergo. These include:
- Electromyographic study.
- Electroneurography.
- Analysis of blood cells for sugar, hormonal levels and narcotic substances.
- Consultation with a specialist in the field of genetics.
- DNA assessment or genome sequencing (the latter option is very expensive for widespread use).
- Biopsy.
Symptoms
Charcot Marie Tooth disease can manifest itself in different ways and the main thing is to recognize the development of the disease in time. This is necessary in order to contact a medical facility in a timely manner.
If the patient is bothered by some signs, it is not recommended to ignore the symptoms and visit a doctor. In children, the disease practically goes unnoticed, so pathology can only be detected in a child over 14 years of age.
The main symptoms during the development of the disease:
- The legs begin to get tired quickly and it is easier for the patient to walk in place than to just stand.
- It is noticeable how the sensitivity of the lower extremities decreases and goosebumps are felt throughout the body.
- If the pathology is in an advanced form, then muscle atrophy may occur. The muscles in the leg may become smaller in volume. If you look closely at the lower limbs, you can see how they have become shaped like an inverted bottle. Deformation of the feet may occur.
- Often an abnormal gait occurs and the patient may walk and raise his knees high.
Neural amyotrophy can develop unnoticed and slowly. If hereditary Charcot-Marie-Tooth neuropathy has been progressing for a couple of years, then the patient may have damage to the nerve tissues of both the arms and legs.
Intermittent dystrophic syndrome occurs most often in the forearm and hands. The muscles of the trunk are affected and atrophy occurs over time. This is when spinal deformity occurs.
Infections, intoxication and injuries can provoke an acceleration of pathology and worsen well-being. If even slight suspicions of neural amyotrophy become noticeable, then you should not hesitate and consult a doctor.