The causes of polyneuropathy are very different, but in general, the functioning of many individual nerves and the peripheral nervous system as a whole is disrupted. The disease manifests itself in damage to the legs (in most cases) and arms, leading to obstructed blood circulation. As a result, with polyneuropathy, muscle function deteriorates and the sensitivity of the affected organs is gradually lost. Such a disease requires drug treatment, but therapeutic exercises and, as far as possible, physical therapy (physical therapy) also help with this disease. But gymnastic exercises still prevail, since they concentrate on a specific diseased organ, they can be done while sitting, which is especially important for polyneuropathy of the legs.
Content:
- The essence of the disease
- Causes of leg damage
- Clinical symptoms, examination methods
- Treatment
Alcohol “hits” absolutely all structures of the body. One of the most sensitive is nervous tissue. It is because of its defeat that pathologies arise that, as it may seem, have nothing to do with the nervous system. These include leg failure due to alcoholism.
The essence of the disease
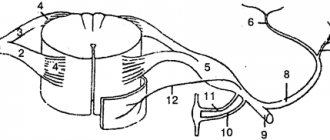
Ethyl alcohol and its metabolites (in particular, acetaldehyde) negatively affect both the neurons themselves and their membrane. In the first case, the function of the cells suffers, in the second the degree of protection deteriorates - they are damaged by pathological factors, and as a result, normal physiological processes in neurons are disrupted.
What category of diseases does leg failure in alcoholism belong to? What is it called according to terminology? Its presence indicates polyneuropathy - multiple damage to peripheral nerve endings.
Please note: Legs fail in every tenth alcoholic, according to other data - in every third. In the “chronicles,” even in the absence of symptoms, disturbances in nerve cells were observed in 9 out of 10 patients.
Males are affected more often.
Causes of the disease
The reasons for the development of such a pathology can be different, and certain symptoms appear.
The disease is insidious in that it disrupts the blood circulation process, which subsequently leads to loss of sensitivity in the affected parts of the body.
Exercise therapy for polyneuropathy can not only improve the patient’s general condition, but also reduce the severity of symptoms of the disorder.
Causes of leg damage
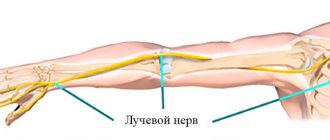
What is the mechanism of development of alcoholic polyneuropathy? It is caused by a violation of the sheath of the fibers that innervate the structures of the lower extremities. If the shell is absent, then the speed of impulse transmission through the neuron decreases by 5-24 times.
The immediate causes of alcoholic polyneuropathy of the lower extremities are:
- damage to nerve fibers by ethyl alcohol and its metabolite acetaldehyde;
- insufficient blood supply to neurons, which entails a deficiency of oxygen, proteins, fats, carbohydrates, mineral compounds and vitamins;
- lack of vitamin B1 in alcoholics. It, in turn, is provoked by poor nutrition (alcoholics often belong to socially disadvantaged segments of the population), failure of digestive processes and impaired liver function, which are observed in persons who abuse alcohol;
- compression of nerve fibers due to the fact that an alcoholic often sleeps in unnatural positions. If it is prolonged (more than 1 hour), then the blood supply to the nervous tissue is disrupted, it does not receive oxygen and nutrients, and in severe cases it can even become dead.
Clinical symptoms, examination methods
The symptoms of alcoholic neuropathy are as follows:
- pain;
- hypoesthesia (decreased sensitivity of soft tissues);
- weakness in the legs;
- paralysis - inability to move;
- reduction in the volume of the legs;
- decrease in their tone.
The patient constantly complains that his feet are cold.
Pain is one of the typical symptoms. Their characteristics are as follows:
- by location - on the back surface of the legs;
- by nature - aching, twisting;
- by severity - depending on the duration and severity of the lesion. The pain becomes more intense, the back of the leg is squeezed;
- by occurrence - first episodic, then constant, intensifying over time.
Violations are also recorded during an objective examination - using physical, instrumental and laboratory methods.
Physical examination consists of inspection and palpation (palpation).
Upon examination the following is revealed:
- swelling of the lower extremities;
- pallor or bluishness of the skin;
- dark areas on the skin are the result of the accumulation of melanin pigment.
On palpation:
- detect increased sweating (usually in the feet);
- confirm the presence of edema;
- identify soreness of the calf muscles (they are located on the back of the lower leg).
An objective examination also reveals a violation of tendon reflexes.
Instrumental methods are used to carry out differential diagnosis with other diseases whose clinical picture is similar to the disease being described. Conducted:
- ultrasound examination of the vessels of the lower extremities;
- angiography;
- CT angiography (computed tomography combined with angiography)
and others.
Laboratory methods are less informative in identifying and assessing alcoholic polyneuropathy, but they can complement the overall diagnostic picture. At the same time, they do a general blood test, a blood sugar test, and others.
Diabetic polyneuropathy - symptoms and treatment
Among all forms of diabetic polyneuropathy, the most common is chronic distal sensorimotor polyneuropathy (damage to sensory and motor nerve fibers of the upper and/or lower extremities). Its development depends on the type of diabetes mellitus: in the case of insulin-dependent diabetes mellitus type 1, symptoms may develop several years after the onset of the disease, while in non-insulin-dependent diabetes mellitus type 2, clinical signs of polyneuropathy may be the first manifestation of diabetes mellitus [5].
In the early stages of development of DPN, patients may complain of a feeling of numbness, tingling, “crawling” (paresthesia), burning, shooting, cutting pain in the legs, which intensifies in the afternoon and often causes sleep disturbances.
In later stages of the disease, thin nerve fibers are involved in the pathological process, which is manifested by the occurrence of hyperalgesia or allodynia. Hyperalgesia is characterized by increased sensitivity to pain from stimuli that in a healthy person cause a slight pain reaction (for example, a prick with a blunt needle). Allodynia is the appearance of pain in response to irritation that is not normally accompanied by it (the touch of a blanket, a piece of cotton wool, a brush).
The distribution of clinical symptoms is relatively symmetrical, typically starting from the toes in a “toe” pattern and moving from bottom to top. Involvement of the upper extremities is noted in later stages. Impaired sensitivity of the hands spreads according to the same pattern as in the lower extremities: from bottom to top, taking on the appearance of “gloves.” Along with sensory disturbances, upon examination one can detect a decrease or loss of tendon reflexes, first distal (Achilles) when checking the reaction of the plantar flexion of the foot to a blow with a hammer, then the knee ones.
Over time, diabetic polyneuropathy progresses, movement disorders such as weakness and muscle atrophy appear. In some patients in the later stages, a characteristic symptom is paralysis of the extensor muscles of the feet, as a result of which they cannot stand on their heels, and while walking, a pathological gait is revealed - stepping (when stepping, the patient raises his leg high, throws it forward and sharply lowers it). The speed and likelihood of development of motor symptoms depends on many factors: both glycemic control and concomitant pathologies (the previously mentioned arterial hypertension, hypercholesterolemia, smoking, alcohol abuse).
If a patient experiences sharp fluctuations in glycemic levels, for example, with decompensation of diabetes mellitus or with a sharp normalization of blood glucose levels at the beginning of treatment, acute sensory polyneuropathy (manifested by a sensitivity disorder) may develop. Among the main acutely developing symptoms are the appearance of intense burning pain in the feet, sensations of “lumbago”, “knife or electric shock”, which spread to the level of the legs, less often - the thighs. Against the background of severe pain, sensory disturbances and motor symptoms are almost never detected. Decreased tendon reflexes and muscle atrophy are not typical.
Chronic diabetic polyneuropathy is characterized by an irreversible progressive course, and acute polyneuropathy is a reversible condition in which the pain syndrome is relieved over time [3][5].
The table lists the main diagnostic characteristics for comparing chronic and acute DPN [5].
| Clinical picture | Acute sensory DPN | Chronic sensory/sensorimotor DPN |
| The nature of spontaneous pain | Very strong, burning | The intensity varies, but in general the pain is less pronounced, aching, shooting, cutting |
| Provoked pain | Allodynia, hyperalgesia | Hyperalgesia often, allodynia less often |
| Decreased sensitivity | Absent or weakly expressed | Decreased or loss of vibration, tactile and temperature sensitivity |
| Motor (motor) symptoms | None | May be (unsteadiness of gait, poor balance, weakness and muscle atrophy), but not necessarily |
| Tendon reflexes | Saved | May be reduced or absent |
| Restless legs syndrome | absent | May be |
| Other symptoms | Often - severe weight loss due to insulin deficiency | Not typical |
| Start | Relatively sharp, fast | Gradual |
| Flow | Complete relief of symptoms within 12 months. Does not lead to the development of foot ulcers or osteoarthropathy | Long-term persistence or worsening of symptoms, possible development of foot ulcers or osteoarthropathy |
| Predominant defeat | Small nerve fibers | Long nerve fibers, possibly small |
Treatment
What kind of intervention does leg failure in alcoholism require? Alcoholic polyneuropathy is treated on an outpatient or inpatient basis. The main principles of treatment are:
- refusal of alcohol;
- good nutrition;
- drug therapy;
- physiotherapy.
is based on the use of drugs such as:
- vitamins;
- antidepressants;
- anticonvulsants;
- antioxidants.
If a patient experiences leg failure, it is extremely important to use B vitamins - B1 in combination with B6 or B12. They stimulate processes as a result of which nerve fibers are restored. As a result, the normal structure of neurons is restored, impulses are transmitted through them without delay, and fiber nutrition improves.
After treatment, the patient undergoes a rehabilitation course. In this case, the following are involved:
- massage;
- acupuncture;
- electrophoresis;
- magnetic therapy;
- mud therapy - it is carried out in the form of mud wraps or applications;
- contrast baths;
- hyperbaric oxygen therapy;
- physical activity. Physical therapy and swimming are effective.
According to indications, sanatorium-resort treatment is prescribed in specialized sanatoriums.
Since the nerve tissue is affected, treatment takes a long time. Its success depends on whether the patient has stopped drinking alcohol. Therefore, it is of great importance to rid him of alcohol addiction. This will require the intervention of highly qualified specialists who successfully practice in addiction medicine.
Since patients often seek help late, it is not possible to cure alcoholic neuropathy, and disability occurs.
Exercise complexes
Exercise therapy for polyneuropathy includes:
- power;
- aerobic;
- for flexibility;
- to maintain exercise balance.
At the very beginning of the lesson, it is best to start with short workouts for 2-10 minutes, gradually increasing them to 30 minutes per day.
Exercise therapy is highly effective for polyneuropathy of the upper and lower extremities.
To perform a balance exercise, take a chair and position yourself behind its back. You need to place your feet shoulder-width apart and hold onto the chair with your hands. After this, you need to alternately raise one leg to the side and stay in this position for at least 5-10 seconds. Important !
Make sure your back and knees remain straight while doing this exercise. Balance exercises should be done 2 times during the day for several minutes. Thanks to stretching for polyneuropathy, it is possible to avoid injuries that arise as a result of performing other physical exercises. Flexibility exercises help keep your joints toned and increase their flexibility. It is recommended to start performing such exercises by stretching the calf muscle.
You need to put your foot back so that your toe points forward. Step forward with your other foot and bend your knee slightly to make it comfortable, but keep the heels of both limbs on the floor. You need to stand in this position for at least 15 seconds, then change legs. It is recommended to do this exercise 2 times a day every day.
The patient’s condition can be improved using the following set of general exercise therapy exercises for polyneuropathy:
- clenching and unclenching of the hands;
- rotating exercises in different directions with fingers clenched into a fist;
- rolling from toe to heel followed by standing on your heels for several seconds.
For polyneuropathy, you can buy a special rubber ball, which should be kneaded alternately with both hands. More examples of exercises:
Literature:
- Basic polyneuropathies: Guillain-Barre syndrome, CIDP, alcoholic, diabetic and other polyneuropathies: textbook / Kodintsev A. N., Volkova L. I., Oshurkov P. A. [et al.]; Federal State Budgetary Educational Institution of Higher Education "Ural State Medical University" of the Ministry of Health of the Russian Federation, Department of Nervous Diseases, Neurosurgery and Medical Genetics, MAU City Clinical Hospital No. 40, Yekaterinburg, Medico-Pharmaceutical. — Ekaterinburg: LLC “Tip. For you", 2019. - 64 p.
- Classical neurology: a guide to the peripheral nervous system and chronic pain syndromes / Silantiev Konstantin. - Volgograd: Panorama, 2006 (Volzhsky: Alliance Yugpoligraphkombinat, Volzhsky polygraphkombinat). — 399 p.
- Private neurology: a textbook for students of medical universities / [G. O. Andreeva and others] ; edited by M. M. Same. — Moscow: Med. information agency (MIA), 2009. – 574 p.