What is hydrocephalus?
The term hydrocephalus is formed from two Greek words: “hydro” - water and “cephalus” - head (“dropsy of the brain”). In hydrocephalus, there is a significant buildup of cerebrospinal fluid (CSF) inside cavities of the brain called ventricles. An increase in the volume of cerebrospinal fluid (CSF) occurs when the balance between the production of cerebrospinal fluid and its absorption and further removal from the body is disturbed. This may be the result of a deficiency in the circulatory system or excessive production of cerebrospinal fluid. Hydrocephalus can be congenital or acquired. The concept of congenital hydrocephalus means that it appears from the moment of birth. The disease can be provoked by various factors: traumatic brain injury, brain tumor, necrosis, meningitis, etc. The frequency of this disease is high throughout the world. According to the literature, hydrocephalus affects 5-15 children out of every thousand newborns. Treatment consists of diverting CSF outside the cerebrospinal fluid system into body cavities where it can be absorbed (absorbed). An effective operation allows a child to live and develop normally, study in a regular school, and an adult to return to a full, active life. However, patients and their loved ones must be able to recognize the signs and symptoms of postoperative complications so that medical care can be provided in a timely manner.
Hydrocephalus
The essence of hydrocephalus is an increase in the volume of cerebrospinal fluid, and, as a rule, an increase in intracranial pressure, due to an imbalance between the production and absorption of cerebrospinal fluid.
Hydrocephalus can be either congenital or acquired. Acquired hydrocephalus occurs due to tumor obstruction of the cerebrospinal fluid pathways, trauma, intracranial hemorrhage, or infectious lesions of the meninges.
Pathophysiology – hydrocephalus develops for the following reasons:
- Excessive production of cerebrospinal fluid (CSF) (due to papilloma, choroid plexus carcinoma)
- Impaired fluid circulation - it occurs due to obstruction (blockage) of the circulation pathways of fluid produced in the ventricles of the brain. Typically, this situation occurs when tumor occlusion of the natural openings connecting the ventricles of the brain with each other and with the subarachnoid space.
- Impaired absorption (absorption) of cerebrospinal fluid. Often, impaired absorption occurs due to blockage of the pachyonic granulations located along the superior sagittal sinus (parasagittal).
In different age groups, hydrocephalus clinically manifests itself differently.
Acute hydrocephalus is clinically manifested by severe headache, gait disturbance, nausea, and visual disturbances. In children, early signs of hydrocephalus may include irritability and an inability to hold the head up. When the third ventricle expands, the patient develops Parinaud's syndrome (upward gaze paresis - inability to raise the eyes upward) or the setting sun symptom (Parinaud's syndrome with retraction of the eyelids and forced downward rotation of the gaze). Rarely, there may be a focal symptom in the form of abducens nerve paresis. In children, the fontanel bulges, the veins of the scalp expand, and the head circumference progressively increases. As the pathology progresses, symptoms of brain stem damage, coma, and hemodynamic disturbances occur.
With normal pressure hydrocephalus (hydrocephalus with normal intracranial pressure), the symptoms are quite clear. It usually develops in elderly patients.
Indications
For symptomatic hydrocephalus, the underlying disease must be treated.
Contraindications
Hydrocephalus does not always need to be treated.
- Ventriculomegaly in the elderly who do not have a triad of clinical symptoms
- Hydrocephalus en vacuo, when brain tissue is replaced by cerebrospinal fluid. Since there is no imbalance between the production and absorption of cerebrospinal fluid, the condition is not technically hydrocephalus.
- Arrested hydrocephalus – which is characterized by the fact that the neurological condition of the patient is stable with stable ventriculomegaly. The diagnosis must be made very carefully, as neurological deterioration in children occurs very slowly and is difficult to document.
- Benign hydrocephalus of children occurs in newborns and infants. The children have no neurological symptoms, and their head sizes are normal. A CT scan of the brain reveals moderately dilated cerebral ventricles and subarachnoid fissures.
Research
- CT scan shows the extent of ventriculomegaly and in many cases determines the etiology. With intravenous administration of a contrast agent, tumors and infectious processes leading to obstruction can be detected. This fact helps to plan surgical treatment. The ventricles are dilated proximal to the point of obstruction. With pseudotumor of the brain, no pathological foci are detected on a CT scan of the brain.
- MRI will show congenital causes of hydrocephalus in many, but not all, cases. It shows pathologies such as agenasia of the corpus callosum, Chiari malformation, neuronal migration disorders, and vascular malformations. Some tumors, for example, gliomas of the midbrain plate, can only be identified with this study. T2-weighted studies may show transependymal fluid flow.
- Fetal and neonatal ultrasound is a good method for monitoring ventricular size and intraventricular hemorrhage.
Diagnostic procedures
Lumbar puncture is used to measure intracranial pressure. But it must be performed after an MRI or CT scan of the brain.
Drug treatment
Has a temporary effect. In transient cases such as sinus occlusion, meningitis, neonatal ventricular hemorrhage, drug treatment may be effective. The following drugs are used.
- Acetazolamide (25 mg/kg/d x 3). Respiratory status and electrolyte balance must be monitored. Treatment is not recommended to continue for more than 6 months.
- Furosemide (1 mg/kg/d x 3) – monitoring of electrolyte and fluid balance is necessary.
- Lumbar puncture - in newborns it is used for intraventricular hemorrhage, in some cases it can lead to cure.
- In many cases, the solution to the problem is to remove the cause of hydrocephalus.
Preoperative details
- Before performing invasive procedures, it is necessary to clarify the cause of hydrocephalus. If possible, hydrocephalus should be treated conservatively (with medication).
- Patients with suspected infection or with elevated protein levels in the cerebrospinal fluid (more than 150 mg/dL) should not undergo surgery.
- It is necessary to preoperatively assess the nature of hydrocephalus (level of intracranial pressure) to select the appropriate valve pressure for shunt operations. The most optimal is the use of programmable shunts.
- Antibiotic prophylaxis is mandatory before surgery.
Surgery
- Endoscopic ventriculostomy of the third ventricle (ventriculostomy) - this procedure is used in patients with normal or almost normal ability to absorb cerebrospinal fluid. Surgery is performed using endoscopic technology. High precision of the operation is ensured by the use of frameless steriotaxic equipment.
- Ventriculoperitoneal shunt is the most commonly performed operation for hydrocephalus. After preoperative assessment of intracranial pressure, an appropriate pressure valve is selected. The most optimal is the use of programmable shunts, which allows, if necessary, to change the valve pressure without repeated surgical intervention .
- If there are certain problems in the absorption of fluid in the abdominal cavity (previous peritonitis, adhesive disease), ventriculoatrial (the distal end of the catheter is installed into the appendage of the heart through the jugular vein) and ventriculopleural (the distal end of the shunt is installed into the pleural cavity) shunting can be performed.
- Torkildsen shunt - using a catheter without a valve, the ventricular cavity is connected to the occipital cistern of the brain.
- Lumboperitoneal shunting is used for connecting hydrocephalus (non-occlusive), especially if the ventricles of the brain are narrow. The classical indication for this type of shunting is cerebral pseudotumor.
Postoperative management of patients
- After shunt surgery, it is advisable to activate patients and bring them to an upright position slowly, to avoid the occurrence of a subdural hematoma.
- An X-ray of the skull is performed to assess the correct location of the ventricular catheter.
- It is necessary to monitor the healing of the wound; sutures are removed 10–14 days after surgery
- A CT scan of the brain is performed 2-3 weeks after surgery.
Complications
- Infectious complications are most likely during the first 6 months after surgery.
- Postoperative subdural hematomas are rare. This complication can be avoided by slowly mobilizing the patient.
- Impaired absorption in the abdominal cavity.
- Excessive drainage - most often occurs with lumboperioneal shunting, manifested by headache in an upright position. More often than not, this problem resolves on its own. Otherwise, the operation is repeated and the valve is changed to a higher pressure (or, with a programmable shunt, the valve is reprogrammed non-surgically)
results
The results depend on many factors - the nature of the underlying pathology, the duration of hydrocephalus, and the initial condition of the patient.
With timely and correctly performed surgery, the results are generally good.
Anatomy and physiology
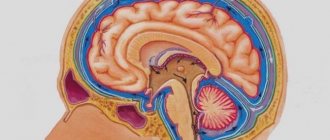
In order to better know and understand the disease, we will give you some information about the anatomy of the skull, the structure of the brain, as well as the process of formation and absorption of cerebrospinal fluid (Fig. 1). The brain occupies most of the cranial cavity. It is penetrated by a large number of blood vessels and is surrounded by cerebrospinal fluid as a buffer. The fluid is located in 4 cavities (ventricles) located inside the brain. The ventricles have delicate structures known as villous plexuses (choroid plexuses). These structures produce a significant amount of CSF - about 500 ml per day. The fluid circulates continuously and contains a large number of substances essential for nutrition and ensuring the normal functioning of the nervous system.
CSF also provides a protective cushion for the brain. CSF circulates in the ventricular system and is removed through 3 holes in the 4th ventricle and then enters the subarachnoid space surrounding the brain and spinal cord.
CSF constantly circulates in the brain and spinal cord, constantly being in the process of a) formation, b) circulation and c) absorption. In a healthy body these processes are balanced. Hydrocephalus develops if CSF is not cleared from the ventricular system through the cerebrospinal fluid tract. Less commonly, hydrocephalus is caused by excess production of CSF, such as with villous plexus papilloma.
What it is
The Greek word “hydrocephalus” is used by specialists along with the Russian term “dropsy of the brain.” If translated literally from ancient Greek. ὕδωρ “water” + κεφαλή “head”, so it turns out – “water in the head”.
However, we are not talking about water, but about cerebrospinal fluid (CSF), which accumulates in the ventricles of the brain and/or in the space between the membranes of the brain. Liquor is produced in the ventricles, then circulates inside the skull, then moves into the circulatory system through special veins. This is a kind of “safety cushion”. It protects the brain and spinal cord from external mechanical influences, that is, it softens blows and other sharp impacts. It also removes harmful substances from the brain and delivers useful ones, that is, it supports metabolic processes between the blood and the brain.
Usually there is very little cerebrospinal fluid, in infants - only 50 ml. But if suddenly the production of cerebrospinal fluid becomes excessive or the outflow becomes difficult, an excess of it appears and intracranial pressure increases. This syndrome is called hydrocephalus.
Excess cerebrospinal fluid puts pressure on the brain - and this can lead to severe neurological disorders, decreased vision, weakness in the upper and lower extremities, decreased intellectual abilities, and most importantly, death.
Diagnostics
In newborn children, the bones of the skull have not yet fused and hydrocephalus is determined visually. The head enlarges, the bones of the skull diverge, the fontanelle is tense and bulging; the skin is thin and shiny; The veins in the hairline area look full and swollen. Also symptoms are: vomiting, apathy, excitability, downward displacement of the eyes (“setting sun symptom”), etc. However, when the cranial sutures are not fused, the signs and symptoms of increased intracranial pressure seem subtle.
In older children and adults, the bones of the skull are fused and, when the ventricles expand, compression of the brain tissue occurs. Symptoms of increased intracranial pressure appear: headaches, nausea, vomiting, blurred vision, lack of coordination, psychopathological personality changes, lack of concentration and lethargy. These symptoms require additional instrumental diagnosis.
Diagnosis of dropsy of the brain
In infancy, a visual examination is sometimes sufficient to determine the nature of the pathology: the doctor, by examining the baby’s physiological parameters and listening to the parents’ complaints, can make a preliminary diagnosis at the initial appointment.
To clarify the disease in children with an open fontanel, including to identify pathology during intrauterine development, ultrasound is used to assess the degree of enlargement of the ventricles. Additional methods are:
- fluoroscopy;
- computed and magnetic resonance imaging;
- lumbar puncture, necessary for a detailed analysis of the cerebrospinal fluid.
A child with suspected hydrocephalus must be examined by an ophthalmologist or pediatrician; if necessary, concomitant diseases may require consultation with a cardiologist, surgeon, oncologist and other specialists.
Types of diagnostic tests
- Ultrasound is a simple, inexpensive test that helps evaluate the extent to which the ventricles of the brain are dilated. Currently, it is the simplest and safest method for diagnosing hydrocephalus.
- Computed tomography (CT) - This is a technique of drawing with a thin beam the contours of the skull, brain, ventricles and subarachnoid space. It is carried out to determine the size and shape of the ventricles and identify abnormalities such as tumors, cysts or other pathologies.
- Magnetic resonance (nuclear magnetic resonance NMR) is a non-surgical diagnostic method that uses radio signals and a magnet. MRI data determines the shape and severity of hydrocephalus. These studies are indispensable for clarifying the causes of dropsy.
- Cisternography (radiography of the cisterns at the base of the skull) is a test that requires the injection of a radioactive substance into the CSF. It is used to clarify the type of hydrocephalus: communicating or obstructive, as well as to determine the direction of CSF flow.
- Pneumoencephalography is now used much less frequently than in the past. In some cases, it is necessary to pump air with a needle into the spinal cord.
- Angiography (X-ray of blood vessels) is a special technique for injecting a contrast agent into the arteries that cross the brain. After some time, anomalies are detected at the level of blood vessels and the presence or absence of pathological disorders.
- A neuropsychological examination consists of a series of questions and answers to identify the presence of abnormalities in the functioning of the brain.
Treatment
Currently, occlusive (obstructive) hydrocephalus is treated surgically. Surgical intervention consists of draining excess cerebrospinal fluid outside the cerebrospinal fluid system: into the abdominal (abdominal) cavity or into the atrium. Sometimes CSF may be drained into the pleural cavity. In these cavities, cerebrospinal fluid is absorbed and excreted along with waste products of the body.
To drain the CSF, the surgeon implants a drainage system (shunt). The system material is silicone and polypropylene. Both of these materials are well tolerated by the body. All elements of the system are implanted under the skin; there are no external areas.
Shunting for hydrocephalus in adults
Bypass surgery is performed on patients of any age. Most often, hydrocephalus, for which surgery is indicated, occurs in children and the elderly. There are the following reasons for the accumulation of excess cerebrospinal fluid in the brain:
- increased production of cerebrospinal fluid in the brain;
- impaired absorption of cerebrospinal fluid in the cerebral vessels;
- disruption of cerebrospinal fluid transport in the brain.
Most often, hydrocephalus develops due to impaired circulation of cerebrospinal fluid. This is caused by cysts, inflammatory processes and brain tumors. Brain shunting for hydrocephalus is performed by neurosurgeons. A shunt for hydrocephalus is a hollow tube through which excess cerebrospinal fluid is drained into one of the cavities of the body, where it is absorbed. For hydrocephalus, various types of shunts are used, each of which has its own advantages and disadvantages. Brain shunting for hydrocephalus in children and adults can improve the quality of life of patients.
The shunt system consists of three parts. The inner part is a thin flexible silicone tube (catheter). It is implanted directly into the ventricle of the brain, in which excess cerebrospinal fluid accumulates. The catheter opens into a storage reservoir. A special valve is installed at the junction of the reservoir and the catheter, which regulates the volume of drained cerebrospinal fluid. Cerebrospinal fluid collects in a reservoir and is drained into the chest or abdomen through the external part of the shunt.
The outer section of the shunt is the part that connects the internal catheter with the cavity into which drainage is performed. Neurosurgeons place this section of the shunt under the skin of the neck. It is not visible to prying eyes.
For hydrocephalus in adults, neurosurgeons use the following types of shunts:
- ventriculoperitoneal - open into the abdominal cavity;
- ventriculopleural - drain cerebrospinal fluid into the pleural cavity;
- ventriculoatrial - open into the atrium.
In the absence of an alternative method, drainage is performed into the gallbladder or bladder.
An important component of the bypass system is the valve. It ensures the movement of cerebrospinal fluid in one direction (from the ventricle of the brain to the outside) and prevents the reverse flow of cerebrospinal fluid. The valve regulates the volume of cerebrospinal fluid entering the reservoir.
Fixed shunts have valves with three preset modes: low, medium or high intensity. Programmable bypass systems have more advanced valves that allow the volume of outflow to be adjusted as needed. The correction is made by a doctor. It uses an external magnetic device for this purpose. Brain shunting for hydrocephalus in children is carried out using a fixed shunt, and then it is replaced with a programmable shunt.
Shunt System Components
The system consists of two catheters and one one-way valve. The ventricular catheter is located in the ventricle of the brain, and the peripheral (peritoneal or cardiac) catheter is placed in the abdominal cavity or in the right atrium, respectively. Both catheters are connected to a valve that regulates the unidirectional flow of cerebrospinal fluid. The valves are designed to operate in different pressure ranges (high, medium, low and very low). The neurosurgeon, having determined the patient’s intracranial pressure, selects the appropriate valve, depending on the severity of the disease, the patient’s age and clinical nuances.
Almost all valve models have a reservoir that your doctor can use to “bleed” the system to determine if it is working properly. From the reservoir, by inserting a thin needle through the skin, you can take samples of cerebrospinal fluid for laboratory tests or administer medications. Patients and their loved ones are not recommended to test the drainage system by “bleeding” the reservoir. This action can be dangerous unless your doctor has given you specific instructions about it. In patients suffering from non-communicating (obstructive) hydrocephalus, cerebrospinal fluid should be drained from the cerebral ventricle using a ventricular catheter. In patients with communicating hydrocephalus, a CSF drainage system is implanted from the lumbar space of the spine into the abdominal cavity - the lumboperitoneal system.
Treatment methods
Timely – early – intervention makes hydrocephalus not as fatal as before. Modern treatment methods save 95% of patients with a similar diagnosis. Surgery is virtually the only method of combating the disease. Drug methods in most cases can only slow down the course of the disease, but do not eliminate the root cause.
Modern techniques have many options for surgical treatment of hydrocephalus. In order to remove excess fluid from the cranial cavity, shunting is usually used. It consists of installing a shunt, which can be compared to a pipeline. It pumps out excess cerebrospinal fluid and pumps it into other cavities of the body - into the abdominal cavity, into the atrium.
Silicone valve systems are used as a shunt, which help regulate the pressure of cerebrospinal fluid in the cavities of the brain. The drainage system (shunt) and the level of pressure in it (in the case of programmable shunts) are selected by a neurosurgeon depending on the form of hydrocephalus and the age of the child. Bypass surgery is free and is included in the compulsory medical insurance list.
Endoscopic operations are also used as surgical treatment. The purpose of the endoscopic operation is to create an anastomosis (connection) between the cavity of the third ventricle and the basal cisterns (the second largest cavity of the brain, which is a reservoir for cerebrospinal fluid), located at the base of the skull. This operation is appropriate for outflow disorders in the posterior cranial fossa.
Endoscopic operations are also widely used when it is necessary to remove any obstacle to the movement of cerebrospinal fluid, for example, to remove a cyst. Without exception, all operations are aimed at restoring the balance between the production and absorption (discharge) of cerebrospinal fluid.
Surgery and hospitalization
Implantation of the shunt system is carried out by a neurosurgeon under sterile operating room conditions. In preparation for surgery, the hair is shaved to achieve maximum cleanliness. The operation is performed under general anesthesia, usually not for a very long time. The neurosurgeon drills a small hole in the skull bone, then makes a small incision in the dura mater that protects the brain and inserts a ventricular catheter into the lateral ventricle. To implant the rest of the bypass system, another incision is made and a tunnel is created subcutaneously to implant a peritoneal or cardiac catheter. The end of the catheter is carefully inserted either into the abdominal cavity or into the jugular vein leading to the ventricle of the heart. Catheters are connected to the valve using connectors on the valve itself. All parts of the shunt are thus connected into a single drainage system. At the end of the operation, small sterile dressings are applied to each incision.
Immediately after the operation, the patient is taken to the postoperative department. The patient is here from 1 hour to 1 day under close observation, then he is transferred to the ward. Most patients are discharged 7-10 days after clinical rehabilitation.
Treatment of hydrocephalus in children
Treatment of hydrocephalus in children
HYDROCEPHALUS IS THE MOST COMMON CAUSE OF SURGICAL INTERVENTIONS ON THE CENTRAL NERVOUS SYSTEM ORGANS IN CHILDREN
Hydrocephalus
, hydrocele - a disease characterized by excessive accumulation of cerebrospinal fluid in the ventricular system of the brain as a result of difficulty in moving it from the place of formation (cerebral ventricles) to the place of absorption into the circulatory system (subarachnoid space) -
occlusive hydrocephalus
, or as a result of malabsorption -
aresorptive hydrocephalus
.
The frequency of occurrence is 1 case in 2000-4000 newborns, more common in boys.
Causes of occurrence.
Hydrocephalus occurs at any age, but most often in young children, due to various reasons: tumors, infectious and inflammatory diseases, traumatic brain injury, congenital anomalies.
Hydrocephalus in a newborn can be caused by a birth craniocerebral injury, infectious diseases suffered by the mother during pregnancy (cytomegalovirus infection), leading to disruption of the ventricular system of the fetal brain. This, in turn, leads to difficulty in the circulation of cerebrospinal fluid and/or its excessive formation. In addition to congenital hydrocephalus, acquired hydrocephalus can also develop (most often in the first months of a newborn’s life) after meningitis, meningoencephalitis, head injuries, intoxication, intraventricular hemorrhages, etc.
Impaired circulation of cerebrospinal fluid (CSF) leads to increased pressure in the cranial cavity and the occurrence of the so-called hypertensive-hydrocephalic syndrome. As a result of the pressure exerted on areas of the brain, vision begins to decrease, convulsions occur, compression of the brain stem is manifested by oculomotor disorders (strabismus, limited upward gaze (the “setting sun” symptom)), weakness in the upper and lower extremities. This can lead to death, severe neurological disorders, and decreased intellectual abilities.
Manifestations
. The most characteristic sign of hydrocephalus in newborns is an accelerated growth of head circumference, leading to a visually well-defined hydrocephalic shape of the skull, greatly increased in volume. Signs of hydrocephalus include a bulging, tense fontanelle, frequent tilting of the head, and a downward displacement of the eyeballs. In places where normal fusion of the skull bones has not occurred, rounded pulsating protrusions may form. Strabismus and nystagmus (involuntary eye movements with high frequency) often occur. There is high excitability due to headaches, the child does not eat well, often cries, vomits, and is lethargic. Sometimes you may notice a decrease in vision and hearing.
Hydrocephalus in older age is characterized by headaches, especially in the morning, nausea and vomiting at the height of headache, dizziness; the size of the head is not increased.
These graphs reflect normal head circumference depending on the age of the child in boys and girls.
Diagnostics.
The most informative are magnetic resonance and computed tomography, which reveal sharply enlarged ventricles of the brain. In young children with an open large fontanelle, neurosonography (ultrasound examination of the brain) is also very informative.
Normal ventricles of the brain.
CT picture of hydrocephalus (dilatation of the lateral ventricles).
IT IS IMPORTANT TO UNDERSTAND THAT THERE IS NO EFFECTIVE DRUG FOR TREATING HYDROCEPHALUS.
MEDICATION TREATMENT OF HYDROCEPHALUS IS MAINLY APPLIED IN THE FORM OF TEMPORARY MEASURES, ESPECIALLY IN CASES WHEN THE DECISION ABOUT SURGICAL TREATMENT HAS NOT BEEN MADE AND MAY BE DELAYED.
ANNUALLY, AT THE NEUROSURGICAL DEPARTMENT OF THE ROSTOV REGIONAL CHILDREN'S CLINICAL HOSPITAL, ABOUT 150 OPERATIONS FOR SURGICAL TREATMENT OF HYDROCEPHALUS ARE CARRIED OUT FOR CHILDREN IN THE ROSTOV REGION AND IN NEIGHBORING REGIONS OF THE SOUTH RUSSIA
Surgical treatment of hydrocephalus in children.
The main method of treating hydrocephalus is endoscopic ventriculostomy of the third ventricle, which consists in creating a connection between the third ventricle and the interpeduncular cistern by dissecting the bottom of the cistern. If endoscopic triventriculostomy is ineffective, a cerebrospinal fluid shunt operation is used - this is a surgical intervention during which a special shunt is installed that drains fluid from the cerebrospinal fluid spaces of the brain into the circulatory system. As a result of the installation of a shunt, fluid does not accumulate in the cranial cavity, and hydrocephalus no longer develops, and a person’s life completely depends on the functioning of this device (shunt).
The entire range of operations performed to treat this pathology is divided into two groups:
1. Operations with drainage of cerebrospinal fluid outside the central nervous system:
-Installation of a ventriculoperitoneal shunt (shunt between the brain and peritoneum);
-Installation of a ventriculoatrial shunt (between the brain and heart);
-Installation of a ventriculovenous shunt (between the brain and veins).
1. “Internal shunting” with the creation of normal channels for the movement of cerebrospinal fluid through the central nervous system systems:
-Torkildsen operation (ventriculocisternostomy). It consists of creating a communication between the lateral ventricle and the occipital cistern by installing a silicone catheter passed under the skin on the back of the head;
-Endoscopic ventriculostomy of the third ventricle. It consists of creating a communication between the third ventricle and the interpeduncular cistern by dissecting the bottom of the cistern in the area of the gray tubercle;
-Implantation of internal stents. It consists of installing stents that expand the Magendie and Luschka holes to normal;
-Plasty of the cerebral aqueduct. It consists of expanding the lumen of the water supply system to ensure normal circulation of cerebrospinal fluid;
-Fenestration of the interventricular septum. It consists of creating an opening between the ventricles through which cerebrospinal fluid can circulate freely.
At the moment, in modern pediatric neurosurgery, only 3 methods of surgical treatment of hydrocephalus are widely used and recognized:
Endoscopic triventriculostomy.
The essence of the method is to create, using a neuroendoscope, a hole in the bottom of the third ventricle for the outflow of fluid into the extracerebral cisterns. As a result, the cerebrospinal fluid flows freely and the person is cured, without shunt dependence. The neuroendoscope is a complex optical system of Hopkins lenses, an illumination channel, a video channel, as well as channels for inlet and outlet of fluid, built into a tube with a diameter of only 6 mm. The operation is performed through a small hole in the skull. The image from the endoscope camera is transmitted to the screen and the doctor sees where the instrument needs to be inserted to restore the outflow of fluid. The method is less traumatic and reliable. Unlike bypass surgery, which takes about an hour, the operation takes only 10-20 minutes.
TO CARRY OUT TRIVENTRICULOSTOMY, THE NEUROSURGICAL OPERATING ROOM OF THE CSTO ROOM IS EQUIPPED WITH MODERN ENDOSCOPIC EQUIPMENT FROM THE LEADING MANUFACTURER
KARL STORZ.
This is what the perforated bottom of the 3rd ventricle looks like.
Endoscopic ventriculostomy of the third ventricle is an effective method for the treatment of obstructive triventricular hydrocephalus; with the correct choice of indications, it allows achieving a lasting cure in 90% of such patients and, therefore, is the preferred method. The risk of serious complications after endoscopic ventriculostomy of the third ventricle is low and amounts to 6.6%. The key to the safety of the operation is: its planning on the basis of complete and high-quality clinical and radiological data and strict adherence to the methodological standard of the operation at all its stages, which together makes it possible to reduce the risk of serious complications by three times. The peculiarity of this surgical intervention is that it is highly effective only for obstructive forms of hydrocephalus.
Ventriculoperitoneal and ventriculoatrial shunting.
Ventriculoperitoneal shunt surgery has been in practice for more than fifty years, being the main standard method for getting rid of almost any form of hydrocephalus. Regardless of the technical nuances of the operation, the final result of VPS is the creation of an artificial outflow of cerebrospinal fluid from the dilated ventricles into the abdominal cavity. In some cases, in order to reduce the risk of trauma to the abdominal organs, in the presence of adhesions after previous abdominal operations, it is possible to use laparoscopic techniques. The shunt system consists of 3 main elements:
— ventricular catheter
, which is installed into the ventricular system through a small burr hole at one of the standard points;
— shunt pumps
regulating the outflow of cerebrospinal fluid from the ventricles; All models of pumps equipped with valves can be divided into three types depending on their throughput, or, in other words, on the level of cerebrospinal fluid pressure (low, medium and high pressure). Shunt systems with valves of a given pressure pose a certain complexity for the surgeon, since an error in selecting the parameters of a shunt system can lead to both excessive and insufficient levels of cerebrospinal fluid drainage; this problem can be solved by shunt systems that have appeared not so long ago, equipped with programmable valves, the “highlight” of a programmable valve is that it is equipped with a device designed for the possibility of remotely changing the level of cerebrospinal fluid drainage;
— peritoneal or atrial catheter
, immersed in the abdominal cavity or atrium to ensure the outflow of cerebrospinal fluid.
This is what a shunt system looks like, consisting of a ventricular catheter, a shunt pump and a peritoneal/atrial catheter
ü IN THE NEUROSURGICAL DEPARTMENT OF GBU RO "CSCH", FOR SURGICAL CORRECTION OF HYDROCEPHALUS ONLY MODERN SHUNT SYSTEMS FROM LEADING FOREIGN MANUFACTURERS, SUCH AS
INTEGRA, AESCULAP, ETC.
Complications.
The key point in the development of complications after liquor shunt operations using shunt systems is the presence of a foreign shunt system in the child’s body. According to various authors, in children in the first year of life, the risk of developing dysfunction of the shunt system (that is, its failure), even with a favorable course, is up to 50% and subsequently decreases by 10% with each subsequent year of the child’s life. The essence of the dysfunction is the impossibility of ensuring the shunt system of normal outflow of cerebrospinal fluid for one reason or another, due to the failure of the main elements of the shunt system, in addition to purely technical issues associated with the breakdown of the valve apparatus of the pump, frequent causes of shunt dysfunction are the development of shunt infection, the formation of pseudoperitoneal cysts in the abdominal cavity (a limited cavity that does not allow cerebrospinal fluid to be normally absorbed into the peritoneum). Clinically, the development of dysfunction is manifested by the development of general cerebral (the child becomes lethargic, adynamic, refuses to eat, nausea, vomiting appears) and focal neurological symptoms (Graefe’s “setting sun” symptom, meningeal symptoms, etc.).
It is important to remember that dysfunction of the shunt system is a serious complication in which repeated surgical intervention is indicated to eliminate it; If there is a suspicion of dysfunction of the shunt system, it is necessary to urgently seek specialized neurosurgical help to examine the child and decide on further treatment tactics!!!
ü Neurosurgical Department of the State Budgetary Institution of the RO “CSTO” operates around the clock and has the ability to conduct emergency surgery for hydrocephalus, including in cases of the development of displacement of shunting systems
Unfortunately, even a successfully performed operation is not a guarantee of hydrocephalus cured for life, since the anatomical dimensions of organs can change, the head can grow (especially in children), the holes in the shunt systems become clogged, etc. Children who have undergone such operations need to be constantly monitored by a neurologist and neurosurgeon in order to promptly identify emerging disorders that require correction. Thus, due to changes in the position of organs or the growth of the head, repeated operations have to be performed to replace the shunt with a more suitable one in terms of parameters.
Participation in care
Children with implanted shunts should be monitored by a neurosurgeon throughout their lives. Most patients suffering from hydrocephalus, after implantation of a shunt system, can lead a normal life, but constant monitoring by loved ones in collaboration with a neurosurgeon is necessary.
The neurosurgeon monitors each patient to prevent drainage failure. The first time after implantation or re-operation - regularly, with a gradual transition to examinations once a year.
Relatives are advised to be able to recognize early signs of complications. Quick and accurate assessment of health problems is very important. Flu symptoms may mask symptoms of a blocked shunt. Quickly identifying them will allow you to plan a repeat operation and avoid an emergency.
Patients and their loved ones should pay close attention to signs and symptoms of complications. The main causes are: blockage, infection and excessive drainage.
Blockage
The main type of complication is blockage of the system. Blockages can occur at any level of drainage. The holes in the ventricular catheter may become clogged with brain tissue or villous plexus tissue. It can also be blocked due to excessive contraction of the ventricular cavity due to too intense drainage of fluid from the ventricular cavity (constricted ventricle syndrome). Intestinal loops or necrotic tissue may adhere to the peritoneal catheter. Shunts inserted into a ventricle of the heart can become blocked by blood clots, pieces of brain matter, or tumor cells.
The shunt system may also be disconnected by disconnection of various elements of the shunt or by changes in the position of the catheter caused by the growth of the child. X-rays are necessary to check the integrity of the shunt.
Partial blockage of the system parts provokes the appearance of symptoms of increased intracranial pressure. Episodic headaches, nausea, apathy and decreased sensory functions may occur. Decreased performance at school or at work is the most common phenomenon in these conditions.
In case of complete blockage, symptoms develop more quickly (headaches, nausea, vomiting, blurred vision, loss of coordination and confusion). The patient falls into a stupor or coma. In such cases, urgent hospitalization is necessary for observation and appropriate treatment.
The surgeon performs a series of tests to locate and determine the extent of drainage blockage. Sometimes it is necessary to remove and replace part or all of the system.
results
Of the 59 patients, premature synostosis of the cranial sutures was detected in 27 (46%) cases (Table 1). The most frequently observed combined synostosis of the sagittal and both coronal sutures (41%). In second place in frequency is isolated fusion of the sagittal suture (37%). The following are in descending order: bicoronal synostosis (11%), pancraniosynostosis (7%) and unilateral coronary synostosis (4%). Isolated lesions of the lambdoid sutures were not detected in any case (Table 2).
Table 1. Characteristics of patients with secondary craniosynostosis Table 2. Types of affected cranial sutures
In 12 (44%) cases, hydrocephalus was congenital, in 6 (22%) - post-inflammatory, in 3 (11%) - post-hemorrhagic, in 3 (11%) cases there was a combination of intraventricular hemorrhage and ventriculitis. In 1 child, hydrocephalus was associated with a tumor; in 2 cases, the etiology of hydrocephalus remained unclear. In the majority of children (52%), a medium-pressure valve was implanted during the initial operation, both with and without the installation of an anti-siphon device. Identified by 1 valve for low and high pressure. In the remaining 11 children, the parameters of the shunt system could not be determined due to the lack of indications of the type of valve in the discharge documents about the primary operation and in the protocols for revision interventions (Fig. 1).
Rice. 1. Distribution of patients according to the type of valve of the shunt system installed during the primary intervention.
24 patients with dysfunction of the shunt system underwent interventions with replacement of the entire shunt or its individual components, after which an improvement in their condition was noted. One of them, in the presence of secondary craniosynostosis and slit-like ventricles, but intact subarachnoid spaces, was diagnosed with clear signs of dysfunction of the distal catheter of the shunt system. After revision of the shunt, an improvement in the child's condition was achieved. In 3 (11%) cases, taking into account the presence of clinical symptoms of increased ICP and radiological signs of craniocerebral disproportion (CCD), a decision was made to perform reconstructive surgery. Two patients underwent biparietal craniotomy, one patient underwent frontoparietoccipital reconstruction. In this case, two of them simultaneously replaced the valve with a programmable one. No complications were noted after reconstructive interventions. The patients were discharged with improvement in satisfactory condition.
Clinical example No. 1
Patient A
., 7 years. At the age of 3 months, a shunt was installed due to hydrocephalus that developed after tumor removal. She was admitted with manifestations of slit ventricle syndrome. After our operation, his condition improved. She was discharged on the 9th day in satisfactory condition. Duration of observation: 11 months. There has been an improvement in development, she has learned to read and walks with support. The headache does not bother me (Fig. 2).
Rice. 2. Clinical example 1. a, b—severe deformation of the skull against the background of synostosis of the sagittal and both coronal sutures; c, d — frontoparieto-occipital reconstruction was performed with replacement of the valve with a programmable one set to medium pressure.
Clinical example No. 2
Patient B
., 8 years.
At the age of 4 months, the child had a medium-pressure shunt installed due to congenital hydrocephalus (Dandy-Walker anomaly). For 7 years the condition remained stable. 6 months before the present hospitalization, an intense headache appeared, which was accompanied by nausea and vomiting. The frequency and severity of pain progressed over 2 months, significantly limiting the child's daily activities. During the examination, slit-like lateral ventricles were diagnosed, and therefore the shunt was revised and the valve was replaced with a programmable one. After the operation, the patient's condition improved. However, after 3 months, complaints of headache, nausea, vomiting resumed, and double vision appeared. The patient was re-hospitalized. The neurological status, in addition to general cerebral symptoms, revealed convergent strabismus due to paresis of the right abducens nerve. Based on the results of the examination and a thorough analysis of CT data, including three-dimensional reconstruction of images, sagittal craniostenosis with narrowing of the convexital subarachnoid spaces and slit-like lateral ventricles was diagnosed (Fig. 3, a
, b). Due to the absence of signs of dysfunction of the shunt system and the presence of obvious CD, a decision was made to reconstruct the cranial vault in order to increase its volume. The patient underwent biparietal craniotomy with the formation of two parietal flaps and a bone bridge over the superior sagittal sinus. Clinically, after the operation, an improvement in the child’s condition was noted: the headache and evacuation disorders were relieved, and regression of congestive changes in the fundus was noted. Postoperative CT examination also demonstrates positive dynamics in the form of normalization of the sizes of the ventricles and the appearance of subarachnoid spaces (see Fig. 3, c, d). He was discharged on the 10th day after reconstructive surgery. Currently, the follow-up period is 12 months. The patient's condition remains stable and satisfactory. Repeated interventions were not performed. Headache and nausea are not a concern, oculomotor disorders have regressed. The child attends school.
Rice.
3. Clinical example 2. a — CT reconstruction of the brain reveals synostosis of the sagittal suture; b - slit-like lateral ventricles. Convexital subarachnoid spaces are not visible; c — CT scan after skull reconstruction; d — positive CT dynamics: normalization of the sizes of the ventricles, appearance of subarachnoid spaces. The introduction of cerebrospinal fluid shunt systems into widespread practice has significantly reduced mortality and increased the effectiveness of treatment for patients with hydrocephalus. Among those patients who were implanted with a shunt system at an early age for the treatment of hydrocephalus, there is a subgroup with premature suture fusion, which characterizes secondary CHIC (Fig. 4). As the brain grows, it gradually fills the available internal space of the closed, rigid skull, which marks the transition of the disease to the stage of craniostenosis. These changes subsequently lead to a discrepancy between the volume of the skull and the volume of the rapidly growing brain, resulting in the development of refractory intracranial hypertension. R. Pudenz and E. Foltz [3] suggested that the development of secondary craniosynostosis requires 2-3 years after shunt implantation, J. Weinzweig et al. [4] reported a mean interval of 26 months. At the same time, a number of authors [5–7] describe the development of secondary craniosynostosis in infants just a few months after shunting. In our group there are also patients in whom synostosis of the cranial sutures was noted in the period from 6 to 18 months after shunt implantation.
Rice. 4. Clinical example 3. a — CT scan of a child performed when replacing the shunt system at the age of 10 months; b — during the next intervention at the age of 18 months, CT data revealed fusion of the sagittal suture; c, d — pictures taken with shunt dysfunction at the age of 2 years. Thickening of the bones of the cranial vault is visible; d, f — the catheter was reinstalled in the occipital horn, after which the manifestations of hypertension syndrome regressed. The presence of wide lateral ventricles provides reserve intracranial space, and therefore there are currently no indications for skull reconstruction.
Clinical example No. 3
Child L
. operated on at the age of 3 months for congenital hydrocephalus associated with meningomyelocele. A medium pressure shunt was installed.
Infection
Infection is the second type of complication. It poses a significant risk for any surgical procedure, most often when implanting a foreign body.
It manifests itself in the form of redness or suppuration along the edges of the suture or along the path of the drainage system under the skin. The surgeon fixes his attention on these signs. If left untreated, the wound may erode or open, and in more serious cases, the infection may cause chills and fever. Typically, the drain needs to be removed. Sometimes antibiotic therapy can be administered without removing the system.
Since the shunt is a foreign body, the patient may experience an allergic or inflammatory reaction. Inflammation at one of the drainage sites should be immediately shown to a neurosurgeon.
Excessive drainage
Excessive drainage of cerebrospinal fluid occurs when the valve is incorrectly selected according to the pressure parameter. If the valve opening pressure is too low, it can cause excessive drainage, causing the cerebral ventricle to compress and deforming the brain tissue. The patient experiences headaches that are most severe when standing.
In addition, nausea, vomiting, drowsiness and nervous system disorders, in particular double vision, appear. School-age children experience a decline in mental abilities.
Causes
Hydrocephalus syndrome in children has a fundamental division into congenital and acquired. Among the factors contributing to the occurrence of congenital hydrocephalus are:
- anomalies and malformations of the nervous system that are formed during pregnancy in utero under the influence of various infections and bad habits.
- intracranial birth injury. The risk of developing hydrocephalus increases in premature infants with low birth weight.
Acquired hydrocephalus can develop with: inflammatory diseases of the brain and its membranes (meningitis, encephalitis); tumors of the brain and skull bones; brain injuries received after birth; rupture of arteriovenous malformations of the brain.
More information about shunt systems for the treatment of hydrocephalus
The result of the operation largely depends on the quality of the shunt system. In recent years, in many hospitals, neurosurgeons have been using shunt systems produced by the largest American company Medtronic. The company's engineers, together with leading US neurosurgeons, have developed a range of valves of various models and sizes (including valves for newborns).
One of the latest achievements in the production of liquor drainage devices is the Delta valve. This is a unique valve, has no analogues from other manufacturers. It was created to avoid such a common complication as excessive CSF drainage. If all other valves pass as much fluid as they are designed for pressure, then the Delta valve allows as much fluid as is needed to remain in the ventricle to maintain intracranial pressure within physiological limits. When implanting the Delta valve, the patient is maintained at normal pressure, regardless of the rate of cerebrospinal fluid production and, most importantly, regardless of the patient’s body position (lying/standing).
The technological features of the materials from which the system valves are made prevent deformation and sticking during pumping; the dome of the valve reservoir is designed to withstand repeated punctures with a thin needle (the holes self-tighten). Catheters are made of high-quality latex-free silicone, so they do not stick together or form loops, which significantly reduces the risk of system blockage.
The valves are equipped with connectors for connection to catheters; their design facilitates connection and reduces the possibility of disconnection and disconnection of the system.
A radiopaque mark is applied along the length of the catheters, this allows you to see the shunt on an x-ray. The same substance is applied to the valve with a dot code indicating the pressure of the valve. There are no metal parts in the shunt system. This is very important when conducting CT and NMR studies, because metal will produce artifacts, and a magnet in NMR may shift the location of the system (if it had metal parts).
All systems are sterile and supplied in double sterile packaging. To reduce the risk of infection, Medtronic has developed a unique BioGlide hydrogel. It is applied to the inner and outer surfaces of catheters, as well as the outer surface of the valve, and does not peel off. Before implantation, the neurosurgeon can treat the system parts with antibiotics, and the hydrogel will hold them for 3 days for postoperative antibiotic therapy inside the patient’s body. This way, the risk of infection is minimized.
Discussion
The concept of CHIC is inextricably linked with such pathological conditions as CDV and slit ventricle syndrome (SVS). Understanding the nature of these disorders is key in choosing adequate treatment for this group of patients.
It is necessary to distinguish between simply anatomical reduction in the size of the ventricles, which does not require treatment, with the thyroid gland itself, which has characteristic clinical manifestations. On neuroimaging, narrow or slit-like ventricles are found in 20-53% of children with shunts, while clinically thyroid gland is observed in 1-37% of cases [4, 8-15]. The syndrome develops predominantly in children operated on during the 1st year of life [16]. The average age of manifestation of thyroid gland is 6-7 years [9, 13], although an earlier development of this condition cannot be ruled out [6]. Explaining the causes of the pathology causes a lot of disagreement, and the choice of tactics for thyroid gland remains a subject of debate to this day [1, 17—22]. However, it is quite obvious that all attempts to elucidate the mechanism of development of PTS against the background of CHIC inevitably lead us to the problem of CCD.
CCD refers to a condition where the volume of the growing brain exceeds the available intracranial space. In this case, normal physiological fluctuations in intracranial contents (the volume of intracranial blood and cerebrospinal fluid) lead to an increase in ICP with characteristic clinical manifestations. Various terms are used to describe this pathology in the literature: cephalocranial disproportion [23-26], post-shunt craniosynostosis [4], cranial hyperostosis [27], secondary craniosynostosis [28, 29], shunt-induced craniostenosis [17, 30], secondary microcrania [24] and others.
A. Sandler et al. [31] distinguishes two categories of CDCs:
1) primary CDD - caused by a primary pathological process leading to diffuse thickening of the bones of the arch or premature ossification and closure of the sutures. A striking example of such CCD is primary craniostenosis;
2) secondary CDD is an iatrogenic phenomenon that is initiated by implantation of a shunt system in early childhood.
The incidence of secondary CCD is unknown, since no similar studies have been conducted. Severe, disabling headaches occur in 42% of adolescents with shunts [32]. In a study of 3100 patients undergoing LSO, craniostenosis was detected in 1.6% of patients [1]. In our group of 59 children, 27 (46%) were diagnosed with premature suture closure, while signs of CD were noted in only 3 (5%) of them. It is possible that the approximate incidence of CCD can be indirectly estimated from the incidence of slit ventricle syndrome. It is conceivable that a significant proportion of patients with this syndrome suffer from CCD and their narrow, slit-like ventricles may be a manifestation of a crowded skull.
In CCD, the brain's ability to compensate for physiological fluctuations in intracranial volume is compromised for a number of reasons [33]. First, the discrepancy between normal brain volume and small cranial volume leads to increased extraparenchymal resistance. Secondly, the reduced volume of the ventricles and subarachnoid spaces, which normally participate in compensating for increased ICP, significantly reduces the potential for damping ICP fluctuations [34]. Thirdly, impaired venous outflow during CDD leads to increased pressure in the superior sagittal sinus, which impairs the absorption of cerebrospinal fluid [14]. In addition, venous congestion leads to changes in the turgor of brain tissue, increasing its rigidity and reducing compliance [11, 14].
Clinical manifestations
Typically, such patients are operated on for hydrocephalus at an early age (before 1 year) and, as a rule, they have a history of repeated revisions and multiple visits for chronic severe headaches, despite a functioning shunt. If drug treatment has an effect, it is most often insignificant or short-lived. The severity of the headache limits daily activities, including school or work activities [35, 36]. In contrast to the “low pressure” headaches that occur in a hyperdrainage state, in CCD, lying down does not reduce the severity of pain. Other manifestations of increased ICP may include diplopia, ataxia, dizziness, and disturbances of consciousness. Cases of acute deterioration leading to death have also been described [26].
Diagnostics
In a number of patients, upon examination, a characteristic deformation of the skull is revealed: microcephaly, scaphocephaly, plagiocephaly. X-rays reveal thickening of the bones of the arch, pronounced “finger impressions”, erosion of the internal plate from the pressure of adjacent grooves, thickening or compaction of the diploe, overlapping of bones in the suture area and their synostosis. Neuroimaging demonstrates normal or slit-like ventricles that do not always dilate even during an exacerbation. This is due not only to a decrease in brain compliance, but also to the absence of intraventricular obstruction [22]. On K.T. and MRI reveals a narrowing of the convexital subarachnoid spaces, as well as overfilling of the cranial cavity, especially in the posterior cranial fossa. In this case, both ascending and descending dislocation of the cerebellum can develop [24, 37]. An increase in ICP does not always lead to changes in the fundus [22]. With invasive ICP monitoring in such patients, A. Sandler et al. [31] found a correlation between headaches and the appearance of plateau waves of increased ICP.
Treatment
In case of radiographically confirmed secondary craniosynostosis and the presence of signs of CD (clinical manifestations of intracranial hypertension, narrowing of the subarachnoid spaces and cerebral ventricles), surgical intervention aimed at decompression of intracranial structures is indicated. Additional criteria may include thickening of the bones of the calvarium, pronounced “finger impressions,” and acquired Chiari malformation.
In 1974, F. Epstein et al. [20] published the results of subtemporal craniectomy performed on 2 children with narrow ventricles who had previously received shunt systems. Essentially, this method creates an artificial surgical fontanel, providing additional space for the brain, and also making it possible to palpate the increased pressure. Such decompression can be performed on one or both sides [22]. However, the authors themselves noted the low effectiveness of such interventions and unacceptable cosmetic consequences: due to the protrusion of the temporal flaps, the head took on the shape of a cloverleaf [22]. Another method used by F. Epstein et al. [11] in 2 children with shunts, there was skull fragmentation - “a radical expansion of the skull... by fragmentation of the skull from the coronal suture to the transverse sinus posteriorly and to the squamosal sutures laterally.”
Open reconstructive interventions aimed at increasing the volume of the skull have become widespread [1, 4, 6, 17, 38]. Particularly noteworthy is the fact that in case of secondary dislocation of the cerebellum, supratentorial reconstruction of the skull is pathophysiologically more justified than decompression of the posterior cranial fossa [24]. When performing reconstruction, it is advisable to replace the valve of the shunt system with a valve with a higher pressure or a programmable valve, or to add an anti-siphon device to the system [1].
Another effective method for correcting secondary craniosynostosis and CD is the use of distraction devices. Distraction osteogenesis can be defined as bone growth surgically induced by applying distending forces at the osteotomy site [39]. The simultaneous use of invasive ICP monitoring sensors and gradual distraction of the skull bones makes it possible to individualize the technique in relation to each patient, performing distraction to the required amount, at which ICP parameters are normalized [31].
Emotional support
The physical side of hydrocephalus is only part of the problem of this disease. The patient and his relatives need to take into account his emotional factors.
Although surgery should resolve your hydrocephalus to some extent, you may feel fearful, depressed, irritable, or doubtful. If the patient is a child, it should be taken into account that he has the same feelings as an adult. If your child is feeling out of shape or uncomfortable because they need to visit the doctor frequently or have repeated tests, it is best to reassure them with simple explanations. If he knows what awaits him, he will be more willing to cooperate with you. Children, like adults, as a rule, do not like unpleasant surprises. A calm atmosphere among loving loved ones is the best environment for children. It is advisable to explain the phenomenon of hydrocephalus in words that the child can understand.
It is very important to know how the child feels and be able to explain to him what he is experiencing. The needles hurt. It is natural to cry and want to get rid of them. Being admitted to hospital is a new challenge for your child. You must tell him the truth in order to gain and secure his trust. Sincerity is the best way to maintain your child's trust.
Children over ten years of age are generally able to comprehend more complex concepts. They may associate signs and symptoms with their illness. Restrictions associated with the disease are easier for them to bear. Tell your doctor about your feelings and give him the right to guide you. Some people share their feelings with close friends, others need professional help. The health professionals treating you or your child are interested in your well-being and their goal is to do what is best for you and your loved ones.
Patients and the patient's parents should communicate with their doctor quite frequently. It is important to actively participate in this communication so that your doctor can better understand your needs and the needs of your loved ones.