What is axonal polyneuropathy
Polyneuropathy (also known as polyneuritis) is a clinical syndrome that occurs due to a number of factors affecting the peripheral nervous system and is characterized by vague pathogenetic changes. The disease occupies one of the leading places in the list of ailments of the peripheral nervous system, second only to vertebrogenic pathology, which is superior in the complexity of the clinical picture and the consequences that develop because of it.
Asconal polyneuropathy is considered an interdisciplinary problem; doctors of various specializations often encounter it. First of all, people with this disease contact a neurologist. The frequency of the syndrome occurring is unknown, since there are no statistical data.
At the moment, only three important pathomorphological mechanisms are known that lie at the origins of the formation of polyneuropathy:
- Wallerian degeneration;
- primary demyelination;
- primary axonopathy.
According to the immunological theory, polyneuropathy is the result of the cross-production of immune globulins that destroy their own cells, resulting in tissue necrosis and muscle inflammation.
Researchers put forward a number of hypotheses for the occurrence and problems of the course of axonal polyneuropathy:
- Vascular. It is based on the involvement of blood vessels in the process, through which oxygen and nutrients enter the peripheral nerves. The characteristics of the blood change in terms of qualitative and quantitative composition, which can lead to ischemia of nerve endings.
- Oxidative stress theory. The formation of the disease is attributed to a disturbance in the metabolism of nitric oxide, as a result of which the potassium-sodium mechanisms underlying the formation of nervous excitation and the conduction of impulses along the nerves change.
- Theory of deactivation of nerve growth factors. It suggests that the disease occurs due to a lack of axonal transport with the subsequent development of axonopathy.
- Immunological. Explains the development of the disease as a result of cross-formation of antibodies to the structures of the peripheral nervous system, which is accompanied by autoimmune inflammation and then necrosis of the nerves.
Even with the use of ultra-modern diagnostic methods, it is difficult to find a reliable cause of the pathology; it is possible to find out only in 50-70% of victims.
There are a lot of factors for the occurrence of polyneuropathy of the lower extremities of the axonal type. However, even innovative research methods do not allow us to establish the true etiology of the disease.
Expert opinion
Author: Alexey Vladimirovich Vasiliev
Head of the Research Center for Motor Neuron Disease/ALS, Candidate of Medical Sciences, doctor of the highest category
Axonal polyneuropathy is one of the most dangerous neurological diseases, accompanied by damage to the peripheral nervous system. During the disease, peripheral nerve fibers are destroyed.
There are several reasons for the occurrence of axonal polyneuropathy. The most common:
- Diabetes mellitus disrupts the structure of the blood that nourishes the nerves, which in turn causes a disruption in metabolic processes.
- Long-term deficiency of B vitamins. They are the most important for the proper functioning of the nervous system, so a long-term deficiency can lead to axonal polyneuropathy.
- The effects of toxins on the body. These include a variety of poisonous substances, for example, alcohol, as well as HIV. In case of poisoning with hazardous substances, the disease can develop within a few days.
- Hereditary factor.
- Guillain-Barre syndrome.
- Various injuries, which also include long-term compression of the nerves, which is typical for hernia or osteochondrosis.
Treatment of axonal polyneuropathy must be comprehensive, otherwise the desired effect will not be achieved. It is strictly forbidden to self-medicate and if the first symptoms occur, you should immediately consult a doctor. Doctors at the Yusupov Hospital select treatment individually for each patient. Depending on the severity of the pathology and symptoms, complex treatment is prescribed under the supervision of experienced specialists.
Archives
Short Wiklad
Dana L. Newswanger, Charles R. Warren Am Fam Physician 2004;69:2405-10.
Guillain-Barré syndrome (GBS) is a name for a heterogeneous group of immune-mediated peripheral neuropathies. Similar to all variants of GBS, there is a rapidly increasing polyradiculoneuropathy, which is the starting point, most often an infection. This condition manifests itself in the form of symmetrical motor paralysis with or without sensory and autonomic disorders.
Population studies were carried out in various countries around the world to estimate the river frequency of GBS - the results of the study found 1-3 episodes/100 thousand. os_b on the river. It occurs in all age groups, although even less often in children. In the age range of people up to 30 years of age, the average frequency is remarkably stable - 1.3–1.9 episodes/100 thousand. osib. The first peak of illness correlates with an increased risk of infection with cytomegalovirus and Campylobacter jejuni. The reason for the onset of illness in the elderly is unknown, but is probably due to defects in immunosuppressive mechanisms. Another pattern is the evolution of the frequency of illness in women during pregnancy and in the postnatal period. According to large epidemiological studies carried out in Sweden, the level is low during the gestation period, but is moving forward during the next few months after the end of pregnancy.
In a patient with GBS, the remaining weakness is manifested, which is accompanied by burning dysesthesias at the end. The tone is more pronounced in the proximal parts of the ends; more often in the legs, not the arms. Paresthesias are eliminated, as they expand proximally, but not beyond the wrist and ankles. Deep tendon reflexes occur several days after the onset of symptoms.
The progressive phase of the syndrome lasts from several days to several years. Almost 73% of patients reach the point of impaired function within 7 days, 98% within 4 days. The progressive phase is followed by a plateau phase (persistent, unchangeable symptoms), after which renewal begins. The period of time until symptoms of illness subside is already varying among different patients.
Inheritance of damage to the cranial nerves in patients may cause disorders on the side of potion-bearing slurries, mimetic and nutmegs, and forging. Such patients should be hospitalized for dynamic care. Approximately 30% of people who fall ill with GBS will require external auxiliary ventilation during the early stages of illness. The poor prognosis is mainly due to the high level of illness - the mortality rate reaches 20%, especially in patients who require new support for their health. Biel, another broadened sign of GBS, disappears in about half of the patients and is even more unpleasant in nature, trying to get rid of minimal problems. The most common in meat is the belt of the upper ends, the back and the rear part. Subjectively, illnesses are described as unacceptable, which suggests muscle discomfort that follows physical rights. It may be accompanied by fleshy spasms and severe pain.
Diagnosis
GBS is the most widespread variant of a rapidly progressive disease of the peripheral nervous system. However, from this, especially at the beginning of the disease, there are a number of other disorders (Table 1).
Table 1. Differential diagnosis and manifestations of diseases that are classified as Guillain-Barré syndrome
| Blockage of the main artery (asymmetric paresis of the ends) Botulism (paralysis) Intoxication with important metals (disorientation, psychosis, organic brain disorder syndrome) Hypophosphatemia (restlessness, anxiety, hyperventilation syndrome, normal liquor readings) Metabolic myopathies (also accompanied by symptoms of cerebral and cerebellar damage) Myasthenia (weakness that improves after recovery) Neoplastic meningitis (asymmetric spastic paralysis) Detection of neurotoxins from marine products (spontaneous exposure within 24 years) Paraneoplastic neuropathy (chronic stab) Poliomyelitis (current fever disorder with meningitis) Polymositis (chronic condition, affected by swelling of the proximal limbs) Spinal cord compression (asymmetrical neurological symptoms) Tick paralysis (every day sensitive disorders, normal liquor readings) Transverse myelitis (Raptian double leg weakness, primary sensory deficit) Vasculitic neuropathies (mononeuropathy) |
The diagnosis of GBS is based on typical clinical manifestations; This verification includes additional electrophysiological diagnostics and monitoring of the spinal cord (SMR) (Table 2).
Table 2. Diagnostic criteria for typical Guillain-Barré syndrome
| Signs needed to make a diagnosis |
| Progressive double weakness of the arms and legs Areflexia |
| Signs that clearly confirm the diagnosis |
| Progression of symptoms over several days (maximum - up to four years) Clear symmetry of manifestations Minor sensitive symptoms Damage to cranial nerves (especially double weakness of facial muscles) Dressing begins 2–4 days after the start of progression Vegetative damage The number of days of fever per ear of illness High concentration of protein in liquor, protein content - up to 10 cells/mm3 Typical results of electrophysiological studies |
| Signs that include a diagnosis |
| Diagnosis of botulism, myasthenia, polyomyelitis and toxic neuropathy Disorders of porphyrin metabolism Recent history of diphtheria Totally sensitive symptoms without weakness |
| The diagnosis of Guillain-Barré syndrome is based on typical clinical symptoms, electrophysiological findings and spinal cord analyses. |
Golovni Danі Elektrophizihiologiy Method as Doslіzhennya, Yaki allow to let the SGB-the n-reflex, nizya amplituda potatziyaliv di chutlivikh, the pathologic f-Khville. On their basis, it is possible to choose nutrition and specific treatment for the onset of illness, but an accurate diagnosis can only be made approximately 5 days after the development of symptoms.
Characteristic changes in the SMR include increased protein content (more than 0.55 g/dL) without pleocytosis (increased cell count in the liquor). Often, the CMR is normal in the first 48 years after the development of symptoms, and until the end of the first period after which the rhubarb protein in it moves. Due to the increase in the number of leukocytes in the liquor (from 10 to 100 cells/mm3) in a patient with typical signs of GBS, the incidence of Lyme disease, neoplasm, SID, sarcoid meningitis and Others will fall ill.
GBS has five distinct variants: acute demyelinating polyradiculoneuropathy (GDP), acute motor axonal neuropathy (GMAN), acute motor sensory axonal neuropathy (MSAN), Miller Fisher syndrome and acute autonomic neuropathy. Whenever there are severe symptoms, axonal forms show a worse prognosis, which indicates the need for a specific type of illness. The rest are divided electrophysiologically and pathologically (Table 3).
Table 3. Variants of Guillain-Barré syndrome
| Gastrointestinal demyelinating polyradiculoneuropathy (GDP) |
| Autoimmune disorder, mediated by antibodies Triggered by a viral or bacterial infection that transmits the disease itself Electrophysiological studies demonstrate demyelinization Inflammatory demyelinization may be accompanied by axonal disruption Remyelinization is evident after immune reactions have occurred |
| Gostra motor axonal neuropathy (GMAN) |
| Suto motor axonal form of neuropathy 66% of patients are seropositive for campylobacteriosis In electrophysiological studies, sensitive nerves are unchanged, motor functions are reduced and completely damaged Oduzhannya zazvichiy nabagato shvidshe A high percentage of the sick are children |
| Gostra motor-sensory axonal neuropathy (GMSAN) |
| Similar to Wallerian degeneration of myelinated motor and sensory fibers Minimal combustion and demyelinization Close to GMAN, due to the fact that with GMSAN sensory nerves and nerves are affected Make you sick when you grow up |
| Miller Fisher syndrome |
| Redkisny Stan Severe evolutionary ataxia, areflexia, mild weakness at the end and ophthalmoplegia Loss of sensitivity is not typical, but proprioception may be impaired Demyelinization and inflammation of the III and VI cranial nerves, spinal nodes and peripheral nerves Decreased daily potentials of sensitive nerves, causing the daily tibial H-reflex Symptoms disappear within 1–3 months |
| Gostra autonomic neuropathy |
| The most common variant of Guillain-Barré syndrome It turns out that both the sympathetic and the parasympathetic nervous system Sometimes there are cardiovascular disorders (postural hypotension, tachycardia, hypertension, arrhythmias) Blurred vision, dry eyes and anhidrosis Clothes in behavior and often inappropriately Frequently suffer from sensitive symptoms |
| Therapy with additional plasmapheresis and intravenous infusion of high doses of immunoglobulin should begin immediately after diagnosis. |
What to do to stop being sick
Acute infectious diseases are caused by drugs that prevent GBS in 2/3 cases. An overreaction between the pathogen and nerve tissue triggers an autoimmune reaction. Patients are encouraged to report respiratory infections or gastroenteritis, which may lead to neuropathy.
A 1995 fall-control study of 103 patients with GBS found that 26% were seropositive for C. jejuni
equal to 2% in the control group and 1% in the control group, compatible with age.
70% of patients infected with C. jejuni
reported the presence of diarrhea in the interval of 12 days before the onset of neurological manifestations. Other trigger infections include cytomegalovirus, VIL, Epstein-Barr virus and chickenpox.
Electrophysiological studies demonstrate that HMAN and HMSAN are detected more often in patients with GBS infected with C. jejuni
, aligned with the State Traffic Safety Inspectorate.
Infection with C. jejuni
is also associated with increased fatigue, axonal degeneration, and significant excess disability.
Recent influenza immunization has also been associated with GBS. One study looked at the incidence of GBS during the peak period of influenza illness in 1992–1993 and 1993–1994 and revealed a rate of 1–2 incidences per 1 million vaccinations.
Based on data from 2003, the System monitored side effects after vaccination carried out by the Center for Disease Prevention and Control and the Administration of Liqueur and Food Products of the United States, the risk of development associated With immunization of GBS there is a lower risk of developing important influenza. In addition, regardless of the increased doses of the prescribed vaccine during the remaining flu seasons, the number of episodes of GBS becomes stable.
Likuvannya
Treatment of GBS includes two components: supportive (basic) and specific therapy. When patients go through the gastric phase of illness, then in most cases the functions are restored. However, if polyneuropathy occurs, it may worsen to the extent that endotracheal intubation and mechanical ventilation will be necessary until symptoms appear.
Therefore, all patients with GBS should be hospitalized for continuous monitoring for respiratory failure, dysfunction of cranial nerves and autonomic disorders. The rest may manifest as arterial pressure, cardiac arrhythmias, a sign of pseudo-obstruction of the scutulo-intestinal canal and obstruction of the septum. It is necessary to ensure the prevention of deep vein thrombosis, as such patients often suffer from weakened tracts of rich veins.
If respiratory weakness develops, it is necessary to consider the possibility of vibular endotracheal intubation. The progression of mental insufficiency can actually be transferred using additional parameters (Table 4).
Table 4. Indications for intubation
| Forced life capacity is less than 20 ml/kg |
| Maximum inspiratory pressure less than 30 mm H2O |
| Maximum expiratory pressure less than 40 mm H2O |
| Progression is noted with a reduced vital capacity of the leg, the maximum inspiratory and expiratory pressure is 30% lower |
Diseases that cannot support minimally functioning lungs will require intubation. Continuous serial assessment of respiratory signs during rapid progression is critically important. Additional predictors of the need for mechanical ventilation are: (1) the period from the onset of GBS to hospitalization is up to 7 days; (2) the inability of the sick person to independently raise his arms and head; (3) the unworthiness of the sick person; (4) the presence of an effect on cough in chronic diabetes and (5) an increase in the level of liver enzymes. Predictors of the need for mechanical ventilation in patients with already terminal vital capacity include the period from the onset of GBS to hospitalization up to 7 days, the patient’s absence from self-pressure The head and vital capacity indicators are less than 60% of those previously transferred.
Such patients also need to take care of pain, one of the important scars. Narcotic drugs must be controlled through the movement of the risk of intestinal obstruction. Physiotherapy through superficial massage, passive exercise and frequent changes in body position can provide significant pain relief. Why use carbamazepine (Tegretol) and gabapentin (Neurontin) as adjuvant therapy? Patients who took these agents had fewer drug needs, minimal side effects, and sedation at levels similar to those who received placebo.
Specific therapy must be started immediately after diagnosis. This includes internal infusion of high doses of immunoglobulin (IVIG; dosed at 400 mg/kg/day for 5 days) and plasmapheresis (5 sessions for 5–8 days). To determine how effective IVIG is compared with plasmapheresis for GBS, a large-center study was carried out and carried out on 150 patients over a period of 4 years. There was no statistically significant difference in the rates of disability between both groups. It was found that IVIG and plasmapheresis are however effective. A recent meta-analysis of the largest study in the Cochrane database suggests that offensive methods have an effect in accelerating the recovery of GBS in patients who require outside assistance during walking.
380 ailments did not have a dodatkovikh of the pass on the posdnani і plasmaphaznino to the monotherapy - Rizznitsa in the rivniye reciditratically meaningful bools in the ilmato -centered. Immunotherapy should be started very early, immediately after the appearance of motor symptoms, but it will not cause mild seizures without clear hearing defects.
Patients who began to experience plasma exchange congestion early on were less likely to require mechanical ventilation and have a short period of hospitalization. This procedure involves the filtering of circulating immune complexes from the blood, which may be related to the pathogenesis of GBS. A French group with plasmapheresis for GBS has come to the conclusion that for patients with mild manifestations of the disease two sessions are sufficient, while patients with severe forms will need two additional sessions. There is a difference between the optimal number of procedures, and based on almost all results, the effect occurs in 4–6 sessions. Today, this method of treatment is considered to be the only effective method of isolated supportive therapy. Moreover, although it is greatest in patients who are able to walk, and in the 2nd period before the onset of illness, it has its positive aspects in immobilized patients in the range up to 30 days after illness develops.
Following plasmapheresis, there is a rare risk of developing a type of sepsis that may result in a decrease in the level of immunoglobulin in the blood. When using replacement infusion of fresh frozen plasma, there is a clear risk of infection with viral infections (hepatitis, HIV).
VVIg has great advantages over plasmapheresis, which is easier to overcome, it is less complicated and easier for the patient. This method is recommended for patients with GBS who cannot collapse without outside help in the interval of 2–4 days after the onset of symptoms. It is important that with this treatment modulation of the immune system is achieved through quite heterogeneous mechanisms from the acquisition of constant and variable regions in IgG molecules, as well as receptors of macrophages and B-cells. Pathological antibodies can bind to IgG, which makes them easier to remove. In addition, through the activation of an as yet unclear mechanism, the function of CD8+ T-cells is enhanced.
Regardless of all the positive aspects, during therapy with the help of IVIG there are some side effects, swelling, increased plasma volume, and immunoglobulin traces should be carefully infused in case of congestion of the heart and the liver. kovіy insufficiency. Patients may develop fever, myalgia, headaches, nausea and vomiting, and “flu-like” symptoms may appear spontaneously, without any rejoicing. Also, aseptic meningitis, neutropenia and hypertension may occur. Data on a history of anaphylactic reactions to immunoglobulins and contraindications for re-stagnation of the remaining ones. The risk of hepatitis C infection has significantly decreased due to the increased modification of purified forms of drugs.
It was assumed that corticosteroids are present in the liquid GBS as a result of their immunosuppressive authorities. An analysis of randomized follow-up studies in the Cochrane database that included hormone therapy and uniquely failed to demonstrate any difference in predictive value. This class of drugs is excluded from standard treatment regimens for GBS.
Forecast and clothing
Approximately 85% of patients with GBS achieve normal and functional clothing within an interval of 6–12 months. The maximum is for 18 months from the beginning of the disease. However, some patients suffer from persistent weakness, areflexia and paresthesia. Approximately 7–15% of patients suffer from excessive neurological inheritances such as double foot paresis, hand atrophy, sensory ataxia and dysesthesia. The mortality rate becomes less than 5% in specialized centers. The causes of death were adult respiratory distress syndrome, sepsis, thromboembolism of the legen artery and cardiac arrest.
A number of factors in the acute phase of illness are predictors of poor sleep. This century is over 60 years; important, rapidly progressing form of the disease; low amplitude of nerve conduction during distal stimulation, indicating axonal alignment. Other factors include mechanical ventilation for more than 1 month and the presence of illness before the development of GBS. In general, the long-term prognosis is poor due to the degree of importance of the acute phase and the delay in initiating specific therapy. Relapses occur in a small number of cases (3–5%), and are not directly related to treatment or any other factors.
Prepared by Yuriy Matvienko
- 1 Dysesthesia is a guilty feeling that is inadequate to the patient (for example, torsion is perceived as pain, pain, temperature, etc.). There may be signs of pathology in the thymic part of the measles of the great pectus, thalamus or sensitive conductors of the spinal cord.
- 2 Paresthesia - spontaneously disappearing sensations, tingling, “repeated goosebumps”, swelling, tightening; Be careful in case of damage to the peripheral nerves of the terminals, or in case of subdivision of postcentral measles.
- 3Lyme disease is a recurrent multisystem illness caused by Borrelia burgdorferi, which in most cases begins with chronic migratory erythema, associated myalgias, arthritis of the great lobes, symptoms of nervous system disorders cardiac-vascular systems.
- 4 Wallerian degeneration is fatty degeneration of nerve fibers that are separated from the trophic center of the neuron (body).
- 5 Ataxia is a symptom complex of impaired statics and coordination in connection with the disorder of the normal functioning of the muscles of agonists and antagonists, caused by damaged cerebellum and ligaments, frontal measles, vestibular ї system, tract of deep sensitivity.
- 6 Ophthalmoplegia - abnormality of the apple. Most often it occurs when there is damage to the spinal cranial nerves (parochal, trochlear and aqueductal).
- 7 Proprioception - we can recognize the subdivisions of proprioceptors located in tissues. In case of ruins, it will ensure a return aference and thus control over the final act of the ruins.
- 8 Plasmapheresis is the removal of plasma from collected blood with retransfusion of blood elements to the donor. Involvement in the treatment of neuroimmune diseases (Guillain-Barré syndrome, myasthenia, multiple sclerosis).
- 9 Sensitive ataxia is a syndrome of static-coordinating disorders that occurs when the sensory tract is affected in various areas (peripheral nerves, posterior spinal cord, medial lemniscus of the brain, thalamus). A characteristic sign is an increase in ataxic symptoms in the absence of visual control of the patient’s side.
Causes
The most common causes of axonal polyneuropathy of the lower extremities:
- exhaustion of the body;
- long-term deficiency of B vitamins;
- ailments leading to dystrophy;
- acute infections;
- toxic damage from mercury, lead, cadmium, carbon monoxide, alcoholic beverages, methyl alcohol, organophosphorus compounds, medications taken without the consent of a doctor;
- diseases of the cardiovascular, hematopoietic, circulatory and lymphatic systems;
- endocrinological pathologies, including insulin dependence.
The main factors that provoke the development of motor or sensorimotor axonal polyneuropathy are:
- endogenous intoxication in renal failure;
- autoimmune processes occurring in the body;
- amyloidosis;
- inhalation of toxic substances or vapors.
The disease can also be caused by heredity.
A lack of B vitamins in the body, and especially pyridoxine and cyanocobalamin, has an extremely negative effect on the conductivity of nerve and motor fibers and can cause sensory axonal polyneuropathy of the lower extremities. The same happens with chronic alcohol intoxication, helminthic infestation, and diseases of the gastrointestinal tract, which impair the rate of absorption.
Toxic poisoning with drugs, aminoglycosides, gold salts and bismuth occupy a large percentage in the structure of factors of axonal neuropathy.
In patients with diabetes, peripheral nerve function is impaired due to the neurotoxicity of ketone bodies, i.e. metabolites of fatty acids. This happens due to the body’s inability to use glucose as the main source of energy. Therefore, fats are oxidized instead.
With autoimmune diseases occurring in the body, the human immune system attacks its own nerve fibers, perceiving them as a source of danger. This occurs due to a provocation of the immune system that occurs when taking immunostimulating medications and unconventional treatment methods carelessly. Therefore, in people who are prone to autoimmune diseases, the triggering factors for axonal polyneuropathy are:
- immunostimulants;
- vaccines;
- autohemotherapy.
With amyloidosis, a protein called amyloid accumulates in the body. It is this that disrupts the basic functions of nerve fibers.
Causes of peripheral neuropathy
There are many factors that can cause peripheral neuropathy, so it is often difficult to determine the cause of the disease. In general, neuropathy is classified into three main groups:
- Acquired neuropathies
caused by exposure to toxins, injury, disease, or infection. Known causes of acquired neuropathy include: Diabetes; - Some rare hereditary diseases;
- Alcoholism;
- Poor nutrition and vitamin deficiency;
- Certain types of cancer and the effects of chemotherapy used to treat them;
- Situations where the nerves are attacked by the body's immune system;
- Some medications;
- Diseases of the kidneys or thyroid gland;
- Some infections (Lyme disease, AIDS).
are not that common. Hereditary neuropathy is a disease of the peripheral nerves that is genetically passed from parent to child.
is diagnosed when the cause of the disease is unknown. About a third of all neuropathies fall into this category.
First signs
The disease usually begins to develop with damage to thick or thin nerve fibers. Often, axonal polyneuropathy has a distal symmetrical distribution on the hands or feet. Neuropathy most often affects the lower extremities first and then spreads symmetrically up the body. The most common primary symptoms of damage include:
- muscle weakness;
- pain syndrome in the limbs;
- burning;
- crawling sensation;
- numbness of the skin.
Symptoms are most pronounced in the evening and at night.
Symptoms
Doctors divide the chronic, acute and subacute course of axonal polyneuropathy. The disease is divided into two types: primary axonal and demyelinating. During the course of the disease, demyelination is added to it, and then a secondary axonal component.
The main manifestations of the disease include:
- weakness in the muscles of the legs or arms;
- spastic paralysis of the limbs;
- feeling of twitching in muscle fibers;
- dizziness with a sudden change in body position;
- swelling of the limbs;
- burning;
- tingling;
- crawling sensation;
- decreased sensitivity of the skin to high or low temperature, pain and touch;
- impaired speech clarity;
- problems with coordination.
The following symptoms are considered vegetative signs of sensorimotor polyneuropathy of the asconal type:
- rapid or, on the contrary, slow heart rate;
- excessive sweating;
- excessive dry skin;
- change in skin color;
- ejaculation disorder;
- erectile disfunction;
- problems with urination;
- failure of motor functions of the gastrointestinal tract;
- increased salivation or, conversely, dry mouth;
- eye accommodation disorder.
The disease manifests itself in dysfunction of damaged nerves. It is the peripheral nerve fibers that are responsible for the motor functions of muscle tissue, sensitivity, and also have a vegetative effect, that is, they regulate vascular tone.
Disorders of nerve conduction function are characterized by sensitivity disorders, for example:
- crawling sensation;
- hyperesthesia, that is, increased sensitivity of the skin to external irritants;
- hypoesthesia, that is, decreased sensitivity;
- lack of sensation of one's own limbs.
When autonomic fibers are affected, the regulation of vascular tone goes out of control. With axonal demyelinating polyneuropathy, compression of the capillaries occurs, causing the tissue to swell. The lower and then the upper limbs, due to the accumulation of fluid in them, significantly increase in size. Since with polyneuropathy of the lower extremities the main amount of blood accumulates in the affected areas of the body, the patient experiences persistent dizziness when taking an upright position. Due to the loss of trophic function, erosive and ulcerative lesions of the lower extremities may occur.
Axonal motor polyneuropathy manifests itself in motor disorders of the upper and lower extremities. When the motor fibers responsible for the movements of the arms and legs are damaged, complete or partial muscle paralysis occurs. Immobilization can manifest itself in a completely atypical manner - you can feel both stiffness of the muscle fibers and their excessive relaxation. With a moderate degree of damage, muscle tone is weakened.
During the course of the disease, tendon and periosteal reflexes may be strengthened or weakened. In rare cases, a neurologist does not observe them. The disease can often affect the cranial nerves, which are manifested by the following disorders:
- deafness;
- numbness of the sublingual muscles and tongue muscles;
- inability to swallow food or liquid due to problems with the swallowing reflex.
When the trigeminal, facial or oculomotor nerve is affected, the sensitivity of the skin changes, paralysis develops, facial asymmetry and muscle twitching occur. Sometimes, when axonal demyelinating polyneuropathy is diagnosed, the lesions of the upper or lower extremities may be asymmetrical. This happens with multiple mononeuropathy, when the knee, Achilles and carporadial reflexes are asymmetrical.
Diffuse axonal brain injury (imaging issues)
Diffuse axonal damage (DAD) of the brain includes widespread axonal ruptures in combination with small focal hemorrhages, caused by predominantly inertial trauma. In this case, the most characteristic areas of axonal and vascular disorders are the brain stem, corpus callosum, paraventricular zones and white matter of the cerebral hemispheres. At the same time, sliding parasagittal contusions of the brain are possible.
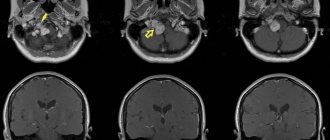
With some experience, a clinical diagnosis of DAP is quite possible. However, it should always be supported by CT or MRI. On CT, diffuse axonal damage is characterized by an increase in brain volume of varying degrees (due to its edema, swelling, hyperemia) with compression of the lateral and third ventricles, subarachnoid convexital spaces, as well as cisterns of the base of the brain. In this case, small focal hemorrhages are often detected in the white matter of the cerebral hemispheres, the corpus callosum, as well as in the subcortical and brainstem structures (Fig. 1).
Rice. 1. Severe DAP of the brain in a 25-year-old victim. CT scan: top row – on the 1st day after TBI, multiple small focal hemorrhages in the deep parts of the hemispheres, subependymal, in the corpus callosum, compression of the ventricular system; middle row - on the 7th day, an increase in the size and density of focal hemorrhages; bottom row – 2.5 months after TBI, pronounced signs of the atrophic process: expansion of the ventricular system, basal and convexital subarachnoid spaces, interhemispheric fissure.
At the same time, even in the acute period, a phenomenon of fluid accumulation (with the density characteristics of cerebrospinal fluid) over the frontal lobes, quite typical for DAP, is detected, mainly in the anterior sections on one or both sides. In mild and moderate forms of DAP, CT scan reveals only signs of a slight increase in brain volume or the computer picture is indistinguishable from normal. Repeated CT studies performed in patients with DAP reveal quite characteristic dynamics. 2–4 weeks after the injury, the phenomena of edema and swelling of the brain regress, small focal hemorrhages are either not visualized or become hypodense. At the same time, the basal cisterns and convexital subarachnoid fissures begin to clearly emerge against the background of a more or less pronounced tendency to expand the ventricular system. Ventriculomegaly and other signs of a diffuse atrophic process often increase further (see Fig. 1).
MRI for DAP is usually more informative than CT, clearly visualizing damage to the corpus callosum, trunk, and other formations. The most common finding is hyperintense areas of various sizes at the border of gray and white matter, in the paraventricular zones, the corpus callosum, and in the brain stem (Fig. 2). Subsequently, the intensity of their image decreases. With small hemorrhages in areas of axonal damage, T1 tomograms may show signs of the presence of derivatives of hemoglobin oxidation; they are especially clearly detected when using the SWAN mode. Multiple areas of decreased signal on T2 and gradient echo scans may be observed for many years after injury.
Rice. 2. Severe DAP. MRI on the 3rd day after TBI: a – T2 in the sagittal projection; b – T2 in axial projection, post-traumatic changes are pronounced in the posterior third and splenium of the corpus callosum; c, d – in T1 in the axial projection, small hemorrhagic foci are visible in the frontal and temporal lobes, the cushion of the optic thalamus on the right; deep coma. After 2 months: d, f – according to T2, g, h – according to T1. changes in the corpus callosum decreased, hemorrhages resolved, the lateral ventricles moderately expanded; deep disability.
Diagnostics
The main research technique, which makes it possible to detect the localization of the pathological process and the degree of nerve damage, is electroneuromyography.
To determine the cause of the disease, doctors prescribe the following tests:
- determination of blood sugar levels;
- toxicology tests;
- complete urine and blood analysis;
- detection of cholesterol levels in the body.
Violation of nervous functions is established by determining temperature, vibration and tactile sensitivity.
During the initial examination, a visual research technique is used. That is, the doctor to whom the victim turned with complaints examines and analyzes such external symptoms as:
- blood pressure level in the upper and lower extremities;
- sensitivity of the skin to touch and temperature;
- presence of all necessary reflexes;
- diagnosis of swelling;
- study of the external condition of the skin.
Axonal polyneuropathy can be identified using the following instrumental studies:
- magnetic resonance imaging;
- nerve fiber biopsy;
- electroneuromyography.
Treatment of axonal polyneuropathy
Treatment of axonal polyneuropathy should be comprehensive and aimed at the cause of the disease, its mechanisms and symptoms. The guarantee of effective therapy is timely detection of the disease and treatment, which is accompanied by an absolute abstinence from cigarettes, alcohol and drugs, maintaining a healthy lifestyle and following all doctor’s recommendations. First of all, the following therapeutic measures are carried out:
- getting rid of toxic effects on the body, if present;
- antioxidant therapy;
- taking medications that affect the tone of blood vessels;
- replenishment of vitamin deficiency;
- regular monitoring of plasma glucose concentrations.
Special attention is paid to treatment aimed at relieving acute pain syndrome.
If peripheral paresis is present, that is, a significant decrease in muscle strength with a multiple decrease in the amplitude of movements, then physical therapy and special physical exercises aimed at restoring tone to muscle tissue and preventing the formation of various contractures are mandatory. Regular psychological support is especially important, which prevents the patient from falling into depression, accompanied by sleep disorders and excessive nervous excitability.
Treatment of axonal polyneuropathy is a long process, since nerve fibers take a long time to recover. Therefore, you should not expect an immediate recovery and return to your usual lifestyle. Drug therapy includes drugs such as:
- pain reliever;
- glucocorticoids;
- B vitamins;
- antioxidants;
- vasodilators;
- agents that accelerate metabolism and improve blood microcirculation.
Drug therapy is aimed at restoring nerve function, improving the conductivity of nerve fibers and the speed of signal transmission to the central nervous system.
Treatment should be carried out in long courses that should not be interrupted, although the effect does not appear immediately. To eliminate pain and sleep disturbances, the following medications are prescribed:
- antidepressants;
- anticonvulsants;
- drugs that relieve arrhythmia;
- painkillers.
Non-steroidal anti-inflammatory drugs are used to relieve pain. But it is worth remembering that they can only be used for a short period of time, since long-term use can lead to damage to the mucous membrane of the gastrointestinal tract.
Physiotherapeutic methods for treating axonal polyneuropathy include:
- magnetic wave therapy;
- mud therapy;
- electrical stimulation;
- acupuncture;
- massotherapy;
- physical training;
- ultraphonophoresis;
- galvanotherapy.
It is physical therapy that allows you to maintain the performance of muscle tissue and maintain the limbs in the desired position. Regular exercise will restore muscle tone, flexibility and increase the range of motion to normal.
Prevention
The patient must take preventive measures that will help avoid relapse or the occurrence of a dangerous disease. They include enriching the diet with vitamins, regular monitoring of blood sugar levels, and complete cessation of smoking, drugs and alcoholic beverages.
To prevent the disease, it is recommended:
- wear comfortable shoes that do not pinch the foot, impairing blood flow;
- regularly inspect your shoes to avoid the formation of fungus;
- avoid walking long distances;
- do not stand in one place for a long time;
- wash your feet with cool water or do contrast baths, which helps improve blood circulation in the body.
Victims in remission are strictly prohibited from taking medications without the consent of the attending physician. It is important to promptly treat inflammatory diseases, take precautions when working with toxic substances that have a detrimental effect on the body, and regularly perform therapeutic physical exercises.