According to WHO (World Health Organization), atherosclerosis is various changes in the inner lining of the arteries (intima). They can manifest themselves as accumulation of lipids, complex carbohydrates, fibrous tissue, blood components, calcification (deposition of calcium salts), which leads to damage to the medial layer of the vessel. In the international classification of diseases ICD-10, the pathology is coded I67 (“Other cerebrovascular diseases”).
Vascular sclerosis occurs as a result of disturbances in lipid and protein metabolism in the body and is accompanied by the deposition of cholesterol, LDL and VLDL (low and very low density lipoproteins) on the walls of blood vessels. In this way, atherosclerotic plaques are formed (they are fibrous and cholesterol), gradually reducing the lumen of the arteries. The smaller their diameter, the less blood flows to organs and tissues, and ischemia occurs. Complete blockage leads to tissue necrosis. Another scenario is possible: an atherosclerotic plaque may break off and travel further in the bloodstream, where it will clog a capillary of a smaller diameter. As a rule, either an infarction occurs in the myocardium of the heart or a stroke in the brain.
The Yusupov Hospital offers complete diagnosis and treatment of cerebrovascular sclerosis using modern equipment. An individual approach to each patient and adherence to current treatment recommendations is the key to the professionalism of our specialists.
Causes of development of vascular sclerosis
The causes of sclerosis depend on risk factors. They can be modifiable, that is, we can influence them - lifestyle and laboratory parameters, or non-modifiable - age, gender and genetic predisposition.
Non-modifiable ones include:
- gender - men suffer more often, this is explained by the fact that in women estrogen has an angioprotective function;
- age - men over 45, women > 50 or with early menopause;
- cases of atherosclerosis in relatives.
Modifiable are:
- smoking;
- drinking excessive amounts of alcohol;
- lack of plant foods in the diet;
- low physical activity;
- stress;
- overweight;
- dyslipidemia;
- diabetes;
- arterial hypertension.
Atherosclerosis of cerebral vessels most often occurs in the following places:
- brachiocephalic trunk;
- carotid artery (common and external carotid);
- cerebral arteries (anterior, posterior and middle);
- vertebral artery and other small vessels.
Expert opinion
Author: Alexey Vladimirovich Vasiliev
Neurologist, Head of the Research Center for Motor Neuron Disease/ALS, Candidate of Medical Sciences
Atherosclerosis of cerebral vessels is an insidious disease that is diagnosed in patients over 45 years of age. The initial stage proceeds almost unnoticed, so patients seek help in an advanced state. People who have relatives with atherosclerosis are susceptible to the disease, so they are recommended to undergo regular diagnostics to detect the disease at an early stage.
The disease occurs due to the accumulation of cholesterol plaques. Most often, BMS sclerosis is diagnosed in people who lead an inactive lifestyle, consume tobacco and alcohol, abuse fried foods and are overweight.
The disease develops in several stages. The initial stage is asymptomatic and very difficult to recognize. However, all stages are accompanied by various symptoms:
- Initial. Headaches and dizziness occur, which are most often attributed to overwork. It is worth considering that after sleep the symptoms disappear.
- Progressive. It is characterized by increased symptoms of the previous stage, the patient experiences emotional instability, and the person becomes depressed.
- Decompensation. It is the most complex form of the disease, in which stroke or paralysis occurs. The patient has memory loss and requires constant care.
The disease is most acutely tolerated by a person, as complications appear that end in complete loss of capacity or, even worse, death of the patient.
Causes of hippocampal sclerosis
The central question of the etiology of FH is to clarify what occurs primarily: structural pathology of the hippocampus, which triggers chronic drug-resistant epilepsy, or, conversely, long-term pathological electrical activity leads to sclerosis over time. It is important to note that a significant proportion of patients with risk-related epilepsy associated with HS experience febrile seizures or other acute pathology of the central nervous system (trauma, anoxia, neuroinfection) in early childhood, which is referred to as initial precipitating damage. The acquired nature of HS is supported by those rare observations when this pathology occurs in one of the monozygotic twins, the second twin does not have sclerosis, and, therefore, the genetic factor is not paramount. However, hereditary familial forms of temporal lobe epilepsy (for example, a group of epilepsies associated with mutations in the SCN1a and SCN1b genes encoding sodium) indicate that a genetic factor also plays a role, causing hippocampal sclerosis in some of these patients without a history of febrile seizures . Speaking about the acquired nature of the disease, it should also be taken into account that not every type of seizure is associated with the development of FH: autopsy data indicate that long-term uncontrolled epilepsy with frequent generalized seizures does not lead to neuronal loss in the hippocampus, as does afebrile status epilepticus. On the other hand, febrile status epilepticus is accompanied by MRI evidence of hippocampal edema. The answer to the question of how often the status of febrile seizures in a child is realized in FH and drug-resistant epilepsy may be provided by the prospective study FEBSTAT. It has already been established that out of 226 children after febrile seizure status, 22 had MRI signs of hippocampal edema, most pronounced in the Sommer sector (CA1). Of these 22 patients, repeat MRI at various times was performed in 14; in 10 cases, signs of hippocampal sclerosis were detected. However, out of 226 children, epilepsy was diagnosed in only 16 patients and in most cases it was non-temporal epilepsy. That is, on the one hand, febrile status does not always lead to epilepsy with hippocampal sclerosis, on the other hand, the time interval between precipitating brain injury and the appearance of temporal lobe epilepsy can be more than 10 years, and the study does not yet have a follow-up of such a duration. Genetic studies also indicate that the etiology of FH is heterogeneous. Genome-wide association studies have shown that febrile seizures with hippocampal sclerosis may be a genetic syndrome, as they are associated with the presence of a specific allele of a single nucleotide sequence located near the sodium channel gene SCN1A. This association was not found for cases of epilepsy with FH without febrile seizures. The consensus opinion of epileptologists is that there is a certain initial genetic predisposition, which is realized in hippocampal sclerosis in the presence of a certain damaging factor (double hit hypothesis).
Symptoms and signs of cerebral sclerosis
Symptoms and signs depend on the degree of mismatch between the brain's oxygen needs and the body's capabilities, as well as on the duration of this pathological condition. Brain tissue consumes up to 25% of all oxygen entering the body and up to 70% of glucose, since the brain does not have glycogen reserves from which other tissues take it. There is an assumption that if you hold your breath for 10 seconds, the brain is able to use all the oxygen that is currently in its tissues. And with sclerosis of its vessels, oxygen deficiency gradually increases, leading to the appearance of the first symptoms that need to be paid special attention to:
- having trouble sleeping, waking up more tired;
- headaches become more frequent or appear for the first time. Most often as a migraine;
- memory deteriorates, you become absent-minded, it is difficult to concentrate on a task;
- constant lethargy and depressed mood.
Rehabilitation for multiple sclerosis
- Physiotherapy.
Exercise therapy helps improve a person’s condition with impaired motor activity. Working out on exercise machines helps restore coordination of movements. With correctly selected loads, the method demonstrated excellent efficiency. - Physiotherapy.
For patients with MS, electrophoresis, myostimulation, ultrasound, and magnetic therapy are recommended. These techniques help to activate the body's metabolic processes and reduce inflammation. - Massage.
For multiple sclerosis, this rehabilitation method can be used to relieve pain symptoms and spasms. Massage also helps improve muscle tone when it decreases.
Rehabilitation for multiple sclerosis also includes psychotherapy, which will help the patient cope with negative thoughts, as well as consultations with a nutritionist.
Disease prognosis
Multiple sclerosis is not considered a fatal disease; the unpleasant symptoms of MS can be quite successfully treated. Scientists have found that thanks to modern treatment, the life expectancy of patients today has increased significantly compared to those who fell ill even a few decades ago.
Overall, people with multiple sclerosis live on average 7 years less than the general population. Often, a decrease in life expectancy is associated with complications of other pathologies: cancer and cardiovascular diseases. For many patients, quality treatment can prevent a decline in quality of life and productivity. According to the National Multiple Sclerosis Society, ⅔ of people with MS are wheelchair-free even 20 years after diagnosis.
Disability in multiple sclerosis
| If multiple sclerosis has caused disability for 5 months or more within a year, the patient can apply for disability registration. |
After reviewing the documents, the commission will make a decision on incapacity for work, which gives the right to receive a pension and preferential working conditions. The establishment of a disability group is influenced by:
- the period for which the ability to work was lost;
- the period when the patient was registered with this disease;
- frequency, duration and severity of exacerbations;
- therapy results;
- changes in the course of the disease, the rate of development of symptoms.
Disability is assigned for a year, after which it is necessary to pass the commission again. Disability of groups I and II with MS gives the right to a reduced working day - 35 hours per week. In this case, wages are paid in full.
Initial stage of the disease
At the initial stage, all previous “bells” become more pronounced and intensified. In addition to the above, dizziness, ringing in the ears and flickering of “spots” before the eyes occur, and a feeling of heaviness in the head appears.
At this stage, about 90% of patients complain of migraine headaches. They differ from ordinary ones in that they can appear at any time of the day. Their occurrence is provoked by physical or mental work, stress, and being in a stuffy room. In addition to the characteristic pulsating or pressing pain sensations, fear of light and noise is added. Conventional painkillers do not relieve the condition.
Treatment of multiple sclerosis in young people
Treatment is divided into 3 categories:
- therapy for exacerbations;
- slowing progression using modification methods;
- symptomatic therapy.
Treatments are becoming increasingly complex as additional subtypes of the disease are being explored. This reduces the frequency and severity of exacerbations, as well as the accumulation of lesions detected by magnetic resonance imaging.
Initiating treatment to slow inflammatory lesions in the early stages is considered a way to prevent the development of disability. There is not yet enough comparative effectiveness data to guide health care providers in making optimal treatment choices.
Yusupov Hospital is one of the best centers for the treatment of multiple sclerosis in Moscow. Contact us for a consultation!
Second stage
It is characterized by a combination of complaints similar to the initial stage, but the condition is aggravated by the appearance of neurological microsymptoms:
- reflexes of oral automatism come to life;
- the innervation of facial muscles is disrupted, the tongue deviates in the direction of damage;
- coordination and oculomotor disorders occur;
- the speed of reflexes decreases, there may be convulsions or even paralysis (complete/partial);
- active movements slow down, muscle tone increases;
- Memory lapses increase, negative character traits become sharper, and psychosis is possible.
Diagnosis of cerebral vascular sclerosis
The Yusupov Hospital has all the necessary equipment to carry out a full range of diagnostics. Experienced neurologists pay close attention to each patient, listen to their complaints and collect anamnesis in order to make the correct diagnosis. To clarify this disease, it is necessary to find out the presence of associated factors:
- bad habits - smoking, drinking alcohol and other drugs;
- relatives with the same disease;
- diabetes mellitus, myocardial infarction;
- cerebrovascular accidents, damage to the great vessels of the head;
- transient ischemic attacks in the past.
Laboratory examination methods use a blood test to identify the following indicators:
- dyslipidemia;
- hyperglycemia;
- hypercoagulation;
- increase in atherogenicity coefficient.
During physical examination, a reliable method for determining carotid artery sclerosis is auscultation in the bifurcation area (where the common carotid artery divides into two large branches - the internal and external carotid arteries). If stenosis is present, a systolic murmur will be heard using a phonendoscope.
The most informative instrumental studies include:
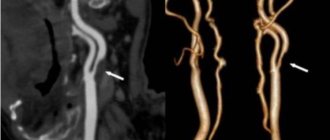
- Doppler ultrasound (duplex scanning) of the vessels of the head. The bottom line is that with the help of ultrasound you can find out the speed of blood flow using the Doppler effect. It is performed in two modes - two-dimensional (B-mode) and transcranial duplex scanning. Their difference is that B-mode allows you to study blood flow in vessels that are not located inside the skull. Transcranial scanning is used additionally when examining brain tissue for the presence of tumors;
- angiography - visualization of blood vessels by introducing a special contrast agent into the bloodstream, which will be visible on x-rays;
- MRI and CT examination. They make it possible to identify cerebral circulatory disorders (ischemia, strokes), vascular malformations (aneurysms, dissections), as well as neoplasms. MRI is preferable because there is no radiation exposure and the method is non-invasive. But with the help of CT, you can detect minimal changes and obtain a three-dimensional image of internal organs, arteries and veins, joints and bones.
Histological structure of the sclerosed hippocampus
Macroscopically, the sclerotic hippocampus is reduced in volume and dense, and among the main microscopic characteristics are a decrease in the number of pyramidal cells in various SA layers and a variable degree of gliosis. In the granular layer of the dentate gyrus, varying degrees of reduction in neuronal density may be observed, although in general its structure is more preserved compared to the SA layers. Also a distinctive histological feature is that the loss of neurons does not extend beyond the SA layers to the subiculum, which distinguishes hippocampal sclerosis from its atrophy during ischemic damage and neurodegenerative diseases. It was noted that loss of neurons in the pyramidal layer of the hippocampus can occur in several ways, which was the basis for the formation of the classification of this pathology. The most widely used classification of hippocampal sclerosis was created by the ILAE commission. In type 1 HS (severe or classic), neuronal loss is observed in all layers of the hippocampus; type 2 is characterized by loss of neurons predominantly in the CA1 layer; and in type 3 HS, only the CA4 layer is affected in the area of the transition to the dentate gyrus (so-called end folium sclerosis). In the literature, along with the term hippocampal sclerosis, a number of definitions often appear that emphasize that histological signs of the disturbed structure of brain tissue can extend beyond the hippocampus.
Thus, the term “mesial temporal sclerosis” takes into account the fact that, along with the hippocampus, atrophic and gliotic changes are observed in the amygdala and habenula. When analyzing the histological material obtained during surgery for temporal lobe epilepsy, it became obvious that sclerosis of the hippocampus is accompanied by pathohistological changes in the lateral neocortex of the temporal lobe. Thom proposed the term “temporal sclerosis”, which defines neuronal loss and gliosis in layers 2-3 of the temporal cortex. Quite often, heterotopic neurons are detected in the neocortex in the 1st layer of the cortex and white matter, which is referred to as “microdysgenesis.” In 2011, the ILAE Commission presented a new classification of focal cortical dysplasias, where a group of FCD type 3a was identified, when hippocampal sclerosis can be combined with dysplasia of the temporal lobe cortex in the form of a violation of its laminar structure, which in turn is classified as FCD type 1. Microdysgenesis, the role of which in epileptogenesis is not yet known, are classified as so-called small malformations of the cerebral cortex and, when identified with hippocampal sclerosis, the diagnosis is defined as FCD type 3a. Just like FCD 3a, a combination of temporal sclerosis and hippocampal sclerosis is considered. The concept of “dual pathology” is often encountered in the literature, when hippocampal sclerosis is combined with a potentially epileptogenic lesion of the neocortex, including outside the temporal lobe, for example, a tumor, vascular malformation, FCD type 2, Rassmussen’s encephalitis, gliotic scar. At the same time, the concept of “double pathology” does not include FCD type 3a. The terminology becomes even more complex, since the presence of two epileptogenic brain lesions, but without hippocampal sclerosis, is designated as double pathology.
To understand the connections between different parts of the hippocampus and the pathogenesis of HS, it is necessary to have an idea of the structure of the polysynaptic intrahippocampal pathway, which starts from the neurons of layer 2 of the entorhinal cortex (located in the anterior part of the parahippocampal gyrus and in the area of the uncus). The processes of these neurons form a perforant path, which goes through the subiculum of the parahippocampal gyrus into the dentate gyrus and contacts the dendrites of the cells of the granular layer. Neurons of the granular layer form mossy fibers that innervate CA3 and CA4 pyramidal neurons, which in turn contact the CA1 layer through lateral axons, the so-called Schaffer collaterals. Abnormal growth of mossy fibers instead of the SA layers into the dentate gyrus with the formation of excitatory synapses is considered one of the pathogenetic links in HS. From the above SA layers, axons enter the alveus and then into the fornix through the hippocampal fimbria. Taking into account the anatomical and functional connection between Ammon's horn, dentate gyrus, and subiculum, a number of authors have designated them the term “hippocampal formation.”
Treatment of cerebral vascular sclerosis
Treatment tactics are aimed at eliminating vessel occlusion (if possible), stimulating the development of collateral circulation and preventing the progression of sclerosis with possible complications.
Treatment begins with adjusting the patient’s lifestyle - quitting smoking and drinking alcohol, increasing physical activity, correcting nutrition and monitoring blood pressure, blood sugar and cholesterol levels. Additional, but no less important, treatment methods include physiotherapy: balneotherapy, massage and other procedures prescribed by a doctor.
Physical activity should be appropriate for age and level of physical fitness, be regular and strictly dosed. It increases the supply of oxygen and blood circulation throughout the body. Physical exercise will help reduce cholesterol levels and weight if it is overweight.
Subchondral sclerosis
Subchondral sclerosis is a disease that affects the joints. As the disease progresses, articular cartilage degenerates, resulting in changes in the articular surface. The incidence of the disease increases markedly with age. Subchondral sclerosis is divided into primary and secondary forms. In the first case, the cause of the disease is severe overload of the spine, while the disease develops in healthy cartilage. In the second case, the disease develops on previously injured cartilage, which has been negatively affected due to injury, arthritis or the influence of other disorders.
Subchondral sclerosis of the endplates of the vertebral bodies often occurs when a person develops osteochondrosis or spondylitis . It is important to conduct a competent diagnosis and prescribe timely treatment for the disease. Various methods of therapy are practiced, but if the disease is too advanced, the doctor may decide on surgical intervention.
Drug therapy
The following groups of drugs are prescribed. Our specialists at the Yusupov Hospital will select the most suitable combination based on your medical history and examination.
- statins;
- antiplatelet agents;
- nootropics to improve cerebral circulation;
- antihypertensive drugs and drugs that lower blood sugar (if there is a concomitant pathology).
Statins are drugs that reduce certain fractions of lipids (in particular low- and very low-density lipoproteins), which are deposited on the walls of blood vessels. Antiplatelet agents increase blood clotting to prevent the accumulation of red blood cells on the atherosclerotic plaque. Thus, these two groups of drugs protect against recurrent sclerosis and the risk of stroke.
Nootropic drugs, in turn, have a stimulating effect on the integrative function of the brain. By regulating energy processes in cells, they fight hypoxia and also improve blood supply to the central nervous system. Taking nootropics improves the trophism of nervous tissue, which leads to increased brain activity, activation of operational and long-term memory and restoration of hemodynamics after a stroke or brain injury.
Antihypertensive therapy aims to lower blood pressure below 140/90 to prevent complications.
Pathogenesis of hippocampal sclerosis
Hippocamal sclerosis has two fundamental pathological characteristics: the first is a sharp decrease in the number of neurons and the second is hyperexcitability of the remaining nervous tissue. One of the key roles in epileptogenesis in HS is played by the sprouting of mossy fibers: abnormal axons of granular cells, instead of innervating the SA cells of the hippocampus, reinnervate the molecular neurons of the dentate gyrus through excitatory synapses, thus creating local electrical circuits capable of synchronizing and generating an epileptic seizure. An increase in the number of astrocytes, gliosis may also play a role in epileptogenesis, because altered astrocytes cannot sufficiently reuptake glutamate and potassium. Proinflammatory cytokines, such as IL-1β, IL 1, TNFa, can also act through the mechanism of increasing glutamate release and decreasing reuptake, GABA inhibition. In this regard, the role of herpes virus type 6, the DNA of which is found in the brain tissue of patients with temporal lobe epilepsy, is discussed in the pathogenesis of FH.
Diet for cerebral sclerosis
Diet No. 10C is prescribed, which consists of reducing the intake of animal fat, easily digestible carbohydrates and cholesterol, as well as salt to 5–7 grams per day. It is recommended to eat plant foods and seafood. The diet should include ingredients that contain B vitamins and vitamin C, dietary fiber, potassium, magnesium (vegetable oils, vegetables and fruits, seafood, cottage cheese). Ready meals should be fresh. Boiled food is preferred, sometimes baking is allowed. The food temperature is normal. Approximate composition of KBZHU: 2200-2600 kcal, proteins - 90-100 g (50% animal), fats - 70-80 g (40% vegetable), carbohydrates - 300-350 g (50 g sugar). Low numbers are recommended for comorbid obesity. Consume up to 1.2 liters of water per day, table salt - up to 7 g.
It is prohibited to consume any types of fatty, salty and spicy foods: fatty meats, fish, poultry, canned food, sausage, caviar, smoked and salted fish, butter and puff pastry, fatty dairy products, rice, semolina, pasta, various salty and spicy foods. snacks and sauces.
A sample menu for one day would look like this:
First breakfast: low-fat cottage cheese with a small handful of nuts and dried apricots, a protein omelet, weak tea.
Second breakfast: fresh apple.
Lunch: fresh cabbage soup, steamed meat balls (chicken), vegetable sauté, compote.
Snack: rose hip decoction, apple or pear.
Dinner: tomato and seaweed salad, baked fish and boiled potatoes, tea with lemon.
At night: a glass of 1% kefir.
Amyotrophic lateral sclerosis
Amyotrophic lateral sclerosis is also called motor neuron disease. This is a disease of the nervous system that has a progressive chronic nature, during which central and peripheral motor neurons are selectively affected. In this condition, a person experiences increasing weakness of the shoulder and pelvic girdle, bulbar muscles, trunk and abdominal muscles, while the extraocular muscles and sphincters of the pelvic organs are affected to a lesser extent. Treatment of the disease is carried out continuously, in courses.
As a rule, the disease occurs sporadically; familial cases occur rarely. A person can get sick at any age, but more often the disease develops in people after 50 years of age.
It is believed that the disease is caused by a virus. The disease develops slowly, sometimes a person does not notice its onset. First of all, weakness of the distal parts of the arms gradually develops, and difficulty speaking may occur. Later, the specialist discovers the presence of atrophy and paresis of the small muscles of the distal segments of the arms. Gradually, there is a progression of paresis and atrophy, which can spread to the muscles of other parts of the body. In addition to these signs, the patient has symptoms that indicate damage to the pyramidal system.
Over time, the patient develops problems with swallowing, articulation, and phonation. They gradually become more pronounced. The tongue has limited movement and atrophy. The patient does not have a pharyngeal reflex; constant salivation occurs due to the inability to swallow saliva.
If there is weakness in the neck muscles, the patient's head may droop and movement is limited. Over time, facial and chewing muscles weaken. A person has a lower jaw and it becomes difficult for him to chew. Involuntary laughter and crying are also possible.
Doctors distinguish three types of amyotrophic lateral sclerosis: bulbar , cervicothoracic , lumbosacral . The disease is always progressive.
Diagnosis of the disease includes determining the presence of characteristic symptoms. The patient also undergoes electromyography, the data of which can confirm damage to the cells of the anterior horns of the spinal cord. To clarify the diagnosis, MRI of the cervical spine and myelography are performed.
Existing methods of therapy to this day do not completely cure the disease. Patients should be regularly monitored by several doctors of different specialties. Patients are prescribed to take riluzone , vitamin E , and B vitamins . Treatment with nootropic drugs , ATP , and anabolic hormones . To improve neuromuscular conduction, treatment with dibazole , prozerin , and oxazil . The use of other drugs and light massage sessions of the limbs is also practiced.
The disease can last from two to ten years, and the prognosis is unfavorable. The patient dies from paralysis of the respiratory center, exhaustion, and intercurrent infections. If a person also has bulbar disorders, he can live no more than two years.
Surgical intervention
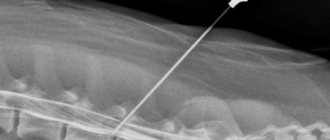
Surgical treatment of carotid artery stenosis is recommended for patients with stenosis greater than 60% (NASCET). For this pathology, two types of surgical interventions are possible: carotid endarterectomy and carotid angioplasty. Surgical treatment is determined by the attending physician based on medical history, examination data and possible risks.
Carotid endarterectomy (CEA) is an open surgical procedure aimed at removing the inner wall of the carotid artery affected by atherosclerotic plaque. Technique of the operation: under anesthesia, an incision is made in the neck in the projection of the carotid artery. It is released and opened at the site of narrowing. A temporary shunt is placed to ensure blood flow to the brain. Then the inner part of the vessel wall with the atherosclerotic plaque is removed. Afterwards, plastic surgery of the artery is performed and the wound is sutured layer by layer.
Carotid angioplasty with stenting (CAS) is a minimally invasive X-ray surgery that involves installing a stent at the site of the narrowing. A stent is a tube made of a special metal mesh. The first stages of stenting are the same as for angiography: preparation, local anesthesia, puncture of the artery, insertion of a catheter and injection of a contrast agent. After installing a guiding catheter, a special metal filter is inserted into the affected carotid artery. Its essence is to delay possible microemboli that can break away from the plaque and enter the brain vessels. Then a stent is inserted along the guide, it is inflated by a balloon catheter, and it restores the normal diameter of the artery, serving as its frame. Thanks to this, proper blood supply to the brain is restored. The entire manipulation is carried out under X-ray control - everything is visible on the monitor. At the end of the operation, the filter and catheter are removed, leaving a stent inside. Over time, it epithelializes and becomes one with the wall.
After surgery, it is recommended to avoid intense exercise for six weeks. You should stop driving for three weeks.
Prevention of cerebral vascular sclerosis
Prevention consists of leading a healthy lifestyle, namely giving up bad habits, maintaining a work-rest schedule and a balanced diet. If you have diseases that can lead to sclerosis (diabetes mellitus, arterial hypertension), you should follow the instructions of your doctor.
All patients who have undergone surgery for carotid artery stenosis should be periodically observed by a neurologist and a vascular surgeon, and at least once a year undergo an outpatient examination with mandatory Doppler ultrasound of the vessels of the neck and head.
You can undergo examination and treatment for cerebral vascular sclerosis in Moscow at the Yusupov Hospital. The clinic’s doctors use the latest equipment to detect the disease at the initial stages. An individual approach to each patient consists of developing a personal treatment plan. Therapy is carried out in accordance with the latest European recommendations for the treatment of atherosclerosis. You can sign up for a consultation and ask all your questions by phone.
Diagnostics
Diagnosing multiple sclerosis is not easy, as its symptoms are common to many other diseases. There is currently no diagnostic method for accurately determining multiple sclerosis. Therefore, if there is a suspicion of this disease, a complex of research methods is used. First of all, the doctor studies the medical history and conducts a neurological examination. The patient is prescribed an MRI and lumbar puncture. To exclude other diseases, a laboratory blood test is practiced.