Many functions of the human body continue to function after death for several minutes, hours or even weeks. This sounds like science fiction, but it is a documented fact. Nails and hair grow for several days after death, and skin cells also function. It has been proven that the brain continues to function for some time. So how long does the brain live after a person’s death?
Controversies and theories
Numerous studies have been carried out, the results of which were the statement that the human brain continues to function for 4-6 minutes after the death of the body. Many scientists have argued about how a person sees and relates to his own death and still cannot come to a common conclusion.
Some doctors believe that the individual’s mind dies immediately, while others believe that it continues to work indefinitely. Recent testing has shown that after death, the work of the central nervous system does not stop. Therefore, in a state of clinical death, a person can be aware of what happened to him, because consciousness continues to function.
Modern medicine has reached a high level of development. New devices can keep the body in working condition (pumping blood and oxygen) for years. Therefore, a reasonable question arose: how long does the brain live after death, and what can be considered death in general? Its main symptom is the death of neurons, which leads to the loss of the individual’s personality.
How long does the brain live without oxygen?
22.09. Exclusive No comments 10068 views, 36 — today Print article
Between 30-180 seconds of oxygen deprivation, you may lose consciousness.
At the one minute mark, brain cells begin to die.
After three minutes, neurons suffer more damage and long-term brain damage becomes more likely.
After five minutes, death becomes inevitable.
After 10 minutes, even if the brain remains alive, coma and long-term brain damage are almost inevitable.
Dying from a scientific point of view
A serious illness or fatal injury leads to exhaustion of the body and the development of a thermal state. As a result, the functioning of all organs and systems is disrupted.
At this stage, timely intervention by doctors with the help of intensive care can help return the body to normal.
If resuscitation does not give a positive result, a preagonal state occurs, the main characteristics of which are:
- decreased blood pressure;
- weak brain response to stimuli;
- slow heart rate;
- weak breathing.
The body uses all its strength to correct the situation. Therefore, in a state of death agony, a person may feel improvement, but this lasts only a moment. The central nervous system cannot cope with its work, so the pressure can be restored and breathing can return to normal.
The body spends its last strength on this, after which clinical death occurs. There is no breathing, the heart does not beat, all metabolic processes in the cells slow down and stop. The body lacks oxygen, the brain suffers the most. After the actual death of the body, the stored nutrients last no more than 6 minutes. This is exactly how long the brain works after cardiac arrest.
If, within 6 minutes after cardiac arrest and lack of breathing, the necessary actions for resuscitation are carried out, which will prevent necrosis of organ cells, then the person can be brought back to life.
If biological death has occurred, that is, the cerebral cortex has died, then this is irreversible. With the help of the device, you can maintain the heartbeat and ventilate the lungs for some time, but this is no longer a sign of life.
The Last Fireworks: What Happens to the Body When We Die
As a patient approaches death, changes occur in his body. They concern breathing, blood circulation, consciousness. We explain in detail what happens: if we understand death, perhaps we will be less afraid of it.
Author: Jacob Zimmank
The author of the article is a former employee of the palliative care service, which supervises dying people at home. He was amazed at how calmly many people faced their own death.
When does dying begin? At what point does a person begin his path to death?
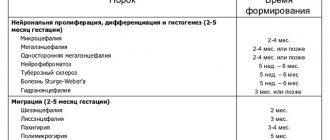
Dying begins long before we are born. It is laid in the womb, in a cluster of cells from which the unborn child is formed. Some cells are redundant and need to make room for new ones. This is the only way the child’s organs can appear. It is due to this that there are only two kidneys, and only ten fingers on the hand. The genome of each cell already contains programs that act as a kind of “catapult”. It turns on at the moment when the cell becomes unnecessary or dangerous for the body. In this case, the cell voluntarily destroys itself.
Becoming a person is a process that involves both life and death. According to palliative medicine doctor Jean-Domenico Borasio, death is “a necessary condition so that we can, in principle, be born as viable organisms.”
“What we know for certain is that a person does not die suddenly, overnight” - Jean-Domenico Borasio, palliative care doctor
Death is omnipresent - but once we are born, we forget about it. And, if all is well, then death will appear in our lives again only after a few decades. Often this will be a condition that cannot be cured: cancer, heart disease, or kidney disease that means they can no longer cleanse the blood. And then the process of dying begins.
“What we know for certain is that a person does not die suddenly, overnight. The organs of the human body stop functioning gradually, not all at the same time, and then at some point their work stops,” says Dr. Borasio. As a result of the chain reaction, the liver, kidneys, lungs and heart stop working.
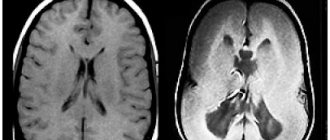
There are a variety of diseases, but at the end of life everything always follows the same pattern: the heart stops beating, breathing stops and, last of all, consciousness fades away. At the same time, it is very difficult to separate the work of the heart and brain. If the heart stops pumping oxygenated blood, brain cells begin to die within seconds. And after a few minutes, brain death occurs: at this moment the EEG will show a straight line instead of the usual curves and teeth. The reflexes that control the deep parts of the brain responsible for breathing, swallowing and consciousness also stop working. Thus, when the heart stops, the brain also stops working.
It also happens the other way around. The brain contains centers that regulate all vital functions: blood pressure, heart function, breathing. If these centers are damaged, breathing will stop and the heart rhythm will be disrupted. Often this damage occurs when intracranial pressure rises sharply as a result of a car accident or accident. The bones of the skull are hard, so with a strong blow, the soft tissue of the brain is squeezed into the only natural opening in the skull - the foramen magnum. Through it, the cranial cavity communicates with the spinal canal (the spinal cord passes into the brain stem). If the brain stem is pinched or damaged, the person dies.
There are no clear signs, but there are general patterns
Dying people live the last years, months and days of their lives in different ways. “The dying process is very individual,” says Lukas Radbruch, president of the German Society for Palliative Medicine and professor at the University Hospital Bonn. It often lasts for months or even years. Doctors divide dying into three stages: at the beginning comes the “terminal” stage, which lasts one to two years. At this time, the functioning of individual internal organs gradually decreases, and the dying person increasingly experiences fatigue. This is followed by the “pre-final” stage, which can last several weeks or months. At this time, symptoms such as shortness of breath and pain appear. And finally, the “final” stage - the last days. The patient stops eating and drinking and slowly fades away. “It is important to remember that this division of dying into stages is nothing more than a convention,” notes Radbruch. It is important for providing treatment and care, but does not provide an accurate picture and “does not help determine when the patient will die.”
“It used to be believed that the approach of death was indicated by pale skin in the nasolabial triangle,” says Radbruch. But this is also an unreliable sign. Currently, research that allows us to accurately determine the time of death is at an early stage. Some scientists are testing blood samples for markers that can be used to calculate remaining life expectancy. Radbruch says the best thing to do is ask the attending physician: Would she be surprised if she learned that the patient died that night or next weekend? If the doctor says that she is not surprised, then it is time to prepare for death.
Part 2. Death rattle
Although dying is a highly individual process, there are certain physical changes that are common to most patients (Palliative Care Review: Plonk & Arnold, 2005). As we approach death, there are more and more similar features, although the cause of death may be different. The dying are exhausted, have difficulty breathing and experience pain. Breathing changes: at first it becomes shallow, then intermittent, but after a while the dying person can again take a deep breath.
Doctors suggest that by this time the centers of the brain responsible for breathing have already been affected. They react late to the presence of carbon dioxide in the blood, allowing it to accumulate in large quantities. In some cases, breathing noises occur, one of which used to be called the “death rattle.” Due to the inability to expectorate and clear the throat, secretions accumulate in the pharynx and bronchi, which affects the passage of air flow during breathing.
The death rattle is often a terrible sound, but there is no evidence that the dying person is suffering at this moment. The same applies to an increase in the level of carbon dioxide in the blood - it is assumed that this has a rather calming and soporific effect. The death rattle (as the name suggests) indicates that death is imminent (American Journal of Hospice and Palliative Medicine: Morita et al, 1998). With very little time left, wheezing may become uncontrollable.
In addition, in the last days and hours before death, changes in blood circulation are observed. The body tries to deliver the small amount of oxygen that the heart is still able to pump through the blood to vital organs. “The pulse weakens and is often barely palpable, the hands become cold and the lips may turn blue,” explains Lukas Radbruch. “It’s a stress reaction.” In some cases, the heart begins to beat faster, the blood pressure drops, and a slight fever may even appear.
When consciousness fades
Radbruch says: “Someone remains conscious until his last breath. Another may experience anxiety and even hallucinations. And the third one just quietly fades away.”
There are enough reasons for such changes. On the one hand, due to uneven flow of blood and oxygen, brain metabolism is disrupted. On the other hand, some organs stop working, and because of this, toxic substances accumulate in the blood. For example, urea, which is excreted through the kidneys, can damage nerve cells in high concentrations. (But the dying person does not suffer from this either. Oblivion caused by a high concentration of urea in the blood is similar to anesthesia - it does not hurt the person, it is even pleasant.)
In addition to urea, ketone bodies accumulate in the blood of a dying person in large quantities, which also affect a person’s consciousness. They are produced from fat and, in conditions of energy deficiency, are used by the body as a substitute for glucose, which is necessary to nourish the brain and muscles. This is exactly what happens when dying: a person stops eating, but does not experience hunger (JAMA: McCann et al., 1994).
When dying, many patients quietly fade away or, on the contrary, become excited and whisper something excitedly. It may seem that they have already left this world, but despite this, “we must treat the dying as if they understood everything,” emphasizes Lukas Radbruch. “We don’t know exactly how much they can take in.”
Many patients continued to perceive what was happening even after cardiac arrest. This is evidenced by the results of a large study. Scientists interviewed 140 people from the UK, Austria and the US who had experienced cardiac arrest. Nine percent of those surveyed reported having had a near-death experience such as feeling fear, seeing a light or seeing family members.
Two of the respondents remembered the process of their own resuscitation. One of them talked about watching the doctors’ actions from above, from the corner of the room. He remembers that the doctors turned on the defibrillator and tried to “start” the heart, make it beat at the right rhythm again. And this coincided with what was happening in reality. It is interesting that the patient regained consciousness only a few minutes after cardiac arrest.
Last fireworks
When the heart stops and stops supplying the brain with oxygen, nerve cells do not die immediately. On the contrary, their activity increases sharply. This was reported by scientists who studied the electrical activity of the brain in laboratory rats (the rat’s brain is in many ways similar to the human brain). A few minutes after the rodents' hearts stopped beating, a burst of electrical activity could be observed—exceptionally strong. “This may explain why the memories of patients who have experienced clinical death are so real and accurate,” writes one of the study authors, anesthesiologist George Mashour of the University of Michigan Medical School.
When the heart stops, a real fireworks display occurs in the brain. Nerve cells release enormous amounts of norepinephrine, which affects the frontal lobes of the brain and sharpens attention. There is also a release of serotonin, so hallucinations and mystical insights are possible. And at the very last moment, dopamine arrives from the midbrain. It is responsible for the feeling of satisfaction, gives a feeling of warmth and joy. Perhaps even happiness.
The original interview is on ZEIT ONLINE.
We thank Vera Foundation volunteer Veniamin Sapozhnikov for translating this article.
How to support hospice patients?
It is very easy to support hospice patients. You can sign up for monthly donations (by checking the box next to “I want to donate monthly”) or make a one-time donation :
Thank you always.
Share
Tweet
Share
Share
SIMILAR
How does lack of oxygen affect the brain?
There are two forms of oxygen deficiency:
- Anoxic damage. The brain is completely deprived of oxygen through sudden cardiac arrest, suffocation or any other injury.
- Hypoxic damage. He receives a smaller dose than is needed for full functioning.
The organ will not be harmed by a few seconds without oxygen, so people can dive or live with breathing problems.
How long does the brain live without oxygen? The onset of anoxic damage depends on many factors: the condition of the organ, the level of oxygen in the blood at the time of injury, and the general condition of the body. A minute without oxygen can cause serious injuries, and the condition only gets worse:
- 180 seconds will result in loss of consciousness;
- neurons begin to die after 1 minute without oxygen;
- 3 minutes lead to serious consequences;
- 5 minutes is inevitable death;
- 10 minutes - coma, while the brain can still function, but suffers severe damage;
How many minutes does it take for the brain to completely die? 15 minutes is enough for irreversible consequences.
If you train your body, you can hold your breath for up to 22 minutes, and the brain does not suffer any damage.
Diagnostic criteria: clinical signs of brain death
The Ministry of Health of the Russian Federation for diagnosis requires that one be guided by the following criteria indicating brain death.
The patient experiences a complete, stable loss of consciousness with a stage IV coma (extreme coma). An atonic state is determined, as evidenced by the lack of normal tone in all skeletal muscles.
With brain death, there is no response to intense painful stimuli. The patient does not experience reflex pupillary reactions to light when the possibility of previous use of pupil dilators is excluded. The eyeballs are completely static.
The criterion for extreme coma is the absence of the corneal (corneal) reflex. When the cornea is irritated, the unconditioned reflex of closing the palpebral fissure does not occur.
When examining a person, a negative phenomenon called “the head and eyes of a doll” is recorded. This way, oculocephalic reflexes do not occur during testing. When the subject's head is abducted, the eyeballs do not deviate in the opposite direction. They move simultaneously with the head as if they were fixed in one position.
When performing a cold test, oculovestibular reflexes are not detected. When ice water is introduced into the ear canal, the abduction of the eyeballs towards the irrigated ear canal is not recorded.
With brain death, a person does not have pharyngeal and tracheal reflexes. This is confirmed by performing tests by moving the endotracheal tube in the upper respiratory system. To determine the diagnosis, the pharyngeal and cough reflexes must also be absent.
The patient is not able to carry out independent (spontaneous) breathing. This is confirmed by an apnea test. When the mechanical ventilation equipment is disconnected, a person does not experience spontaneous inhalation and exhalation.
When performing diagnostics, it must be taken into account that the diagnosis of “brain death” is prohibited if there is a suspicion of poisoning or overdose of drugs that have a depressing effect on the central nervous system. The basis for additional research is the fact of endogenous intoxication provoked by acute renal or liver failure. Extreme coma is excluded if there are symptoms of cardiogenic shock. A more detailed diagnosis of a person’s condition is required if, when assessing his neurological status, decortication or decerebrate postures are observed. This diagnosis cannot be made if the patient experiences convulsive movements indicating electrical activity in the brain. The reason for performing neuroimaging diagnostic methods is the presence of spinal reflexes. It should be taken into account that spinal cord reflexes are preserved partially or fully in 65% of patients with angiographically recorded brain death. The diagnosis is not made when hypothermia is determined with a core body temperature below 32°C.
To confirm the diagnosis or in the presence of a clinical picture of conditions simulating brain death, the following studies are carried out:
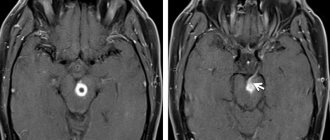
- electroencephalography - a study of the electrical activity of the brain to confirm or exclude the bioelectrical activity of neurons;
- cerebral angiography is a method of X-ray examination of cerebral vessels, allowing to confirm or refute the cessation of intracranial blood flow and cerebrospinal fluid pulsation;
- transcranial Dopplerography is a non-invasive ultrasound method for assessing the presence and speed of blood flow through intracranial vessels;
- toxicological analysis - measures to determine the presence of toxins in the body;
- blood tests.
Why is oxygen so important?
Of the total body weight, gray matter occupies only 2%, but at the same time, for full-fledged work, it consumes 20% of all gas entering the body. Without oxygen, the brain will not be able to do its job.
Glucose is needed to perform any activity, such as the neurons that control all body functions. Without oxygen, cells will not be able to produce this substance and subsequently convert it into the necessary energy.
If you deprive the brain of oxygen, the cause of its death will be the inability to nourish the cells, because there simply will not be energy (glucose) for this.
Alarming symptoms
Due to oxygen deficiency, circulatory disorders occur. This provokes the development of single and complex disorders in the body from memory impairment to paralysis. An acute lack of oxygen can be recognized by the following symptoms:
- speech disorder;
- decreased sensitivity;
- tingling in the limbs;
- disruption of the gastrointestinal tract;
- uncontrolled coordination;
- spots or “stars” before the eyes.
In rare cases, numbness of one part of the face, nausea and profuse vomiting are possible. Manifestations rarely occur alone; more often, a person with oxygen starvation experiences a number of symptoms. With mild symptoms, darkening of the eyes, dizziness, irresistible drowsiness, and nausea appear.
Chronic fasting is characterized by weakness, poor concentration and dizziness.
Symptoms can occur both during a stressful situation, overload, and in a calm state. It is provoked by diseases of the central nervous system, circulatory disorders, infectious lesions, and overwork. An incorrect lifestyle and bad habits can also have an impact.
The level of cholesterol in the blood affects the functioning of the cardiovascular system, the functioning of the heart, and the condition of the veins. You can normalize the amount of organic compounds in the blood with the help of a special diet. Read more in the article: “excellent cholesterol-lowering foods.”
What confirms brain death?
The main criteria for death may be the following:
- Lack of response to external stimuli.
- No brainstem reflex:
- emetic;
- pupil reaction to light;
- corneal reactions;
- no breathing.
But such indicators cannot always indicate the occurrence of death. It is mandatory to measure the pupils, which must be fully dilated or of average size. If the pupils are narrow, this may indicate the presence of vital processes.
In general, it is very difficult to determine this condition; any mistake will cost the patient’s life. There are basic criteria for organ death, which were formulated in 1968 at Harvard. All neurologists and resuscitators adhere to them and always use them before turning off the ventilator and declaring death.
First, each patient is diagnosed with a disease, based on which various causes are identified that led to the death of the human brain. Afterwards, all conditions that are externally similar to death, but can be reversible, are necessarily excluded:
- overdose of medications;
- poisoning of the body with toxins;
- dysfunction of the endocrine system.
After this, doctors determine the symptoms of organ stoppage:
- coma;
- no reaction to pain and irritants;
- no reaction of pupils to light;
- absence of reflexes of the pharynx, trachea and eyeball.
Also, a test is carried out for the presence of breathing - the blood is saturated with gases, controlling their quantity, after which the mechanical ventilation is stopped, and the level of carbon dioxide in the arteries is measured. The result is considered positive at 60 mmHg. Art. and lack of breathing. If breathing resumes, the lungs are ventilated again and try to restore the person’s vital functions.
Another stage is monitoring a person for 6 hours with primary brain damage. They check all parameters, the presence of a reaction, and monitor all changes that may appear in the presence of brain activity.
Diagnostics
When diagnosing, the doctor must collect anamnesis. He must find out how long ago the patient fell into such a dangerous state, under what conditions he lost consciousness, whether he had speech or motor activity
It is important to know what event preceded the loss of consciousness. An examination is carried out by a neurologist, he necessarily assesses the patient’s level of consciousness and checks his reflexes
Body temperature must be measured. If the temperature is below 32.2°C, it may distort the picture and show a false death. In this case, the person may be alive, but tests will show the opposite, since physiological processes literally freeze from the cold.
A blood test is prescribed that will help determine whether the metabolism is disturbed, whether there is hormonal dysfunction, and at what level the glucose levels are.
To correctly diagnose brain death, inpatients resort to instrumental research:
- encephalogram (EEG);
- contrast study of cerebral vessels;
- test with irritation of the eardrums (ice water is dripped onto them through the ear canal);
- apneic oxygenation test.
Oxygen starvation is extremely destructive for neurons, even if it is not long-term. Literally after a few minutes of complete lack of oxygen supply, tissues begin to die. The electroencephalogram in this case will show a zero line. This means that there is no brain activity at all.
Encephalography examines brain activity. In this case, the device registers biocurrents, their work is reproduced on paper in the form of curves.
The diagnostic protocol also includes the study of cerebral vessels using a contrast agent. It cannot always be accomplished, as there may be financial restrictions, and sometimes there is simply no equipment. The essence of the test is that a contrast agent is injected, which enters the brain vessels through the bloodstream and identifies possible areas of necrosis. If the brain is dead, the substance does not enter its vessels. This is one hundred percent confirmation of death.
Apneic oxygenation involves temporarily removing the patient from a ventilator. The goal is to observe whether spontaneous respiratory movements have appeared. The monitor monitors the level of carbon dioxide in the blood. It is carbon dioxide that stimulates the body to produce breathing movements. If after 8-10 minutes breathing does not appear, and the level of CO2 in the blood jumps by 20 mm Hg. Art. higher than the original, we can definitely talk about death.
From the editor: What pathologies are accompanied by dizziness with blocked ears
How long does the brain survive after cardiac arrest?
Conducted studies have shown that the activity of the central nervous system in the absence of a heartbeat lasts differently for each individual person. Therefore, it is impossible to say exactly how long the brain lives after cardiac arrest. When the oxygen supply instantly stops, it is impossible to calculate the duration of clinical death, which leads to its death.
The neurons that suffer the most are those that begin to die after 10 minutes without recharge. But in fact, these cells can continue to work. There were cases when, after resuscitation, already dead areas began to function as before again.
Organ damage due to lack of oxygen depends on many indications. After quality therapy, some damage may be compensated or disappear. If he has been without oxygen for a long time, the consequences may include:
- damage to specific areas (loss of the ability to speak, but the patient understands the language);
- change in character;
- memory problems;
- loss of coordination (some people could no longer write or walk);
- impaired perception of pain;
- behavioral changes, incontinence, aggression;
- the occurrence of chronic pain when there is no injury (occurs when the organ cannot correctly process the information received);
- mental illness.
Diagnostics
When diagnosing, the doctor must collect anamnesis. He must find out how long ago the patient fell into such a dangerous state, under what conditions he lost consciousness, whether he had speech or motor activity
It is important to know what event preceded the loss of consciousness. An examination is carried out by a neurologist, he necessarily assesses the patient’s level of consciousness and checks his reflexes. Body temperature must be measured
If the temperature is below 32.2°C, it may distort the picture and show a false death. In this case, the person may be alive, but tests will show the opposite, since physiological processes literally freeze from the cold
Body temperature must be measured. If the temperature is below 32.2°C, it may distort the picture and show a false death. In this case, the person may be alive, but tests will show the opposite, since physiological processes literally freeze from the cold.
A blood test is prescribed that will help determine whether the metabolism is disturbed, whether there is hormonal dysfunction, and at what level the glucose levels are.
To correctly diagnose brain death, inpatients resort to instrumental research:
- encephalogram (EEG);
- contrast study of cerebral vessels;
- test with irritation of the eardrums (ice water is dripped onto them through the ear canal);
- apneic oxygenation test.
Oxygen starvation is extremely destructive for neurons, even if it is not long-term. Literally after a few minutes of complete lack of oxygen supply, tissues begin to die. The electroencephalogram in this case will show a zero line. This means that there is no brain activity at all.
Encephalography examines brain activity. In this case, the device registers biocurrents, their work is reproduced on paper in the form of curves.
The diagnostic protocol also includes the study of cerebral vessels using a contrast agent. It cannot always be accomplished, as there may be financial restrictions, and sometimes there is simply no equipment. The essence of the test is that a contrast agent is injected, which enters the brain vessels through the bloodstream and identifies possible areas of necrosis. If the brain is dead, the substance does not enter its vessels. This is one hundred percent confirmation of death.
Apneic oxygenation involves temporarily removing the patient from a ventilator. The goal is to observe whether spontaneous respiratory movements have appeared. The monitor monitors the level of carbon dioxide in the blood. It is carbon dioxide that stimulates the body to produce breathing movements. If after 8-10 minutes breathing does not appear, and the level of CO2 in the blood jumps by 20 mm Hg. Art. higher than the original, we can definitely talk about death.
Signs
Criteria for brain death:
- Persistent lack of consciousness;
- Lack of response to addressing the patient, tactile sensitivity, stroking, pinching the skin;
- Lack of eye movement;
- Cardiac arrest, straight line on ECG;
Brain death is not immediately diagnosed. If all of the above signs are present, the patient is observed in a hospital setting for an average of 12 hours; if during this time the patient does not react in any way to external stimuli and has no reflexes of the brain stem structures, biological death is declared. If the cause of the disease is suspected of poisoning, the patient is observed for 24 hours. If death occurs as a result of a traumatic brain injury, the patient can be observed for less time, only 6 hours; this decision is made by the neurosurgeon who provided assistance from the onset of the disease.
Possible reasons
Brain death can occur for various reasons, but the pathophysiological processes are approximately the same. Brain death occurs due to persistent circulatory disorders, oxygen starvation, and stagnation of metabolic products. Diseases that lead to organ death can be varied: trauma, inflammatory diseases, heart disease, multiple organ failure and many others.
After cardiac arrest, the brain does not die immediately . This depends on many criteria: the general condition of the patient, concomitant diseases, the age of the patient, the disease that caused this condition, the ambient temperature. Irreversible tissue necrosis begins after 3 minutes, but in young healthy people this process is slower. At low air temperatures, the brain dies more slowly. If after 3 minutes or more the patient responds to resuscitation measures and returns to life, no one can predict the consequences; perhaps some neurons have died, and this will significantly affect the patient’s life in the future.