More detailed information about other diseases starting with the letter “R”: Radiation damage to the nervous system; Multiple sclerosis; Radiculitis; Spina bifida; Disseminated encephalomyelitis; Retrobulbar neuritis; Retinal migraine
What is retrobulbar neuritis?
Retrobulbar neuritis is an inflammatory disease that affects the optic nerve, located between the orbit and the visual area. If there is an anomaly, the patient experiences a decrease in the level of visual acuity, the occurrence of prolapses, minimization of boundaries, and painful sensations during motor reflexes with the eyeballs. As research methods, doctors use complex neurological and ophthalmological techniques. Therapeutic therapy is performed using antibacterial/antiviral medications, glucocorticosteroids, diuretics and neuroprotective drugs. In some cases, detoxification procedures and physical therapy are prescribed.
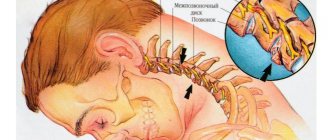
What is the optic nerve
As mentioned above, with retrobulbar neuritis the optic nerve is affected. It consists of bundles of fibers that are separated from each other by myelin.
In this article
- What is the optic nerve
- Forms of retrobulbar neuritis
- Causes of optic neuritis
- Signs of retrobulbar optic neuritis
- How is retrobulbar neuritis diagnosed?
- Retrobulbar optic neuritis: treatment
- Possible complications of optic neuritis
They penetrate the sclera, where they are surrounded by meningeal formations that form the nerve trunk.
The optic nerve is necessary for transmitting impulses associated with the perception of color, shadow and light, objects.
Useful facts
Typically, retrobulbar neuritis acts as a secondary consequence after any abnormality occurring in the brain. In very rare situations, the disease is diagnosed as a primary true inflammatory process. In the neurological field, doctors are still studying the issue of this disorder in detail. Neuritis that is localized in the intraorbital region is called intrabulbar (it is examined by ophthalmologists). In both cases, therapy requires a joint solution of the problem between the neurologist and the ophthalmologist. The risk group includes people aged 20 to 40 years. According to average statistics, this type of disease occurs twice as often in females as in males.
CLINICAL AND DIAGNOSTICS OF RETROBULBAR NEURITIS
Ivanov V.T.
State Healthcare Institution Lipetsk City Hospital No. 4 “Lipetsk-Med”, Russia, Lipetsk
Kutashov V.A., Ulyanova O.V.
FSBEI HE VSMU named after. N.N. Burdenko of the Russian Ministry of Health,
Department of Psychiatry and Neurology, IDPO, Russia, Voronezh
Annotation.
Multiple sclerosis (MS) is one of the most complex complex and global medical and social problems. There are currently at least 150,000 sick people living in the country, at least 50% of whom are already disabled. In recent years, there has been a steady trend towards an increase in the incidence of MS, including in the North-West of the Russian Federation, as well as a rejuvenation of this contingent of patients. The reason for this was not only improved diagnosis of the disease, but also improved quality of epidemiological studies, as well as a real increase in incidence.
The article describes the main clinical manifestations and methods for diagnosing damage to the optic nerve in demyelinating diseases. The main directions of treatment for patients with MS are identified.
Keywords
: demyelinating disease, young age, multiple sclerosis, retrobulbar neuritis, central nervous system.
Relevance of the problem
. Multiple sclerosis (MS) is a demyelinating disease of the nervous system (NS), affecting mainly young people aged 20 to 40 years and characterized by polymorphism of clinical forms, diversity of course and early stages of disability [3, 5, 8, 9, 14, 15] .
The ambiguity of many issues of the occurrence and mechanisms of development of the disease, the difficulties of diagnosis in the early stages, the variety of clinical variants of the course with rapid disability, the lack of effective treatment methods - all this is the urgent task of modern medicine. According to European and American organizations, MS is the most expensive chronic neurological disease (per patient over a lifetime) for the state and private insurance companies. Currently, there are about 3 million MS patients in the world. In Russia, the incidence of MS ranges from 30 to 100 cases per 100,000 population [3, 5, 8, 9, 13, 14, 15]. A feature of the clinical course of MS is that in most patients, especially in the early stages of the disease, higher nervous activity (HNA) suffers to a minimal extent, as a result of which patients retain the ability to actively influence the solution of work, home and social problems. At the same time, the condition of MS patients significantly depends on their psycho-emotional mood. Social isolation, the inability to actively participate in the life of society, awareness of one’s “uselessness” and lack of demand adversely affect the course of the disease and lead to psychological maladaptation of patients (according to statistics, the number of suicide attempts in the group of MS patients is 7.5 times higher than in healthy people of people). In this regard, MS patients need constant highly qualified specialized medical care with the involvement of both neurologists and psychologists, urologists, speech therapists, physiotherapists, neuro-ophthalmologists, gynecologists, surgeons, therapists and doctors of other specialties specially trained in MS problems [8, 9, 13 ].
Continuous dynamic outpatient monitoring and periodic hospitalization are required to prevent and treat exacerbations and complications in patients with this disease. The solution to many problems faced by patients with MS entirely depends on the prompt use of adequate medical care in the early stages of the disease, when work capacity and social functions are preserved or slightly impaired [3, 5, 8, 9, 13, 14, 15].
Diagnostics
MS is based primarily on the clinical characteristics of the manifestation of the pathological process in the central nervous system (CNS). However, additional diagnostic methods, which include magnetic resonance imaging (MRI) and cerebrospinal fluid examination (isofocusing of oligoclonal immunoglobulins) can provide significant assistance in controversial cases [3, 4, 5, 7, 8, 9, 10, 11, 12. 13, 14, 15].
Retrobulbar neuritis
– usually not an independent disease, but a manifestation of an autoimmune process (one of the earliest symptoms of MS) or a neuroinfection with damage to the optic nerve (ON). The optic nerve is a connection of more than 1 million sensory processes or axons of retinal nerve cells that transmit information about the perceived image in the form of electrical impulses to the brain. In the occipital lobe of the brain, this information is finally processed and the person gets the opportunity to see everything that surrounds him. According to studies, MN lesions were found in 24 (38%) patients who, according to medical history, had retrobulbar neuritis (RBN) at the onset of MS [1, 2, 7].
This is a symptom of acute damage to the optic nerve in the area from the eyeball to the chiasm at the onset of PC development. RBI was observed much more often in women than in men (91.6% and 8.3% of cases, respectively). The average age of onset of RBN is 25 – 29 years. Retrospectively, according to the anamnesis, it was found that with the development of acute RBN, patients complained of a sharp decrease in visual acuity in one eye: right - 5 (21.0%) people, left - 16 (66.7%). Bilateral RBI occurred in 3 (12.5%) patients. Patients noted that suddenly, often in the morning, after sleep, a “spot” appeared in front of the eye or a feeling that “he was looking through gauze.” In 6 (25.0%) people, visual impairment was accompanied by pain in the retrobulbar region (RBR). According to medical documentation, all patients were diagnosed with RBN by an ophthalmologist, 19 (79.2%) of them were examined by a neurologist during the acute period of RBN and a conclusion was made about probable MS [1, 2, 6, 7, 10, 12, 14] .
In MS, the lesion of the optic nerve is determined by its morphological feature. This nerve, along with the olfactory nerve, is essentially a reduced lobe of the brain; in its structure it is closer to the conductors of the central nervous system than to the spinal nerves [1, 5, 6, 7, 8, 9, 10, 11, 12, 14, 16 , 17 , 18 , 19 , 20 ].
Currently, there is a widespread division of inflammatory diseases of the optic neuritis into optic neuritis (ON neuritis, ON) and retrobulbar neuritis (RBN).
ON is that form of inflammation when the inflammatory process also involves the disc of the optic nerve. In this regard, in case of optic neuritis, ophthalmoscopy always reveals changes in the optic disc. In contrast, PPH is an inflammation of the optic nerve behind the eyeball that does not extend to the n disc. opticus. In such cases, there are no changes in the fundus. Essentially, in PH, the inflammatory process can involve peripheral and central bundles of nerve fibers. In accordance with this, 2 types of changes can be observed in the visual field: narrowing of the boundaries in the absence of changes in the central part of the visual field; appearance of central scotomas. Often, RPH is still accompanied by mild inflammatory changes in the MN disc [1, 2, 5, 6, 7, 14, 15, 16].
Clinical picture
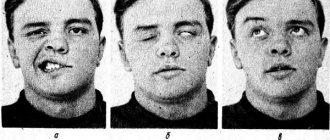
ON is characterized by an acute decrease in vision down to color perception, which may be preceded by attacks of “fogging” for several hours [2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 13, 14, 15, 17, 18 , 20 ]. Decreased vision is usually caused by the appearance of a central scotoma (90% of cases), paracentral scotoma, a narrowing of the visual fields by 10-30% and is often accompanied by a change in color vision with loss of tone and color, a predominance of gray, a narrowing of the visual fields to red and green color. Changes in visual fields can be very diverse. Depending on whether the inflammation involves peripheral fibers or penetrates deeper into the nerve trunk, either a slight narrowing of the visual fields or narrowing of the boundaries with sharply irregular outlines (when the inflammatory process penetrates especially deeply into the thickness of the nerve trunk) may be observed. During exacerbation of PC, the process of demyelination may involve optic fibers in one or another part of the chiasm. Changes in visual fields in such cases vary widely [3, 4, 5, 7, 8, 9].
PPH is accompanied by pain in the area of the eyeball, which intensifies with movement or pressure, especially when looking up, which is associated with irritation of the optic membranes when the superior and internal rectus muscles are tense [1, 2, 3, 6, 7, 8, 10, 11, 13 , 14 , 15 , 16 , 19 , 20 ].
A characteristic feature of PC according to D.A. Markov and A.L. Leonovich (1976) is the phenomenon of " clinical splitting
", or the syndrome of "
clinical dissociation
" - a discrepancy between the degree of preservation of function and pronounced changes in objective data. For example, the presence of normal visual acuity and detection of signs of partial atrophy of the optic disc in the fundus [1, 2, 5, 6, 7, 9, 10, 11, 12, 14, 16, 17, 19, 20].
For the diagnosis of MS, a very important criterion is the detection of foci of demyelination in the central nervous system - “plaques” in the brain and spinal cord, as well as thinning of the ganglion fibers of the optic nerve with a decrease in their layer by 8-33% [3, 4, 5, 8, 9, 10 , 12 , 13 , 14 , 15 ]. Also, the process of demyelination of the optic nerves can be detected by topographic scanning of the retina. Until now MRI
is the most informative paraclinical method for diagnosing MS.
The presence of characteristic changes on MRI can serve as an important prognostic criterion for the likelihood of developing definite MS at the onset of demyelinating lesions of the central nervous system (the so-called clinically isolated syndrome
- CIS), as well as for predicting the rate of development of disability in patients with definite MS [3, 4, 5, 7, 8, 9, 10, 11, 12, 13, 14, 15]. In order to obtain a clearer image and increase resolution, high-field MR tomographs (1.5; 3 Tesla) are used. High-field MRI is safe for patients and allows more detailed examination of focal changes in the brain in patients with MS [3, 4, 5, 8, 9, 14, 15, 16, 19, 20].
Foci of demyelination can be detected when examining the fundus of the eye using a fundus camera (linear areas of clearing and darkening, fan-shaped from the optic nerve head along the vessels). Important methods for assessing the functional state of the degree of preservation of the visual pathways, as well as for localizing the level of the pathological process, are electroretinography (ERG) and the method of visual evoked potentials (VEP). VEPs complement ERG data, and are also the only source of information in cases where ERG cannot be registered for one reason or another [1, 2, 5, 6, 7, 11, 12, 13, 14, 15, 16, 17, 18. 19, 20].
When analyzing VEPs, the shape is mainly taken into account, the amplitude (μV) and the time to wave peaks (ms). The difference in its latency when stimulating the right and left eyes (interocular difference in latency and amplitudes), interhemispheric asymmetry, paradoxicality of VEP lateralization. When determining subclinical lesions of the visual pathways, a sensitive test is to determine the latency time of the VEP - an increase in the latency of the component is the earliest and most stable sign of damage to the optic nerve, occurring even before the clinical manifestations of the disease. As the disease progresses, an increase in the latency period is observed (by 30–35% of normal values) with a simultaneous decrease in amplitude and a change in the configuration of the response. The amplitude and configuration of VEP can gradually normalize with the restoration of visual functions, while the temporal characteristics continue to remain increased after normalization of clinical parameters. Demyelination of the optic nerve is indicated by an increase in retinocortical time with a preserved ERG pattern and an increase in the time parameters of VEP. With severe axonal lesions with retrograde degeneration of optic nerve fibers, a sharp decrease in amplitude or absence of ERG pattern is observed in combination with changes in VEP. With partial atrophy of the optic nerves, a decrease in amplitude and an increase in the latency period of P are observed. These changes can occur independently of each other. The absence of VEP indicates atrophy of the optic nerve, failure of the visual pathways and centers [1, 2, 4, 5, 6, 7, 10, 11, 12, 14, 15, 16, 17, 18, 19, 20].
MS treatment
is one of the most pressing and complex problems of modern neurology. The drugs available to doctors can only reduce the frequency and severity of exacerbations, as well as slow down the rate of accumulation of neurological deficits, which is confirmed by positive dynamics according to MRI data of the brain and spinal cord [3, 4, 7, 8, 9, 11, 12, 13]. One of the key problems in the treatment of MS is the creation and clinical trial of new drugs that block the development of brain atrophy, inflammation and demyelination, reduce the frequency of exacerbations, and prevent the progression of disability.
The modern standard for treating exacerbations of the disease is high-dose pulse therapy with methylprednisolone 1 g daily for 3–5 days, intravenously. It is possible to administer intramuscular dexamethasone for 7–14 days or take oral prednisolone for up to 30 days [1, 3, 4, 5, 6, 8, 9, 10, 11, 12, 13, 14, 15]. In the case of hormonal therapy administered intramuscularly or orally, the patient (insurance company or government) faces fewer material costs, but recovery occurs much later, which can significantly increase indirect costs.
To prevent exacerbations and prevent progression of the disease, five drugs from the DMT group (drugs that modify the course of MS) with proven effectiveness are currently widely used. It has been shown that these drugs can be used effectively not only during relapsing-remitting MS, but also in the early stages of MS (clinically isolated syndrome - CIS), and during secondary progression with exacerbations; the peculiarities of action and tolerability of each of them leave a wide opportunity for individual selection. mitoxantrone remains the only drug
. Evidence of a long-term sustainable effect of these drugs was obtained both clinically and using MRI over time. The main effects of DMTRS: 1) reduction in the frequency of exacerbations (by 25–30% compared to placebo in randomized trials, by 60–70% compared to the period before treatment in open observations); 2) slowing down the rate of progression of irreversible disorders (disability); 3) reduction in the activity of the inflammatory reaction, demyelination and neurodegeneration (the latter to a lesser extent) according to MRI data [1, 4, 5, 6, 7, 8, 9, 12, 13, 14, 15, 16, 17, 18].
Conclusion.
Thus, it is necessary to consider RBN as one of the earliest manifestations of MS, the timely diagnosis of which significantly facilitates the diagnosis and helps determine the correct tactics for further treatment of this group of patients.
Bibliography
1. Averyanov D.A., S.L. Alpatov. In V. Bukin et al. / Ed. L.G. Shchuko. V V Malysheva. Optical coherence tomography in ophthalmology. ‒ Irkutsk. 2005. - 112 p.
2. Avetisov S.E.. E. L. Egorov. L.K. Moshegova and others. Ophthalmology. National leadership. ‒ M.: GEOTAR‒Media. 2011.‒ 44 p.
3. Gusev E.I., Boyko A.N. Demyelinating diseases of the central nervous system//Consilium Medicum. ‒ 2002. ‒ No. 2. ‒ P. 12‒18
4. Gnemitsky V.V. Shamshinova AM Experience in the use of evoked potentials in clinical practice. ‒M.: MBNyu, 2001.‒472 p.
5. Gusev E.I. Multiple sclerosis and other demyelinating diseases. ‒ M.: Miklos. 2004. - 540 p.
6. Guseva M.R. Clinic and diagnosis of optic neuritis in children with multiple sclerosis // Rus.med. magazine. - 2001. - T.2. No. I. ‒ P. 6‒12.
7. Guseva M.R. Results of clinical and immunological examination for optic neuritis in children with definite multiple sclerosis // Neurological Journal. ‒ 1999.‒Х®5.‒С. 10-15.
8. Esaulenko I.E., Chernov A.V., Ulyanova O.V., Kutashov V.A. Basic principles of providing neurological care to patients with multiple sclerosis in a multidisciplinary city hospital (30 years of experience) / I.E. Esaulenko [and others] // Journal “Bulletin of Neurology, Psychiatry and Neurosurgery”. - Moscow. ‒ 2021. – No. 7. – P. 37 – 41.
9. Kutashov V.A., Ulyanova O.V., Khabarova T.Yu., Budnevsky A.V. Cognitive impairment in multiple sclerosis / V.A. Kutashov [etc.] // Saratov Medical Scientific Journal. ‒ 2021. ‒ T. 12, No. 2. ‒ P. 267 ‒ 270.
10. Manoilova I.K. On the outcomes of retrobulbar neuritis in young patients in the short and long term // Ob. tr. scientific-practical anniversary and conf. having eaten, in memory of T.I. Broshevsky. Saint Petersburg. 2005 - St. Petersburg. 2005.‒C 480‒483
11. Nikiforov A.S.. Guseva M.R. Nsyroofhalmology: a guide. ‒ M: GEOTAR‒Media. 2008. ‒ 624 p.
12. Throne E.Zh. Diseases of the visual pathway. ‒ Medgiz, 1968. ‒ 394 p.
13. Ulyanova O.V., Kutashov V.A., Dutova T.I. Multiple sclerosis is a pressing neurological problem of the 21st century / O.V. Ulyanova, V.A. Kutashov, T.I. Dutova // Young scientist. ‒ No. 15 (119) ‒ P. 558 ‒ 566.
14. Shamshinova A.M.. Volkov V.V. Functional studies in ophthalmology. ‒ M: Medicine. 2002. - 415 p.
15. Schmidt T.E.. Yakhno N.N. Multiple sclerosis: a guide for doctors. ‒ M: MEDIPRESS‒inform. 2010. ‒ 272 p.
16. Hubsll D. Eye. brain, vision. ‒ M.: Mir. 1990. - 239 p.
17. Cense B. Thickness and Birefringence of Healthy Retinal Nerve Fiber Layer Tissue Measured with Polarization‒ Scnsitivc Optical Coherence Tomography// Intestig. Ophthalmolog. Visual Sci. - 2004. - V.45. ‒ P. 2600‒2612.
18. Ccuomai D Reproducibility of Optical Coherence Tomography in Multiple Sclerosis // Arch. Neuol. ‒ 2008. V.65‒P. 1218‒1222.
19. Fisher JB Relation of Visual Function to Retinal Nerve Fiber Layer Thickness in Multiple Sclerosis // American Academy of Ophthalmology Annual Meeting. ‒ Chicago‒lllinois. 2005. ‒ P. 105‒109.
20. Houguaard JL Evaluation of Heredity as a Determinant of Retinal Nerve Fiber Layer Thickness as Measured by Optical Coherence Tomography // Intcstig. Ophthalmolog. Visual Sci. - 2003. - V.44. ‒ P. 3011‒3016.
Information about authors:
Ivanov V.T. –
State Healthcare Institution Lipetsk City Hospital No. 4 “Lipetsk-Med”, Russia, Lipetsk
Kutashov Vyacheslav Anatolievich
‒ Doctor of Medical Sciences, Professor, Head of the Department of Psychiatry and Neurology, Institute of Postgraduate Education, Voronezh State Medical University. N.N. Burdenko. [email protected]
Ulyanova Olga Vladimirovna
‒ Candidate of Medical Sciences, Associate Professor of the Department of Psychiatry and Neurology, Institute of Postgraduate Education, Voronezh State Medical University. N.N. Burdenko.
CLINIC AND DIAGNOSIS OF RETROBULBAR NEURITIS
Ivanov VT
GUZ Lipetsk City Hospital No. 4 “Lipetsk‒Med”, Russia, Lipetsk
Kutashov V.A., Ulyanov a
. O.V.
FGBOU in VGMU them. NN Burdenko
Abstract.
Multiple sclerosis (MS) is one of the most complex and global medical and social problems. Currently, the country is home to at least 150,000 patients, at least 50% of which are disabled. In recent years there has been a steady trend to increase the incidence of DCS, including in the North‒West Russia, as well as the rejuvenation of the patients [6]. The reason for this was not only improve the diagnosis of the disease, but also improving the quality of epidemiological studies, as well as the real increase in morbidity. The article describes the main clinical manifestations and diagnostic methods of lesions of the optic nerve in demyelinating diseases. The basic directions of treatment of patients RS.
Keywords:
demyelinating disease, young age, multiple sclerosis, retrobulbar neuritis, Central nervous system.
Bibliography
1. Averyanov DA, SL Alpatov. In V. Bukin, etc. / Under the editorship of LG Shchuko. In Malysheva. Optical coherence tomography in ophthalmology. ‒ Irkutsk. 2005. ‒ 112 p.
2. Avetisov SE. E L. Egorov. L. To Moshegov etc. Ophthalmology. National leadership. ‒ M.: GEOTAR‒Media. 2011.‒ 44 p.
3. Gusev EI, Boyko AN Demielinizirute Central nervous system diseases//Consilium Medicum. ‒ 2002. ‒ No. 2. ‒ P. 12-18
4. Gramicci In In . Shamshinova am the Experience of application of evoked potentials in clinical practice. ‒M.: Mbny, 2001.-472 S.
5. Gusev, EI, Multiple sclerosis and other demielinizirutaya disease. ‒ Moscow: Miklosh. 2004. ‒ 540 p.
6. Guseva MR clinic and a diagnosis of optic neuritis in children with multiple sclerosis // Rus.med. log. ‒ 2001. ‒ T. 2. No. ‒ P. 6-12.
7. Guseva MR the Results of clinical and immunohistologic examination in optic neuritis in children with reliable multiple sclerosis // Neurological journal. ‒ 1999.‒X®5.‒S. 10-15.
8. Esaulenko IE, Chernov AV, Ulyanova OV, Kutashov VA the Main principles of providing neurological care to patients with multiple sclerosis in a multi-profile city hospital (30 years experience) / Esaulenko IE // Journal “journal of neurology, psychiatry and neurosurgery". ‒ Moscow. ‒ 2021. – No. 7. – P. 37 – 41.
9. Kutashov VA, Ulyanova A., Khabarova TY, Budnevsky AV Cognitive impairment in multiple sclerosis / VA Kutashov // Saratov scientific medical journal. ‒ 2021. ‒ Vol. 12, No. 2. ‒ P. 267 ‒ 270.
10. Manoilova IK About the outcomes of retrobulbar neuritis in young patients in early and late periods //On. Tr. scientific.‒pract. anniversary I. proc. after eating, the memory of TI Broshevskiy. Saint‒Petersburg. 2005 - SPb. 2005.‒With 480-483
11. Nikiforov A.C. Gusev MR Siraichalai: a guide. ‒ M: GEOTAR‒Media. 2008. ‒ 624 p.
12. Throne, JE diseases of the visual pathways. ‒ Medgiz, 1968. ‒ 394 p.
13. Ulyanova OV, Kutashov VA, Dutova TI Multiple sclerosis is a neurological actual problem of the XXI century / OV Ulyanova, VA Kutashov, TI Dutova // Young scientist. ‒ No. 15 (119) - Pp. 558 ‒ 566.
14. Shamshinova AM Volkov VV Functional studies in ophthalmology. ‒ M: Medicine. 2002. ‒ 415 p.
15. Schmidt TE. Yakhno NN Multiple sclerosis: a guide for physicians. ‒ M: Medpress‒inform. 2010. ‒ 272.
16. D. Hubell Eyes. brain, vision. ‒ M.: Mir. 1990. ‒ 239 p
17. V. Cense Thickness and Birefringence of Healthy Retinal Nerve Fiber Layer Tissue Measured with Polarization‒ Scnsitivc Optical Coherence Tomography // Intestig. Ophthalmolog. Visual Sci. ‒ 2004. ‒ V. 45. ‒ P. 2600-2612.
18. Ccuomai D Reproducibility of Optical Coherence Tomography in Multiple MS // Arch. Neuol. ‒ 2008. V. 65‒P. 1218-1222.
19. Fisher, JB Relation of Visual Function to Retinal Nerve Fiber Layer Thickness in Multiple MS // American Academy of Ophthalmology Annual Meeting. ‒ Chicago‒lllinois. 2005. ‒ P. 105-109.
20. Houguaard JL Evaluation of Heredity as a Determinant of Retinal Nerve Fiber Layer Thickness as Measured by Optical Coherence Tomography // Intcstig. Ophthalmolog. Visual Sci. - 2003. - V. 44. - P. 3011-3016.
Factors causing retrobulbar neuritis
Various problems provoke the development of abnormal vision impairment. Inflammation itself begins as a result of damage to the body by infectious diseases, chronic diseases caused by immunodeficiency. Etiological reasons include:
- Chronic stages of viral infections - the main causative agent is cytomegalovirus, which provokes the development of mononucleosis. The stable location of harmful agents causes deformations in immune properties. Due to the production of antibodies for one's own tissues, the process of autoimmune inflammation begins.
- Chronic infectious points - most often the anomaly is caused by unfavorable foci that are located nearby (for example, sinusitis, otitis media and others), much less often - by distant places (cystitis). The infection enters the nervous structure of the visual apparatus through blood transportation.
- Inflammatory phenomena in the orbit - provocateurs are inflammatory processes. Spread occurs in two ways: hematogenous and perineural, which causes damage to the retrobulbar perimeter of the nerve. Quite often, total optic neuritis is diagnosed.
Secondary progression of optic nerve disorder begins as a result of an anomaly that is localized in the cerebral region. The main etiofactors include the following diseases:
- Multiple sclerosis - selective damage to the myelin sheath of nerve fibers moves to the optical areas, which causes an inflammatory reaction. Neuritis of a retrobulbar nature is considered the initial stage in more than 65% of cases of disease.
- Brain tumors - when voluminous tumors form in the area of the chiasm glioma, objects in another place begin to actively pressure the optic chiasm, disrupting the process of blood circulation in the body and metabolism in tissues. As a result, the patient develops symptoms of neuritis.
- Neuroinfections - Lyme disease, neuroAIDS, tuberculous meningitis can provoke abnormalities in the retrobulbar zone. Inflammatory phenomena are associated with the entry of infectious microorganisms into the body. In some cases, the disease may appear due to intoxication. Exogenous lesions are caused by the influence of toxic chemicals, methyl alcohol, iodine substances. Toxins appear as a result of dysmetabolic processes, renal failure or during pregnancy.
Causes of optic neuritis
The causes of this disease are still poorly understood. According to the results of one study, the main factor provoking the development of retrobulbar optic neuritis is genetics. Because of this predisposition, myelin proteins are mistakenly perceived as harmful, resulting in the accumulation of T cells and activation of immune defenses.
The risk of developing the disease is highest at a young age: the first symptoms occur in patients under 30 years of age. Retrobulbar neuritis appears especially often in women. Among the reasons that provoke the development of the disease are infectious and non-infectious factors. Primary inflammation can occur due to viral infections: herpes, infectious mononucleosis, etc. In addition, it can be caused by tonsillitis, tonsillitis and sinusitis. A separate group of diseases that cause inflammation of the optic nerve includes uveitis and chorioretinitis.
If there has been brain damage, secondary retrobulbar neuritis may occur. It can occur due to HIV infection, Lyme disease, and inflammation of the brain.
The vast majority of people with multiple sclerosis are diagnosed with secondary bulbar neuritis, which occurs due to a lack of myelin. At the same time, at first, atrophic processes in the myelin sheath are invisible: they can be difficult to detect even on MRI.
Signs of myelin atrophy are noticed approximately 5 years after the onset of the disease. In 50% of patients, demyelination of both visual pathways is noticed in the images; in approximately 37%, the process is noticeable only on one side; in the remaining patients, both pathways are intact.
Mechanism of occurrence
When examining the visual department, one can understand that the nerve contains a large number of fibers (more than a million), which begin their journey from the retina and end in the subcortical ganglia of the eye. Various forms of pathogens can cause serious disorders, for example: ischemia, inflammation and tissue destruction. As a result, the patient experiences detrimental changes that affect the functions of transmitting information from the retinal receptors that receive the external image.
The clinical picture appears as a decrease in the level of vision, impaired color perception, and loss of boundaries. If you ignore the doctor’s recommendations or completely refuse treatment, the patient begins to experience irreversible abnormalities that fill the cavities with connective tissue growths. The last stage of the disease leads to complete loss of visual abilities.
Symptoms of intrabulbar neuritis
Intrabulbar optic neuritis has an acute onset. The inflammatory process can be provoked by pathogens such as staphylococcus, streptococcus, influenza and herpes viruses. The infection penetrates the optic nerve through the vitreous and perivascular spaces. Inflammation of the nerve can be total or partial. Total inflammation is characterized by a sharp decrease in normal vision. With partial damage to the nerve, vision may remain normal, but paracentral and central scotomas of oval, round and arch-like shapes are noted. Patients also have reduced color vision.
All pathological changes are usually concentrated in the area of the optic nerve head. The disc itself is hyperemic, its shade merges with the background of the retina, its tissue is edematous, and the edema has a pronounced exudative character. The boundaries of the disc are blurred, and there is no excessive prominence. The fundus of the eye with this optic neuritis is poorly and unclearly visible. Hemorrhages can be seen on the disc, the veins are slightly dilated.
The acute period of the pathology lasts about 3-5 weeks, after which the swelling begins to gradually subside, the boundaries of the disc become clearer, and all hemorrhages resolve. As a result, recovery and complete restoration of normal vision are possible, even if the prognosis was initially unfavorable. However, if the disease is severe, the death of nerve fibers, their disintegration and gradual replacement by glial tissue is possible. The prognosis for the patient is unfavorable, since optic nerve atrophy occurs. The degree of atrophy varies from minimal to complete, which leads to a sharp deterioration of vision.
Types of neuritis
There are different types of symptoms, which depend solely on the location of the lesion (central or peripheral lobe). In neurology, retrobulbar neuritis is divided into three classes:
- Axial - a common form of inflammatory reaction, localized only in the axial fascicle, characterized by a sharp decrease in central visual acuity and the appearance of scotomas.
- Peripheral - originates in peripheral structures, accompanied by the formation of intrathecal fluid, which provokes pain. A narrowing of the optical fields is characteristic.
- Transversal - a detrimental anomaly progresses in the periphery or axial region and then reaches the diameter of the nerve center. The patient is completely blind.
Another area of division of retrobulbar neuritis depends on the variability of the course:
- Acute form - manifests itself in the rapid loss of visual acuity. Most often it is diagnosed in the primary version of the lesion, which is typical for young people.
- Chronic form - symptoms have a gradual scale of increase, which are caused by a cerebral disorder. Patients experience some periods of remission or exacerbation. There is a possibility of the acute form becoming chronic.
How does it manifest itself?
The main manifestations of the anomaly are various disturbances of optical perception. According to average statistics, in 60% of situations patients have vision problems. When diagnosing an acute form of neuritis, visual acuity decreases within a short time (from a couple of hours to two days), and in the chronic form it will take 7-14 days. Patients, talking about their sensations, report a “veil before their eyes” and “blurring of all objects”; some experience “light flashes”. The slow progression of the disease causes deterioration of visual adaptation at night.
Deformations of the optical boundaries provoke the appearance of dark dots before the eyes, narrowing the visible trajectory. They can be combined with a decrease in vision. Retrobulbar neuritis occurs with impaired color perception. Dychromatopsia is practically not noticed by patients, but is only detected during certain tests. Doctors say that more than 50% of patients complain of a feeling of pain in the area of the eye orbits, which increases with activity, in particular when turning their gaze upward.
Examination methods
The main goal of the diagnostic procedure is to make a correct conclusion with a clear identification of the etiology and the mandatory exclusion of the presence of multiple sclerosis in the patient. The study will require clarification of all symptoms, the rate of their development and previously experienced diseases, as well as full ophthalmological and neurological testing. Diagnostics:
- Visometric analysis helps determine vision loss; emerging problems can be corrected by wearing lenses.
- Color vision test - designed to accurately identify anomalies in the absence of changes in the optic disc.
- Perimetric scanning - scan the central, paracentral and peripheral sections.
- Ophthalmoscopy - looks for swelling, bleeding and the possibility of atrophy.
How to get rid of it?
Therapeutic measures for retrobulbar neuritis are based on an etiopathogenetic principle, which is selected taking into account the etiology of the disease. A secondary lesion requires elimination of the primary source, that is, removal of the tumor, therapy aimed at restoring immune abilities in multiple sclerosis, and getting rid of neuroinfections. The main treatment complexes include:
- Pharmacological antibiotics with a wide range of applications.
- Antiviral components.
- Introduction to a course of glucocorticosteroid therapy.
- To reduce swelling, diuretics and antihistamines are prescribed.
- A course of vitamin complexes (vitamins B and C, nicotinamide and others) is prescribed.
In case of toxic damage, detoxification will be required; for this, intravenous administration of saline solutions and dextran through a dropper is used. If the patient has no restrictions, it is recommended to carry out physiotherapeutic procedures.
Treatment method
In the mildest stage, optic neuritis goes away unnoticed on its own. But most often it cannot be done without the intervention of medications, including hospitalization, in case of serious complications. They mainly use drugs from the steroid group, which eliminate inflammation in the area of the optic nerve.
In order to begin treatment correctly, it is necessary to understand the causes and understand whether all the symptoms are correctly identified and adequately assessed. The stages of recovery and the category of necessary medications depend on this. Most often, it is impossible to determine all the causes at once, so doctors will act according to the established scheme:
- Prescribing penicillin antibiotics with a very wide range of action. It is prohibited to use drugs of the streptomycin group with this category.
- Treatment with sulfonamide-type drugs.
- Antihistamines.
- The use of local hormonal therapy.
- Complex therapy with the use of antiviral and antibacterial medications.
- Treatment based on established symptoms using detoxification-type medications and agents with the properties of improving metabolic processes and restoring the acidic environment.
- In later manifestations of optic neuritis and when nerve atrophy appears in the eye canals, antispasmodic drugs are prescribed that affect blood microcirculation in the vessels.