Brain glioma is the most common type of tumor that grows from glial tissue, which makes up the supporting cells of the nervous system. Gliomas account for about 60% of all tumors localized in the brain. The name of the types of gliomas - astrocytomas, ependymomas and others - comes from the name of the cells that form the tumor.
Services for the diagnosis and treatment of brain glioma are offered by the leading multidisciplinary medical center in Moscow - Yusupov Hospital. Positive treatment results are achieved thanks to the high professionalism of the oncology center’s doctors and advanced technologies used to combat brain tumors.
Classification
- Astrocytomas are the most common type of glioma, localized in the white matter of the brain. Depending on the type, astrocytic glioma of the brain can be fibrillary (protoplasmic, gemistocytic), anaplastic, glioblastoma (giant cell, gliosarcoma), pilocytic astrocytoma, pleomorphic xanthoastrocytoma, and subependymal giant cell astrocytoma.
- Ependymomas - can occur in 5-7% of cases of brain tumors, are characterized by typical localization in the ventricular system of the brain.
- Oligodendrogliomas account for 8 to 10% of all brain tumors and develop from oligodendrocytes.
- Chiasmal glioma - spreads along the optic nerve into the orbital cavity, can grow into the hypothalamus, and affect the third ventricle of the brain. This tumor causes endocrine imbalance, metabolic disorders, decreased vision, and is characterized by intracranial hypertension, depending on the location and size of the tumor.
- Mixed gliomas – oligoastrocytomas, anaplastic oligoastrocytomas.
- Neuromas make up 8 to 10% of tumors.
- Choroid plexus tumor is a rare type of glioma, occurring in 1-2% of cases.
- Neuroepithelial tumor of unknown origin - this group includes astroblastoma and polar spongioblastoma.
- Diffuse glioma of the brain stem is a tumor with a high degree of malignancy, cancer of the central nervous system. People of any age are affected, but the tumor is rare in adolescents and children. The survival prognosis for this type of tumor is poor. Diffuse glioma develops in the area of the brain in which all the important nerve connections are located, providing communication between the analyzing nerve centers of the brain and the impulses of the musculoskeletal system of the extremities. The tumor very quickly causes paralysis.
- Neuronal and mixed neuronal-glial tumor - occurs in extremely rare cases (up to 0.5%). This group includes gangliocytoma, ganglioglioma, neurocytoma, neuroblastoma, neuroepithelioma).
- Gliomatosis cerebri.
Types of gliomas
There are several types of gliomas, which are classified by the name of the cells from which they originate, as well as by other characteristics - molecular markers.
| Glial cells | Type of glioma | Grade of malignancy (WHO Grade) |
| Astrocytes | Piloid astrocytoma | I |
| Diffuse astrocytoma | II | |
| Anaplastic astrocytoma | III | |
| Glioblastoma | IV | |
| Gliosarcoma | IV | |
| Ependymal cells | Subependyoma | I |
| Myxopapillary ependymoma | I | |
| Ependymoma | II | |
| Anaplastic ependymoma | III | |
| Oligodendrocytes | Oligodendroglioma | II |
| Anaplastic oligodendroglioma | III |
Piloid astrocytoma (WHO Grade I) is a benign, slow-growing tumor. More common in children and young patients. Characteristic of these tumors is the presence of cysts. Piloid astrocytomas are most common in the cerebellum. Localization in the cerebral hemispheres is more typical for patients in the older age group. Treatment is carried out surgically. Despite their benign nature, radical surgical treatment of piloidal astrocytomas can be difficult when located in vital structures such as the brainstem. In such cases, after confirmation of the histological diagnosis, radiation treatment may be used. If complete tumor removal is possible, no additional treatment is required.
Diffuse astrocytoma – (WHO Grade II). These astrocytomas are characterized by infiltrative growth, that is, the absence of boundaries between the tumor and the healthy brain. However, the surgeon should always strive to remove as much tumor tissue as possible. Most often, these tumors occur in young patients and are located in the cerebral hemispheres. Despite their conditionally benign nature, these tumors can become malignant over time, that is, become malignant.
Anaplastic astrocytoma (WHO Grade III) is a malignant glioma. People aged 35 to 50 years are at risk. It is at this stage that severe symptoms are present, which forces you to consult a doctor. Combined treatment: surgical removal followed by chemotherapy and/or radiation therapy.
Glioblastoma is the most malignant brain tumor and, unfortunately, a common primary brain tumor. Glioblastomas account for approximately 20% of the total number of all primary intracerebral tumors. The tumor is characterized by rapid and aggressive growth. Early signs are usually absent, but as carcinogenesis progresses, a corresponding clinical picture appears. The main type of treatment is surgical removal of the tumor followed by radiation treatment and chemotherapy. Glioblastoma is prone to frequent recurrence, even with combined treatment, so the prognosis is unfavorable.
Degrees
There is a WHO classification, according to which gliomas are divided into four grades:
- Grade I – slow-growing benign glioma, which is associated with a long life expectancy;
- Grade II – slowly growing “borderline” brain glioma, which tends to progress to grades III and IV;
- III degree – malignant glioma;
- IV degree – fast-growing glioma of the brain: the life expectancy of patients with this diagnosis is significantly reduced.
Causes
There are congenital and acquired causes that determined the development of the pathological focus. If the processes of neuroglial proliferation are associated with congenital anomalies, intoxications, infections, injuries suffered during the perinatal period, the prognosis is usually unfavorable. Pediatric patients rarely survive beyond 3 years of age.
For example, in children diagnosed with cerebral palsy, cystic-glial changes are detected during neuroimaging in 32% of cases and are the most significant clinical criterion of pathology. In adults, the progression of cystic gliosis transformation can often be stopped. Main causes:
- Processes of ischemia and hypoxia.
- Intracranial hemorrhages.
- Tumors localized in brain tissue.
- Past neuroinfections.
- Birth injuries.
- Traumatic brain injuries.
- Surgical interventions in the area of the skull and its internal structures.
- Intoxication (chronic, acute).
- Metabolic disorders.
- Chromosomal mutations.
- Cerebrovascular pathologies.
Hereditary degenerative diseases and demyelinating diseases can provoke the proliferation of neuroglia. Pathologies of the vessels that make up the circulatory system of the brain are one of the common causes of cystic-gliotic lesions. If pathological processes are caused by vascular sclerosis, against the background of circulatory disorders, the development of severe conditions (cerebral infarction, stroke) with the subsequent formation of cystic-gliotic areas is possible.
Symptoms
The symptoms of brain glioma depend on the location of the tumor, its size, and it consists of general cerebral and focal symptoms.
Most often, brain glioma manifests itself as persistent and constant headaches, in which patients experience nausea and vomiting, after which there is no relief, as well as convulsions.
In addition, depending on which part of the brain is affected by glioma, patients have speech impairment, weakened muscles, and may experience paresis and paralysis of the arms or legs, face and other parts of the body. Visual or tactile function, coordination of gait and movements may be impaired.
The psyche may change, and the development of behavioral disorders is often noted. In addition, memory and thinking are impaired in patients with brain gliomas. Due to impaired circulation of cerebrospinal fluid, intracranial hypertension and hydrocephalus develop.
Diagnostics
Diagnosis of brain glioma is based on the results of a thorough neurological examination and other special diagnostic tests.
First of all, the doctor at the Yusupov Hospital Oncology Center assesses the condition of reflexes and skin sensitivity, and motor function of the limbs. If the patient complains of deterioration in visual function, he is prescribed a consultation with an ophthalmologist.
The neuromuscular system is assessed using instrumental diagnostic methods - electromyography and electroneurography. In addition, a lumbar puncture is performed to identify atypical cells in the cerebrospinal fluid. This study is also used for ventriculography and pneumomyelography.
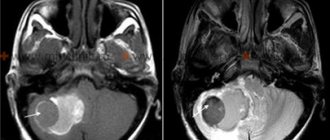
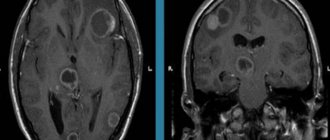
Modern imaging methods that provide layer-by-layer images of brain tissue are of great importance in the diagnosis of brain tumors. These include computed tomography (CT), magnetic resonance imaging (MRI). These studies are considered quite safe and very informative; they help determine the location, size, shape and structure of the tumor.
To determine the displacement of the midline structures of the brain, an ultrasound examination of the brain (M-echo) is performed.
Additionally, cerebral contrast angiography (x-ray examination of cerebral vessels), electroencephalography, scintigraphy and PET may be prescribed.
Make an appointment
Definition of pathology
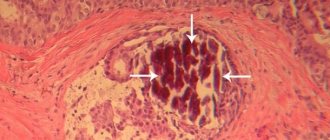
Organic lesions of brain tissue are often accompanied by cystic changes. Pathological processes occurring in brain tissue lead to changes in its structure. Transformation of the structure is manifested by a decrease in the number of fibers, damage to myelin, a change in the volume of intercellular space, and the replacement of neurons with glial cells.
Cystic-glial transformation, which occurs in the brain, is a process during which neuroglial proliferation occurs, which is usually associated with damage and death of neurons. The mechanism of compensatory replacement of damaged nervous tissue is a protective reaction of the body, which tries to restore lost areas of the brain matter and their functions.
Cystic-glial growths also play the role of a protective barrier that separates healthy tissue from the pathological focus - tumor, abscess, necrosis. The formation of cystic areas interferes with normal blood flow, which can provoke ischemic and atrophic processes in nearby tissues.
Treatment
Like any malignant tumor, brain glioma is treated with three main methods that are used in modern oncology - surgery, radiation therapy (including radiosurgery) and chemotherapy.
The gold standard treatment for brain glioma is surgery. If the tumor is operable, surgery is performed to remove the tumor.
Radiation therapy is performed before and after surgery. For inoperable tumors (if the glioma is localized in a hard-to-reach place), this method is used as a separate method. Today, traditional radiation therapy has been replaced by stereotactic radiosurgery.
Chemotherapy treatment of glioma can be used both preoperatively and postoperatively.
Surgery
The operation to remove malignant glioma is open, involving craniotomy, during which the skull is opened. The main goal of surgery is to remove as much of the tumor as possible while leaving healthy brain tissue intact, thereby preventing neurological damage. A certain localization of gliomas allows the effect of surgical treatment to be achieved up to 98%.
No operation to remove a tumor guarantees a 100% result, since there is always a possibility that cancer cells remain in the brain tissue. However, surgical intervention eliminates compression of surrounding brain tissue and the symptoms of glioma, as well as restores cerebrospinal fluid circulation if intracranial hypertension is present.
The effectiveness of surgical treatment of brain glioma largely depends on the skill and experience of the operating specialists. Treatment of brain tumors at the Oncology Center of the Yusupov Hospital is carried out using high-precision tomographs and neuronavigators, thereby minimizing the likelihood of a relapse of the disease.
Radiation therapy
Radiation therapy may be given before surgery to shrink the tumor before excision, or after surgery to kill any remaining tumor cells.
In addition, this method can be used as an independent method when the tumor is localized in a hard-to-reach place, which prevents its surgical removal. In this case, radiation therapy does not completely destroy the tumor, but can significantly stop its growth.
Traditional radiation therapy is accompanied by a number of undesirable effects: patients experience nausea, decreased appetite, and increased fatigue. At the site of radiation exposure there is a high probability of hair loss and the development of radiation dermatitis. As a rule, side effects of radiation therapy appear 10-14 days after irradiation.
In addition, late complications of radiation exposure are known: patients experience memory impairment to varying degrees, and radiation necrosis may develop (scar tissue forms around the dead tumor tissue).
Radiosurgery
Due to the fact that surgical treatment of brain tumors does not guarantee a complete cure, a relapse of the disease may occur after surgery. Therefore, it is advisable to use additional treatment methods - radiation therapy and chemotherapy. As a rule, relapses are localized at the borders of healthy tissue with the area where the tumor was removed. In such cases, it is recommended to use radiosurgery: cyber knife, gamma knife, Novalis.
Radiosurgery is an innovative method of radiation therapy, the essence of which is to irradiate a glioma with a beam of radiation from different angles, which ensures that radiation reaches the tumor and minimal irradiation of soft tissues.
During the procedure, the position of the patient's head and the location of the tumor are constantly monitored using computed tomography or magnetic resonance imaging, so that the radiation beam is directed exclusively to the malignant neoplasm.
This method is non-invasive, as no incisions are required to perform it. Thanks to this, there is no risk of intraoperative complications and side effects associated with traditional radiation therapy.
In addition, radiosurgery is an absolutely painless method that does not require anesthesia or preparatory measures, and there is no recovery period. The only limitation to radiosurgery is the size of the tumor.
It is important to understand that the effect of radiation therapy occurs gradually, unlike surgery. However, radiosurgery is often the only alternative treatment for inoperable brain gliomas.
Treatment options.
Gliosis cannot be cured. The main goal of the therapy, regardless of the methods, is to prevent further progression of the pathology.
Traditional methods.
To stop the development of pathology, the following groups of drugs are used:
- Aimed at activating metabolic processes in brain tissues, improving nutrition (Actovegin, Vinpocetine).
- Anti-platelet aggregation (aspirin-based).
- Strengthening vascular walls.
- Nootropic – to increase the stability of the central nervous system (Piracetam).
- Preventing the progression of atherosclerotic processes.
- Analgesics for headaches.
Surgical intervention is practically not used in treatment. It is advisable to perform surgery when patients experience epileptic seizures, convulsions, and dysfunction of internal organs.
The essence of the intervention is to perform a shunt and remove cerebrospinal fluid, which accumulates due to the presence of scar formations.
In case of multiple foci, surgical intervention is also not used - lifelong drug treatment is prescribed.
Ethnoscience.
Any folk remedies can be used only after consultation with a specialist. The treatment is based on the use of agents that improve blood circulation. Tinctures and decoctions of clover and hemlock are used.
The main goal of therapy is to eliminate the cause that provoked the pathological changes. In no case can traditional medicine recipes act as the only method of treatment.
It is recommended to arrange fasting days and give up bad habits - this will help cleanse the body of toxins.
Treatment of glioma at Yusupov Hospital
Oncologists at the Yusupov Hospital have enormous experience and effective methods of treating cancer. An individual treatment program is drawn up for each patient, based on the results of a thorough diagnostic examination. The Oncology Center of the Yusupov Hospital is equipped with innovative equipment for high-quality diagnosis and treatment of gliomas and other brain tumors.
An appointment with an oncologist can be made by calling the Yusupov Hospital or online on the website using the feedback form. The coordinating doctor will answer all your questions and tell you about the cost of medical services and the conditions for hospitalization of the patient.
Make an appointment