Benedict's syndrome (syn. alternating paralysis syndrome)
The syndrome occurs as a result of a pathological process in the medial-dorsal part of the midbrain at the level of the red nucleus and the cerebellar-rednuclear tract with the preservation of the paramidal fasciculus. The causes of the lesion are thrombosis and hemorrhages in the posterior cerebral artery basin, tumor metastasis.
Clinical signs and symptoms. On the affected side, extrapyramidal hyperkinesis in the limbs and cerebellar ataxia occur. On the side opposite to the localization of the lesion, mild spastic hemiparesis and tremor of the lower extremities develop. Against the background of hemiparesis, increased tendon reflexes are observed.
In addition, there is an increase in overall muscle tone. Eye symptoms are caused by complete or partial paralysis of the oculomotor nerve. Ptosis occurs on the side of the pathological focus. There is a deviation of the eyeball towards the lesion, there may be disturbances in associated eye movements during convergence and the direction of gaze up or down. A differential diagnosis of this syndrome is made with the following syndromes: Claude, Weber-Gubler-Gendrin, Millard-Gubler, Fauville, Nothnagel.
The development of the syndrome is associated with a pathological process located directly in the region of the cerebral peduncles, which occurs as a result of hemorrhages, ischemic cerebral circulation disorders, as well as neoplasms. In addition, the signs of this syndrome may be caused by dislocation compression of the cerebral peduncles by a tumor located at a distance.
Clinical signs and symptoms. Due to damage to the facial and lingual nerves, as well as the pyramidal tract, paralysis of the muscles of the face, tongue and limbs of the central type occurs on the side opposite the pathological focus. Eye symptoms are caused by complete (ophthalmoplegia, ptosis, mydriasis) or partial (damage to only intraocular muscles or individual extraocular muscles ) oculomotor nerve palsy.
Symptoms of paralysis occur on the side of the pathological focus. In case of damage to the extraocular muscles innervated by the oculomotor nerve, the eyeball deviates towards the temple and “looks” towards the pathological focus, “turning away” from the paralyzed limbs. If a pathological process - for example, an aneurysm of the anterior cerebral artery - involves the optic tract or the external geniculate body, homonymous hemianopsia occurs.
Unilateral damage to the ventral part of the pons involving the nucleus or bundle of fibers of the facial nerve, the root of the abducens nerve and the underlying pyramidal tracts leads to the development of this syndrome. The pathological process in this area may be associated with impaired circulation in the paramedian arteries (hemorrhages, thrombosis).
With the development of a tumor of the pons (most often glioma and much less often cancer metastasis, sarcoma, solitary tubercles), a slow gradual development of the syndrome is observed. Clinical signs and symptoms. On the affected side, signs of peripheral paralysis of the facial nerve appear, while central hemiparesis or hemiplegia is observed on the side opposite the lesion.
{module direct4}
Ocular symptoms are caused by damage to the abducens and facial nerves. On the side opposite the pathological focus, signs of damage to the abducens nerve appear - paralysis of the external rectus muscle, convergent paralytic strabismus, diplopia, which intensifies when looking towards the affected muscle. On the contrary, symptoms of damage to the facial nerve are observed on the side of the pathological focus - lagophthalmos, lacrimation.
The pathological process in this syndrome is located at the base of the legs and involves the fibers of the oculomotor nerve. The development of the syndrome is caused by damage to the branches of the posterior cerebral artery - the middle and posterior arteries of the red nucleus, which supply blood to the lower parts of the red nucleus. The most common causes of vascular damage are atherosclerosis and syphilitic endarteritis.
Etiology and pathogenesis
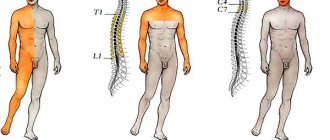
Alternating syndromes occur with damage to one half of the brain stem, spinal cord (Brown-Séquard syndrome), as well as with unilateral combined damage to the structures of the brain and sensory organs. Various alternating syndromes can be caused by circulatory disorders in the spinal cord and brain stem, tumor processes localized in the brain stem, and traumatic brain injuries. Stem symptom complexes, which occur most often, are characterized by damage on the side of the lesion to one or more cranial nerves of the peripheral type (due to damage to their nuclei or roots), as well as conduction disorders on the opposite side (hemiparesis, hemiplegia, hemianesthesia, hemiataxia, etc.) due to damage fibers of the pyramidal tract, medial lemniscus, cerebellar connections, etc.
There are bulbar, pontine, peduncular and mixed alternating syndromes depending on the location of the lesion (which is important for clarifying the location of the damage).
Diagnostics and therapy
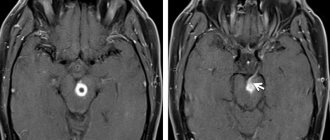
As a rule, the diagnosis of such a disease is made based on the patient’s medical history and external manifestations. In the case of Zakharchenko syndrome, the result is obvious. In addition to examining and interviewing the patient, the doctor must conduct a number of clinical and instrumental tests to exclude other diseases with similar symptoms, including the following:
- MRI of the brain;
- Doppleroscopy of the cervical spine;
- CT head;
- clinical blood test;
- a series of neurological tests.
Confirming the presence of Jacksonian epilepsy in a patient is extremely difficult, since its clinical picture is similar to other disorders. For example, with the myoclonic form of the disease and hysterical seizures. Therefore, during the diagnosis, the neurologist first examines the patient’s medical history, listens to his complaints, and only then sends him for a full examination of the body.
The patient, in addition to standard tests, needs to undergo electroencephalography. Using this diagnostic method, discharges of epileptic activity are detected. Additionally, MRI of the brain is prescribed to differentiate Jacksonian epilepsy from other pathologies (tumors, abscess, encephalitis).
If you suspect Jacksonian epilepsy, a person should consult a neurologist. He will listen to the patient's complaints and then refer him for examinations. People are required to undergo echoencephalography, MRI and CT scans, as well as blood tests. Based on the results of the research, it will be approximately clear what exactly we are dealing with.
For a complete cure, it is recommended to perform neurosurgical intervention, the purpose of which is to remove the pathological focus. If the restoration of nerve tissue is successful, then the symptoms will gradually subside. In this case, you will have to carry out maintenance therapy in order to achieve recovery faster.
If characteristic symptoms appear, a person must immediately consult a doctor and undergo an examination. Even with the help of medications, you can significantly improve your well-being. With the correct selection of medications, the manifestations of the disease will not only not intensify, but will also be significantly weakened.
Diagnostics
The diagnostic value of alternating syndromes lies in the ability to localize the lesion and determine its boundaries. For example, Jackson syndrome occurs with thrombosis of the anterior spinal artery or its branches, Avellis and Schmidt syndromes develop with circulatory disorders in the branches of the artery supplying the medulla oblongata, and Wallenberg-Zakharchenko and Babinsky-Nageotte syndromes - in the basin of the inferior posterior cerebellar or vertebral artery. Pontine syndromes of Foville, Brissot, Raymond-Sestan occur with damage to the branches of the basilar artery, peduncular syndromes - the deep branches of the posterior cerebral artery, Claude syndrome - the anterior and posterior arterioles of the red nucleus, Benedict syndrome - interpeduncular or central arteries, etc.
A change in symptoms characterizes the cause of the pathological process. Ischemic damage to the brainstem, for example, as a result of thrombosis of the vertebral branches, basilar or posterior cerebral artery, leads to the gradual development of alternating syndromes, not even accompanied by loss of consciousness. In this case, the boundaries of the lesion correspond to the zone of impaired blood supply; hemiplegia or hemiparesis is spastic in nature. Hemorrhages in the brain stem can lead to atypical alternating syndromes. This occurs due to the fact that, in addition to the area of the damaged vascular basin, the surrounding brain tissue is also involved in the process due to the development of peripheral edema. Acute development of a lesion in the pontine zone is accompanied by breathing disorders, cardiac activity, and vomiting. In the acute period, a decrease in muscle tone on the side of hemiplegia is determined.
Nothnagel syndrome (syn. quadrigeminal syndrome)
The syndrome occurs with extensive lesions of the midbrain involving the roof, tegmentum and partly the base of the brain - the quadrigeminal plate is affected; red nuclei or superior cerebellar peduncles, nuclei of the oculomotor nerves, medial geniculate bodies, central gray matter in the circumference of the aqueduct of Sylvius.
The main cause of the pathological process is pituitary tumors. Clinical signs and symptoms. At the onset of the disease, signs of cerebellar damage appear: ataxia, intention tremor, choreiform or athetoid hyperkinesis; There is a decrease in hearing on both sides or only on the side opposite to the localization of the lesion.
https://www.youtube.com/watch?v=ytoSdJfFgpg
In some cases, spastic paresis of the limbs develops. Due to bilateral pyramidal lesions, central paresis of the facial and hypoglossal nerves occurs. Eye symptoms are caused by damage to the oculomotor nerves. Bilateral ophthalmoplegia, mydriasis, and ptosis are observed. In the case of a unilateral lesion, the symptoms are more pronounced on the side opposite the lesion.
Clinical picture
Bulbar alternating syndromes
Jackson syndrome
(medial medullary syndrome, Dejerine syndrome) is observed with half the lesion of the lower part of the medulla oblongata, and is characterized by a combination of peripheral paralysis of the hypoglossal nerve and central hemiparesis of the limbs on the opposite side. Peripheral paralysis of the hypoglossal nerve: atrophy of the homonymous half of the tongue (thinning and folding of the mucous membrane), fascicular twitching. The tongue, when protruded, deviates towards the lesion of the nucleus or nerve. Standard: when the left genioglossus muscle contracts, the tongue is pushed forward and to the right, when the right muscle contracts, vice versa. If the right nerve is affected, then when the left genioglossus muscle contracts, the tongue is pushed to the right (to the affected side).
Avellis syndrome
(palatopharyngeal paralysis) develops when the nuclei of the glossopharyngeal, vagus and hypoglossal nerves and the pyramidal tract are damaged. It is characterized from the source by paralysis of the soft palate and pharynx.
Schmidt syndrome
characterized by combined damage to the motor nuclei or fibers of the glossopharyngeal, vagus, accessory nerves and pyramidal tract. It manifests itself from the side of the lesion as paralysis of the soft palate, pharynx, vocal cord, half of the tongue, sternocleidomastoid and upper trapezius muscles.
Wallenberg-Zakharchenko syndrome
(dorsolateral medullary syndrome) occurs when the motor nuclei of the vagus, trigeminal and glossopharyngeal nerves, sympathetic fibers, inferior cerebellar peduncle, spinothalamic tract, and sometimes the pyramidal tract are damaged. On the side of the lesion, paralysis of the soft palate, pharynx, vocal cord, Horner's syndrome, cerebellar ataxia, nystagmus, loss of pain and temperature sensitivity of half the face are noted; on the opposite side - loss of pain and temperature sensitivity on the torso and limbs, the emergence of perverted temperature sensitivity. Occurs when the posterior inferior cerebellar artery is damaged.
Babinski-Nageotte syndrome
occurs with a combination of damage to the inferior cerebellar peduncle, olivocerebellar tract, sympathetic fibers, pyramidal, spinothalamic tracts and medial lemniscus. Characterized from the side of the lesion by the development of cerebellar disorders, Horner's syndrome.
Pontine alternating syndromes
Millard-Gubler syndrome
(medial pontine syndrome) occurs when the nucleus or fibers of the 7th pair and the pyramidal tract are damaged. On the side of the lesion - peripheral paralysis of the facial muscles: the face is asymmetrical, the muscles of the healthy half pull the skin of the face to their side, the racket symptom, the absence of nasolabial and frontal folds, weakness of the facial muscles of the upper and lower floors (atrophy, hypotrophy, hypotonia, hyporeflexia, fibrillation and fasciculations ). Lagophthalmos (incomplete closure of the palpebral fissure due to paralysis of the orbicularis oculi muscle); eyelash symptom (when you try to close your eyes, your eyelashes remain visible); Bell's phenomenon - when you try to close your eyes, the eyeballs run upward. There are no autonomic disorders (normal taste, lacrimation, salivation and swallowing reflex are normal. Dysakusia. On the opposite side - central hemiparesis or hemiplegia.
Fauville syndrome
(lateral pontine syndrome) is observed with combined damage to the nuclei (roots) of the abducens and facial nerves, the medial lemniscus, and the pyramidal tract. It is characterized from the side of the lesion by abducens nerve palsy and gaze paralysis towards the lesion, sometimes by facial nerve paralysis. On the opposite side there is central hemiparesis or hemiplegia.
Raymond-Sestan syndrome
noted when the posterior longitudinal fasciculus, middle cerebellar peduncle, medial lemniscus, or pyramidal tract are affected. Characterized by paralysis of gaze towards the hearth.
Brissot's syndrome
occurs when the nucleus of the facial nerve is irritated and the pyramidal tract is damaged. Characterized by facial hemispasm on the side of the lesion.
Gasperini syndrome
occurs when the tegmentum of the pons is damaged and is characterized by a combination of damage to the auditory, facial, abducens and trigeminal nerves on the side of the pathological focus.
Peduncular alternating syndromes
Weber syndrome
(ventral mesencephalic syndrome) there is damage to the nuclei and roots of the third pair of the cranial nerve (oculomotor nerve) and the pyramidal tract. On the affected side: ptosis, mydriasis, strabismus, diplopia, impaired accommodation, exophthalmos. On the opposite side: Wernicke-Mann position (flexor tone in the hand, extensor tone in the leg), the jackknife phenomenon, the Pharean component, clonus of the hands and feet, flexion of the wrist and protective reflexes, pathological synkinesis.
Claude syndrome
(dorsal mesencephalic syndrome, inferior red nucleus syndrome) occurs when the nucleus of the oculomotor nerve, superior cerebellar peduncle, or red nucleus is damaged. On the affected side, it is characterized by ptosis, divergent strabismus, and mydriasis.
Benedict's syndrome
observed with damage to the nuclei of the oculomotor nerve, the red nucleus, red nucleus-dentate fibers, and sometimes the medial lemniscus. On the side of the lesion, ptosis, divergent strabismus, and mydriasis occur, on the opposite side - hemiataxia, eyelid tremor, hemiparesis (without Babinski's sign).
Nothnagel syndrome
occurs with combined damage to the nuclei of the oculomotor nerves, the superior cerebellar peduncle, the lateral lemniscus, the red nucleus, and the pyramidal tract. On the side of the lesion, ptosis, divergent strabismus, and mydriasis are noted, on the opposite side - choreathetoid hyperkinesis, hemiplegia, paralysis of the facial and tongue muscles.
Central hemiparesis of the limbs
A generalized description of the changes occurring on the opposite side, with alternating syndromes, regardless of the location of the lesion.
On the opposite side: spastic hypertonicity, with a predominance of the phasic component, characterized by the “jackknife” phenomenon, Wernicke-Mann posture, clonus of the feet and hands, hyperreflexia and expansion of reflexogenic zones, the appearance of pathological reflexes (on the hand - Rossolimo, Zhukovsky, Bekhterev; on the foot – Babinsky, Rossolimo). Pathological synkinesias (global [accompany massive movements (coughing, sneezing), involuntary movements of the paralyzed limb are observed]; coordinating [involuntary cooperative movements in the paralyzed limb when performing voluntary movements in healthy muscles functionally associated with the paralyzed ones]); imitation [the paralyzed limb involuntarily repeats the movement healthy, although the same movement cannot be performed voluntarily] Pronounced protective reflexes: protective shortening; protective Remak reflex.
Text of the book “Clinical diagnostics in neurology”
4.11. Cross hemiplegia syndrome
Crossed hemiplegia syndrome is cross (in the right arm, left leg, or vice versa) paralysis or paresis. Its occurrence is associated with a limited focus located laterally at the border of the medulla oblongata and spinal cord in the area of the intersection of the pyramidal tracts. The fibers of the pyramidal tracts going to the cervical and lumbar enlargements intersect at different levels. More often, central paralysis (paresis) of the arm is observed on the side of the lesion, and central paralysis (paresis) of the leg is observed on the opposite side.
4.12. Alternating syndromes of the medulla oblongata
Alternating syndrome is a symptom complex that occurs as a result of unilateral combined damage to the nucleus (nuclei) of cranial nerves or their roots, as well as long pathways in the brain stem. As a result, on the side of the lesion, symptoms of damage to the cranial nerves are revealed, and on the side opposite to the lesion, conduction disorders (hemiparesis, hemihypesthesia, etc.) are revealed. Features of the clinical picture of alternating syndromes are determined by the localization of the pathological focus within the medulla oblongata, pons, and midbrain. Among the alternating syndromes of the medulla oblongata, the most common syndromes are Jackson, Tapia, Avellis, Schmidt, Collet-Sicart, Wallenberg-Zakharchenko, Babinsky-Nageotte.
Alternating Jackson syndrome.
This syndrome is associated with the name of the English neurologist D. Jackson, who described it in 1864 and 1872.
The clinical manifestations he described were very far from those that are currently commonly referred to as Jackson syndrome. The true clinical picture was first described by the Russian doctor A. Gukovskaya in 1895. The lesion is localized in the caudal parts of the base of the medulla oblongata, affecting the nucleus of the XII nerve and the pyramidal tract. The main cause of the development of the syndrome is thrombosis of the branches of the anterior spinal artery ( a. spinalis anterior)
.
1. Ipsilateral symptoms: peripheral paresis of the muscles of the corresponding half of the tongue and (possibly) the orbicularis oris muscle is determined, caused by damage to the nucleus of the XII nerve.
2. Contralateral symptom – central hemiparesis.
Alternating Tapia syndrome.
It was described by the Spanish otorhinolaryngologist AG Tapia in 1905. The lesion is localized in the caudal parts of the base of the medulla oblongata. Unlike Jackson syndrome, it is characterized by greater prevalence, affecting the nuclei of the XII and XI nerves, as well as the pyramidal tract. The etiological factors are similar to those in Jackson syndrome.
1. Ipsilateral symptoms:
– peripheral paresis of the muscles of the corresponding half of the tongue and (possibly) the orbicularis oris muscle, caused by damage to the nucleus of the XII nerve;
– peripheral paresis of the sternocleidomastoid and trapezius muscles due to damage to the nucleus of the XI nerve.
2. Contralateral symptom – central hemiparesis.
Alternating Avellis syndrome.
Described by the German otorhinolaryngologist G. Avellis in 1891. The lesion is localized in the tegmentum of the medulla oblongata in the region of the double nucleus and spreads to the base of the medulla oblongata, damaging
the nucl.
ambiguus (sometimes together with the nucleus of the XII nerve) and the pyramidal tract.
The syndrome occurs when branches of a.
fossae lateralis bulbi .
1. Ipsilateral symptoms:
– peripheral paresis of the muscles of the soft palate and vocal cord (sagging of the soft palate at rest, its insufficient mobility during phonation, deviation of the uvula to the healthy side, paresis of the vocal cord) due to damage to the nucleus ambiguus;
– peripheral paresis of the muscles of the corresponding half of the tongue and (possibly) the orbicularis oris muscle due to damage to the nucleus of the XII nerve.
2. Contralateral symptom – central hemiparesis.
Alternating Schmidt syndrome.
Described by the German physician A. Schmidt in 1892. The lesion is localized in the posterolateral parts of the tegmentum of the medulla oblongata or may be located outside the trunk, damaging the nuclei or proximal part of the roots of the IX - XII cranial nerves, as well as the pyramidal tract.
The development of the syndrome can be caused by vascular disorders in the anterior spinal artery (a. spinalis anterior)
, an extra-stem tumor in the area of the jugular foramen.
1. Ipsilateral symptoms:
– peripheral paresis of the muscles of the corresponding half of the tongue and (possibly) the orbicularis oris muscle, caused by damage to the nucleus of the XII nerve;
– peripheral paresis of the sternocleidomastoid and trapezius muscles due to damage to the nucleus of the XI nerve;
– peripheral paresis of the muscles of the soft palate and vocal cord due to damage to the nucleus ambiguus.
2. Contralateral symptom – central hemiparesis.
Collet-Sicard syndrome.
Described in 1922 by French neurologists FJ Collet and JA Sicard. Clinically manifested by damage to the IX, X, XI and XII cranial nerves due to unilateral pathology in the area of the jugular foramen and the hypoglossal nerve canal. The syndrome develops with unilateral pathological processes in the posterior cranial fossa, with fractures of the base of the skull in the area of the bone canals of the cranial nerves of the caudal group.
Alternating Wallenberg-Zakharchenko syndrome.
It was described in 1895 by the German doctor and pathologist A. Wallenberg, and in 1911 the Russian neurologist M. A. Zakharchenko added to the description.
The lesion is localized in the dorsolateral parts of the tegmentum of the medulla oblongata in its upper part. In the main variant described by Wallenberg, the following anatomical structures are affected: the nucleus or the initial part of the root of the nucleus ambiguus, the bulbar part of the nucleus of the spinal tract of the trigeminal nerve (nucl. tr. spinalis n. trigemini)
, the inferior cerebellar peduncle, suprasegmental sympathetic pathways from the center of sympathetic innervation of the eye
(centrum ciliospinale)
, spinothalamic tract.
1. Ipsilateral symptoms:
– peripheral paresis of the muscles of the soft palate and vocal cord due to damage to the nucleus ambiguus;
– dissociated disorders of surface sensitivity in the caudal and (or) middle zones of Zelder due to damage to the bulbar part of the nucleus of the spinal tract of the trigeminal nerve;
– cerebellar hemiataxia due to damage to the inferior cerebellar peduncle;
– Horner’s syndrome and (possibly) vegetative-vascular disorders in the face, neck, arm due to damage to the suprasegmental sympathetic pathways from the center of sympathetic innervation of the eye.
2. Contralateral symptom – hemihypesthesia of superficial types of sensitivity (excluding the face).
The main cause of the development of the syndrome is considered to be vascular disorders in the posterior inferior cerebellar or vertebral artery. Based on an analysis of several dozen observations, M. A. Zakharchenko came to the conclusion that this syndrome is characterized by a certain polymorphism. Therefore, they identified 5 types of syndrome, differing in the localization of the pathological focus and some clinical manifestations (Table 4.1).
Table 4.1
Types of dorsolateral alternating syndrome of the medulla oblongata according to M. A. Zakharchenko (1911)
Alternating Babinski-Nageotte syndrome.
Described in 1902 by the French neurologist G. Babinski and pathologist G. Nageotte.
The lesion is localized in the lateral part of the tegmentum and at the base of the medulla oblongata on the border with the pons. The main cause of the development of the syndrome is vascular disorders in the vertebral artery basin (a. vertebralis)
- the posterior inferior cerebellar artery
(a. cerebellaris inferior posterior)
, the artery of the lateral bulbar fossa
(a. fossae lateralis bulbi)
.
1. Ipsilateral symptoms:
– cerebellar hemiataxia due to damage to the posterior spinocerebellar tract as part of the inferior cerebellar peduncle;
– Horner’s syndrome and (possibly) vegetative-vascular disorders in the face, neck, arm due to damage to the suprasegmental sympathetic pathways from the center of sympathetic innervation of the eye (centrum ciliospinale)
.
2. Contralateral symptoms:
– central hemiparesis;
– hemihypesthesia of all types of sensitivity.
4.13. Syndromes of acute short-term ischemia of the brainstem
Unterharnscheidt syndrome.
In the literature, it is also referred to as a “shaving symptom”, since it often occurs in men while shaving when throwing their head back. The syndrome develops as a result of compression or spasm of the vertebral artery during sudden turns or tilting of the head, which leads to short-term ischemia of the structures of the reticular formation of the trunk and the cervical thickening of the spinal cord. It is clinically manifested by a fall with a short-term loss of consciousness (2 - 3 minutes) and subsequent short-term tetraparesis (3 - 5 minutes), which in some cases can reach the degree of complete immobility, and complete restoration of muscle strength can occur within 20 - 30 minutes. Therefore, the patient, upon regaining consciousness, first complains of weakness in the muscles of the arms and legs. The main causes of the development of the syndrome are vertebrogenic pathology of the cervical spine, atherosclerotic lesions of the vertebral artery, anomalies in the course of the vertebral artery and the structure of the circle of Willis, and volumetric pathological processes in the cervical spinal cord.
Drop attack syndrome, or “falling drop”.
It is also accompanied by a fall of the patient, however, unlike Unterharnscheidt syndrome, loss of consciousness does not occur. The syndrome manifests itself only by the loss of postural muscle tone with a fall, as a rule, to the knees, after which the patient can immediately stand up (“suddenly his legs gave way”). The genesis also does not exclude short-term ischemia of the caudal part of the trunk, however, unlike Unterharnscheidt syndrome, most authors associate the development of drop attacks primarily with ischemia of the cervical spinal cord.
Chapter 5 LESIONS OF THE PONTINE AND PONTINA GROUP OF CRANIAL NERVES
5.1. General anatomical characteristics of the pons
Varoliev Bridge (pons Varolii)
represents the anterior part of the rhombencephalon.
It has the appearance of a transversely located roller, gradually narrowing in the lateral direction. In front it is sharply delimited from the peduncles of the brain (pedunculi cerebri)
, in the back - from
the medulla oblongata
.
The conditional lateral border of the bridge is considered to be a longitudinal line passing through the exit site of the trigeminal nerve roots (n. trigeminus)
. The bridge has a ventral surface facing the clivus of the occipital bone and a dorsal surface facing the cavity of the fourth ventricle and representing the upper half of the rhomboid fossa. In addition to the roots of the trigeminal nerve, the roots of the abducens, facial and vestibulocochlear nerves also emerge from the substance of the brain.
The diameter of the pons is divided into three parts:
1) the ventral part (base) faces the slope of the skull;
2) the dorsal part (tegmentum) faces the cerebellum;
3) the trapezoid body (the beginning of the supranuclear auditory pathway) is located between the tegmentum and the base.
5.2. Nuclei of the pontine group of cranial nerves and other formations located in the pons
1. Nuclei of the cranial nerves (see Fig. 4.1):
– VIII – ventral and dorsal cochlear nuclei (nucl. cochlearis ventralis et dorsalis)
, vestibular nuclei of Bekhterev, Deiters, Schwalbe, Roller
(nucl. vestibularis superior, lateralis, medialis, inferior)
, ventral and dorsal nuclei of the trapezoid body
(nucl. ventralis et dorsalis corporis trapezoidei)
, nuclei of the lateral loop
(nucl. lemnisci lateralis)
;
– VII – nucleus of the facial nerve (nucl. n. facialis)
, pontine part of the nucleus of the solitary tract
(nucl. solitarius)
, lacrimal nucleus
(nucl. lacrimalis)
, superior salivary nucleus
(nucl. salivatorius superior)
;
– VI – nucleus of the abducens nerve (nucl. n. abducens)
;
– V – motor nucleus of the trigeminal nerve (nucl. motorius n. trigemini)
, sensitive nucleus of the trigeminal nerve
(nucl. pontinus n. trigemini)
, pontine part of the nucleus of the spinal tract
(nucl. tractus spinalis n. trigemini)
.
2. Core of the pontine gaze center.
3. Own nuclei of the bridge (nucl. pontis)
.
4. Nuclei of the reticular formation (nucl. formatio reticularis)
.
5.3. Conducting tracts of the pons
Ascending pathways:
1) spinothalamic tract (tr. spinothalamicus)
(spinal loop -
lemniscus spinalis
);
2) bulbothalamic tract (tr. bulbothalamicus)
(medial loop -
lemniscus medialis
);
3) nuclear-thalamic pathway (tr. nucleothalamicus)
(trigeminal loop -
lemniscus trigeminalis
);
4) auditory tract (tr. acusticus)
(lateral loop -
lemniscus lateralis
);
5) anterior spinocerebellar tract (tr. spinocerebellaris anterior)
(Gowers way).
Along with the main ones listed above, a number of other ascending pathways are also described in the bridge: spinotectalis (tr. spinotectalis)
, spinoreticular
(tr. spinoreticularis)
.
Descending pathways:
1) corticopontocerebella tract (tr. corticopontocerebellaris – tr. corticopontinus et tr. pontocerebellaris)
;
2) corticospinal pyramidal tract (tr. corticospinalis)
;
3) corticonuclear pyramidal tract (tr. corticonuclearis)
;
4) red nuclear spinal tract (tr. rubrospinalis)
;
5) roof-spinal tract (tr. tectospinalis)
;
6) vestibulospinal tract (tr. vestibulospinalis)
;
7) reticulospinal tract (tr. reticulospinalis)
;
 medial longitudinal fasciculus (fasciculus longitudinalis medialis)
medial longitudinal fasciculus (fasciculus longitudinalis medialis)
.
9) posterior longitudinal fasciculus (fasciculus longitudinalis posterior)
;
10) central tegmental tract (tr. tegmentalis centralis)
.
5.4. Pontine lesion syndromes
1. Motor, sensory, secretory disorders due to damage to the pontine group of cranial nerves or their pontine nuclei: VIII – central cochleovestibular disorders; VII - homolateral peripheral prosoparesis or facial hemispasm (with damage to the nuclei of the intermediate nerve - dry eye and ageusia of the anterior two-thirds of the tongue); VI – homolateral paresis of the external rectus muscle of the eye (if the pontine center of gaze is affected, gaze paresis to the ipsilateral side); V – dissociated disorders of superficial sensitivity in the oral zones of Zelder (partial damage to the pontine nucleus of the spinal tract of the trigeminal nerve), dissociated disorders of deep sensitivity on the entire half of the face (damage to the pontine nucleus of the trigeminal nerve), homolateral peripheral paresis of the masticatory and temporal muscles (damage to the motor nucleus of the trigeminal nerve).
2. Bilateral oculomotor disorders: gaze paresis or forced rotation of the eyes towards the lesion (if the pontine center of gaze is affected), or disturbances in the conjugate movements of the eyeballs (if the medial longitudinal fasciculus is affected).
3. Alternating syndromes of the pons.
4. Cerebellopontine angle syndrome.
5. Pseudobulbar palsy.
6. Acute pontine myelinolysis syndrome.
7. Herniation syndromes at the pons stage.
8. “Locked-in person” syndrome (see subsection 14.4).
Thus, among the above syndromes, oculomotor disorder syndromes - damage to the abducens nerve, pontine center of gaze, damage to the medial longitudinal fasciculus - occupy one of the leading places in cases of damage to the pons. However, it is more appropriate to consider them in the next chapter together with other oculomotor disorders, since the latter are characteristic of damage to the midbrain, as well as the III and IV cranial nerves.
5.5. Anatomy of the auditory analyzer pathways
The auditory analyzer provides the perception of auditory stimuli, the conduction of nerve impulses to the auditory nerve centers, the analysis and integration of information received in them. Receptors that perceive sound stimulation are located in the organ of hearing (organ of Corti). The organ of Corti is located in the cochlear duct and consists of inner and outer sensory hair cells, which are surrounded by supporting epithelial cells.
First neuron of the auditory pathway
represented by bipolar cells.
The bodies of these cells form a spiral ganglion (ganglion spirale)
, which is located in the spiral canal of the cochlea of the inner ear.
The central processes of bipolar neurons are collected in a bundle - the cochlear root of the vestibulocochlearis nerve (radix cochlearis n. vestibulocochlearis)
, which, connecting with the vestibular root
(radix vestibularis)
, enters the cranial cavity through the internal auditory canal.
Second auditory pathway neuron
located in the ventral and dorsal cochlear nuclei
(nucl. cochlearis ventralis et dorsalis)
.
The fibers of the cochlear root of the VIII cranial nerve end on them, which first enters the cerebellopontine angle and then into the substance of the brain (pons). The ventral and dorsal cochlear nuclei are located in the lateral corner of the rhomboid fossa, and their central processes go in the medial direction and participate in the formation of the trapezoidal body ( corpus trapezoideum
), separating the ventral and dorsal parts of the bridge.
A minority of these fibers end on the neurons of the ventral and dorsal nuclei of the trapezoid body (nucl. trapezoidei ventralis et dorsalis)
on their side, while most of the fibers approach the same formations on the opposite side.
In addition, part of the central processes of the nucleus of the cochlear nerve forms the medullary stripes of the fourth ventricle (striae medullares ventriculi quarti)
, which end on the dorsal nucleus of the trapezoid body of the opposite side.
Third auditory pathway neuron
located in the dorsal and ventral nuclei of the trapezoid body of its own and the opposite side, and its central processes form the lateral loop and end at the subcortical hearing centers.
A minority of the fibers end in the nuclei of the lower colliculi. Most of the fibers reach the second subcortical hearing center - the nuclei of the medial geniculate bodies of the diencephalon of its own and the opposite side. From the lower tubercles of the quadrigeminal, the tectospinal (tr. tectospinalis)
and tectonuclear
(tr. tectonuclearis)
pathways begin, which go to the anterior horns of the spinal cord and the motor nuclei of the cranial nerves, which provides unconditioned reflex motor responses to auditory stimuli.
Fourth neuron of the auditory pathway
located in the medial geniculate bodies, and its central processes pass through the posterior femur of the internal capsule and then, fan-shaped, are directed to the middle part of the superior temporal gyrus to the primary cortical field of the auditory analyzer (Heschl's gyrus).
The path from the medial geniculate body to the superior temporal gyrus is called auditory radiation (radiatio acustica)
. The cerebral cortex, according to the feedback principle, influences the subcortical hearing centers and indirectly influences the organ of Corti.
5.6. Structures of the sound-conducting and sound-receiving apparatus, differential diagnosis of their lesions
Sound conducting apparatus
carries out the delivery of sound vibrations to the receptor apparatus. This function involves the auricle, external auditory canal, tympanic membrane, chain of auditory ossicles, cochlear window membrane, perilymph, basilar plate and vestibule (Reissner's) membrane (outer and middle ear and fluid media of the inner ear).
Sound-receiving apparatus
carries out the transformation (transformation) of the energy of sound vibrations into a nerve impulse, its conduction to the centers of the cerebral cortex, analysis and comprehension of sounds. It is represented by the receptor apparatus, the spiral ganglion, the VIII pair of cranial nerves and its nuclei, central conductors and the cortical part.
The examination of the auditory analyzer by a neurologist has two main goals: establishing the very fact of hearing loss, determining the level of damage to the auditory analyzer (sound-conducting or sound-receiving apparatus). To achieve the first goal, a survey, speech study, and audiometric study are used. To establish the localization of damage to the auditory analyzer at the level of the sound-conducting or sound-receiving apparatus, studies using tuning forks, audiometric studies and a number of special tests are used.
The necessity and informativeness of studies using tuning forks should be especially emphasized, although the final conclusion in these cases is given after a special examination by an ENT doctor.
The following tests with tuning forks are used in clinical practice.
1. Rinne's experience
(R) – comparison of air and bone conduction. A sounding tuning fork C128 is placed with its stem against the mastoid process. After the subject’s perception of sound has ceased, the tuning fork (without exciting) is brought to the external auditory canal. If the subject hears vibrations of a tuning fork propagating through the air, the Rinne experience is positive (R+), and if not, then the result is considered negative (R–). With a positive Rinne experiment, air conductivity prevails over bone conduction by 1.5–2 times, and with a negative one, vice versa. A positive Rinne experience is observed in normal conditions and in cases of damage to the sound-receiving apparatus, a negative one – in cases of diseases of the sound-conducting apparatus.
2. Weber's experience
(W) – determination of the side on which the subject perceives the sound of the same tuning fork C128 more strongly when it is placed in the middle of the crown. Normally, the subject hears the sound of a tuning fork in the middle of the head or equally in both ears. If the sound-conducting apparatus is damaged, the patient feels a louder sound on the affected side (lateralization of the sound towards the worse-hearing ear). With lesions of the sound-receiving apparatus, lateralization towards the better hearing ear is revealed.
3. The Jelle experience
(G). With it, a sounding tuning fork is placed at the crown of the head and at the same time the air in the external auditory canal is condensed using a pneumatic funnel. If at the moment of air compression the subject feels a decrease in perception (due to deterioration in the mobility of the sound-conducting system due to its compression), then Jelle’s experience is considered positive (G+), which is possible both in normal conditions and in cases of pathology of the sound-perceiving apparatus. If there is no change in perception, then Jelle’s experience is negative (G–), which indicates ankylosis of the stapes, i.e., pathology of the sound-conducting apparatus.
4. Bing's Experience
(Bi). It is carried out to determine the relative and absolute conductivity of sound through the bone using a C128 tuning fork. In this case, bone conduction is examined first with the ear canal open, and then with the ear canal closed by pressing the tragus against the auricle.
Both in normal conditions and in cases of pathology of the sound-receiving apparatus, turning off air sound conduction prolongs sound conduction through the bone. If the sound-conducting apparatus is damaged, bone sound conduction remains the same with the external auditory canal open and closed.
5. Federici's experience.
The C128 tuning fork in the sounding state is first placed on the mastoid process, after the subject stops hearing the sound, the same tuning fork is moved to the tragus. A normally hearing person perceives the sound of a tuning fork from the tragus longer than from the mastoid process.
When sound conduction is disrupted, the opposite picture is observed.
For a more accurate idea of the nature (violation of sound conduction or sound perception) and the degree of these disorders, various audiometric methods are used. Pure-tone threshold audiometry is used as the main audiometric study in clinical practice. Through an air and bone telephone, sounds of different frequencies and intensities are delivered to the test subject's ear. The weakest sounds of a particular tone are recorded and audiogram graphs are compiled. With pathology of the sound-conducting apparatus, the thresholds for air conduction in the range of low and medium frequencies predominantly increase, the auditory thresholds for bone conduction remain quite good, as a result of which on the audiogram graphs there is a significant (so-called bone-air) gap between the threshold curves of bone and air conduction. With pathology of the sound-perceiving apparatus, the perception of high tones mainly suffers, and the bone-air gap is practically absent.