Learn more about diseases starting with the letter “P”: Panic attacks; Duchenne-Erb's palsy; Todd's palsy; Parasomnias; Paroxysmal hemicrania; Paroxysmal myoplegia, Paroxysmal positional vertigo; Peripheral autonomic failure; Hepatic encephalopathy; Pineoblastoma; Pineocytoma; Writer's cramp; Platybasia; Plexites; Brachial plexitis; Humeroscapular periarthrosis; Pneumococcal meningitis Pneumocephalus; Subacute sclerosing panencephalitis; Spinal cord injury.
Pineoblastoma is characterized by a malignant neoplasm. The disease begins with damage to the parenchymal cells of the epiphysis. Occlusive hydrocephalus, damage to the cerebral trunk and cerebellum, all this is characteristic of the course of this disease.
The manifestation may affect intracranial pressure, sleep disturbances, cerebellar syndrome, visual and oculomotor disorders. Pineoblastoma can be diagnosed using neuroimaging, studying cerebrospinal fluid, and histological examination of newly formed tissues. Sequential treatment occurs in 3 stages: neurosurgical operation to eliminate the tumor, radiation therapy, polychemotherapy.
General information
Pineoblastoma belongs to the neuroectodermal type of neoplasm - a poorly differentiated embryonic tumor. In its structure, neoplasia differs little from other malignant tumors, which begin with tissue damage of neuroectodermal origin - retinoblastoma and medulloblastoma.
The tumor begins to progress from the cells of the pineal gland, i.e. gland that produces melatonin, which regulates sleep-wake cycles. The disease is quite rare, accounting for 0.1% of all intracranial neoplasms. Applies to children, mainly males.
How is a treatment plan made?
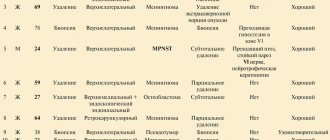
After the final diagnosis, a treatment plan is drawn up. In order to create the most individual treatment program, specifically selected for a particular patient, and to assess the possible risks of relapse of the disease (risk-adapted therapy), the team of treating doctors must take into account certain factors that influence the prognosis of the disease in a particular child (the so-called prognostic factors or risk factors).
Important prognostic factors are the information that was obtained after completing the entire diagnosis: what specific type/type of tumor was found in the child, where exactly the tumor is located, how much it has managed to grow (tumor size) and metastasize. In addition, the biological (molecular biological) characteristics of the tumor tissue (specialists can talk about the molecular profile of the tumor) increasingly determine which treatment is considered the most optimal in a particular case. The age of the child and his general health also matter. The age of the child at the time of diagnosis determines whether the child can be sent for radiation therapy or not. All these factors are included in the treatment plan in order to obtain the most effective treatment result for each patient.
Causes of pineoblastoma
The occurrence of pineoblastoma is associated with mutation of individual pinaeocytes, which are capable of rapid division. Mutations are sporadic, meaning a hereditary predisposition is possible. The exact reasons for the change in the state of pinaeocytes have not been identified. Presumably, mutations are caused by the following factors:
- Carcinogens. These substances can adversely affect the genetic mechanism of cellular structure. Food fillers - preservatives, artificial additives, flavors, dyes - can cause a carcinogenic effect. Also components of household chemicals, paints and other similar materials. Exposure to carcinogens during pregnancy is greater.
- Ionizing radiation. It affects the chromosomes of living organisms. Increased radiation, the use of radiation therapy in the treatment of certain diseases.
- Pregnancy with complications. Cell dysfunction can be caused by fetal hypoxia, exposure to toxins (drinking alcohol, smoking, taking drugs), and infections inside the womb. After the baby is born, cells remaining in the pineal gland can contribute to the development of a tumor.
Prognosis of pineoblastoma
The prognosis for survival of the disease depends on the following factors:
- the size and prevalence of the tumor before surgery;
- presence of residual cancer cells after surgery;
- patient's age.
The lethal outcome is caused by compression of the brain, hemorrhage into the ventricles, and the involvement of the vital centers of the medulla oblongata in the process. Combined 3-stage treatment helps to increase the life expectancy of patients. The predisposition of the tumor to implantation spread and metastasis explains the high rate of relapses.
Pineoblastoma in children under 5 years of age has a more malignant course; 5-year survival can be only in 15% of cases; in children over 6 years of age, the prognosis is much more favorable. If the tumor disseminates, patients die within a year from the onset of clinical symptoms. Operated patients survive to the five-year mark in 60-70% of cases. Premature death is possible if the tumor is inoperable.
Pathogenesis
Why malignant cells appear in the pineal gland is unknown. Here it is relevant to consider many different changes in the genetic structure within cells that can transform the properties of pinaeocytes.
The effect manifests itself in the form of uncontrolled reproduction and lack of differentiation of pineoblasts. Pineoblastoma is characterized by the instant spread of pathology in the tissue and active infiltrative growth. A malignant tumor leads to the destruction of the tissues of the pons and medulla oblongata, spreading to the meninges and subarachnoid space.
The pineal gland is located next to the aqueduct of Sylvius, which drains cerebrospinal fluid into the fourth ventricle. A growing pineoblastoma puts pressure on the aqueduct of Sylvius, thereby blocking the flow of liquor. There is an accumulation of cerebrospinal fluid in the third ventricle, the formation of occlusive hydrocephalus, the manifestation of which is characterized by symptoms of intracranial hypertension.
If we talk about the visible concept of pineoblastoma, then the tumor is a dense, elastic neoplasm of a brown hue. A study under the micro effect will show that the tumor contains small monomorphic cells with hyperchromatic nuclei.
Clinic
At the time of clinical presentation, almost all patients have HCF with typical symptoms (H/P, vomiting, drowsiness, memory impairment, abnormal increase in head circumference in infants, seizures). There may be Parinaud's syndrome (or Sylvian aqueduct syndrome). Boys with choriocarcinoma or germinoma with scintiotrophoblastic cells may experience precocious puberty as a result of the action of βhCG secreted in the cerebrospinal fluid, similar to the action of LH. Metastasis to the cerebrospinal fluid may cause radiculopathy and/or myelopathy
Symptoms
The very first symptoms at the initial stage of the disease: progressive headache, vomiting, nausea, decreased performance of vision, sometimes elevated body temperature, whims and anxiety in young children, rarely the presence of convulsive syndrome.
Penetration of the tumor into the midbrain may be accompanied by strabismus, bilateral ptosis, and double vision. Damage to the cerebellum adversely affects the ability to walk normally, measured movements, and control of body coordination. Improper melatonin production is characterized by sleep disturbances. There is also a possibility of hemiparesis, poor sensitivity of body parts, and behavioral disturbances.
Localization
The boundaries of the pineal region: behind - the splenium of the corpus callosum and the choroid plexus, in front - the quadrigeminal plate and the tegmentum of the midbrain, rostrally - the posterior part of the third ventricle, caudally - the cerebellar vermis.
Tumors in this region are more common in children (they account for 3-8% of pediatric brain tumors) than in adults (≤1%). A distinctive feature of these tumors is their diversity, which is due to the different tissues that are normally present in this area. Moreover, many tumors are of mixed nature. Pineoblastoma is a malignant tumor that is considered a primitive neuroectodermal tumor (PNET).
Complications with pineoblastoma
This disease is characterized by a rapid increase in intracranial pressure due to occlusion of the cerebrospinal fluid channels. The condition is aggravated due to damage to the third ventricle. Due to the unfavorable course of the disease, the tumor spreads to the lateral ventricles, which practically leads to dysfunction of the ventricular system.
A strong increase in ventricular volume puts pressure on the brain. Given the ability of pineoblastoma to manifest itself in metastases, secondary metastatic foci are possible in the areas of the spinal cord and brain. Hemorrhage into tumor tissues with blood breaking into the ventricles can lead to serious and irreversible consequences.
Complications may also be associated with pressure and the growth of pineoblastoma in the tissue of the medulla oblongata, where the vital centers of the cardiovascular and respiratory systems are located. When cardiovascular regulation is affected, it is fatal.
How is the disease diagnosed?
If the child’s medical history (history) and the results of an external examination [external examination] give the pediatrician a suspicion of a malignant tumor in the central nervous system, then the doctor refers him to a clinic that specializes in pediatric and adolescent oncology (clinic of pediatric oncology and hematology). Because if such a tumor is suspected, then a full examination is carried out by specialists of various profiles. First, they must confirm the diagnosis of whether the child actually has a malignant tumor of the central nervous system [brain tumor]. Secondly, if the diagnosis is confirmed, they must say what specific type of tumor the child has and how far the disease has spread throughout the body. Only by answering these questions can we optimally plan treatment tactics and give a prognosis for the disease.
What tests and studies are done to confirm the diagnosis?
To check whether the child has an embryonic tumor of the central nervous system or pineoblastoma, the medical history is carefully studied again and an external examination is performed. To make an accurate diagnosis, doctors first need to do diagnostic imaging - magnetic resonance imaging (MRI), sometimes also CT, that is, computed tomography. Using these methods, you can accurately determine whether there is a tumor in the brain and whether it has managed to metastasize into the spinal canal. In the pictures you can see exactly where the tumor has grown, what size it is, where the borders of the tumor with neighboring structures are. They can also be used to accurately see whether the child has hydrocele.
To definitively confirm the diagnosis, a piece of tumor tissue (biopsy) is needed. She is sent for histological and molecular genetic analysis. As a rule, during an operation to remove a tumor, a part of the tumor is taken and it is this that is sent for this diagnosis. The volume of histological studies and, first of all, molecular genetic analyzes has grown greatly in recent years. Modern laboratory research methods are able to describe the molecular genetic properties of tissue so accurately that this makes the diagnosis more accurate. Depending on the results of this diagnosis, specialists also receive information about how the disease will progress (disease dynamics), for example, how the tumor is able to grow and how quickly. Already today, based on the results of molecular genetic studies, doctors decide on what plan they will use to treat the child. In the future, the value of this information for modern diagnostics will become even greater.
Diagnostics to determine the extent of the disease
If the diagnosis of embryonal tumor of the central nervous system or pineoblastoma is confirmed, then specialists conduct additional tests and studies to understand how much cancer cells have spread throughout the central nervous system. For example, MRI images of the entire central nervous system (that is, images of the brain and spinal cord) show (that is, visualize) those metastases that doctors call macroscopic metastases (those that are visible on the images). Additionally, specialists must conduct a microscopic examination of the cerebrospinal fluid (CSF) in the spinal canal. Because it may contain cancer cells that are not visible on MRI images. Most often, cerebrospinal fluid is taken after surgery, when a puncture is made in the lower back/lumbar spine (lumbar puncture). There is a cavity from which it is easiest to obtain cerebrospinal fluid.
What tests and studies are done before starting treatment?
Before treatment, children may additionally undergo other tests and studies. For example, they do an ECG (electrocardiogram) and an echocardiogram (echocardiogram) to check how the heart is working. Various blood tests are also done to check the general condition of the child’s body, as well as to assess how well individual organs (for example, kidneys and liver) are working, or whether there may be any metabolic disorders. These baseline data are then regularly compared with the results obtained during treatment. If any changes occur during treatment, it is easier for specialists to correctly assess the situation.
Diagnostics
This disease is diagnosed by neurologists and neurosurgeons. A general understanding of the course of pregnancy, the process of childbirth, the postpartum period, and symptoms of the initial stage of the lesion is given by collecting an anamnesis. The neurologist determines the approximate location of the pathology. Further examination involves:
Clinical tests. A complete blood count may show leukocytosis and anemia. Blood biochemistry gives a general picture of the level of ALT, AST, and protein status.
Examination by an ophthalmologist. Ophthalmoscopy is one of the fundamental diagnostic techniques. If this study reveals papilledema, this means increased intracranial pressure.
Study of cerebrospinal fluid. Eliminates infectious damage to the central nervous system. This method reveals significant cytosis, high protein concentration, and the presence of pineoblasts (tumor cells). Determines the condition of red blood cells.
Neuroimaging. Mainly magnetic resonance imaging of the brain, or cerebral computed tomography at an older age. This method is capable of diagnosing neoplasia, its course and localization.
Stereotactic tumor biopsy. This diagnostic method is typical for complex cases when there is a question about neurosurgical treatment. Basically, this is a histological study of the material that is removed intraoperatively.
If symptoms appear in the first year of life, congenital abnormalities of brain development must be excluded. In young children, the first symptoms in the form of vomiting, nausea, and fever can be confused with the manifestation of an intestinal infection.
What are the symptoms of the disease?
Typically, in children and adolescents with embryonal tumor or pineoblastoma, symptoms of the disease appear very quickly, as the tumor itself grows quickly and uncontrollably. Just like other types of brain cancer, the symptoms of the disease depend primarily on the age of the child, as well as on which specific part of the central nervous system the brain tumor grew in and how far it has already spread throughout the body. It is customary for specialists to divide symptoms into general (doctors talk about nonspecific symptoms) and local (doctors talk about specific symptoms).
Nonspecific symptoms (general)
General symptoms appear regardless of where exactly the tumor has grown. They generally appear in other diseases that are not related to tumors of the central nervous system. These may be, for example, headaches and/or back pain, dizziness, loss of appetite, nausea and vomiting (a typical symptom in brain cancer, when a person vomits at all without depending on food intake [vomiting on an empty stomach]; very often this occurs due to lying down in the morning), weight loss, increased fatigue/fatigue, decreased academic performance, loss of concentration, changes in a person's character and behavior, developmental delays.
Most often, these symptoms appear because pressure begins to slowly build up inside the skull. Compression of the internal structures in the skull can be caused by the growing tumor itself, and/or due to the tumor, the free circulation and outflow of cerebrospinal fluid (CSF) is disrupted. Due to a violation of the outflow of cerebrospinal fluid, the child may develop water on the brain (hydrocephalus). If dropsy of the brain appears in infants and young children, when the fontanelles have not yet closed, then they can see how much the head has grown in volume (macrocephaly).
Specific symptoms (local)
Specific (local) symptoms indicate exactly where in the central nervous system the tumor has grown and the functioning of which control centers it disrupts. For example, if a tumor grows in the cerebrum [cerebrum], or in the diencephalon [diencephalon], the child may have motor problems (paralysis) and/or seizures. Also, the child may experience disturbances in vision, sleep, and normal behavior; mood swings and problems regulating appetite may occur. A patient with pineoblastoma may experience gaze paresis. Experts call this form of visual impairment Parinaud's syndrome. Due to the fact that the pineal gland tumor grows in a certain place in the diencephalon, it compresses the center there, and among other things, the eyeballs cannot move upward.
Good to know: if a child has one of these symptoms, or several at once, this does not mean that he has an embryonal tumor, pineoblastoma, or another form of brain cancer. Many of the symptoms mentioned can appear in other diseases, relatively less insidious, which have nothing to do with brain tumors. However, we recommend that if you have certain complaints, you should consult a doctor as soon as possible (for example, if your child has constant headaches, or in young children the volume of the head quickly becomes disproportionately large) in order to find out the exact cause of these symptoms. If doctors really find some type of brain cancer in a child, then they need to begin treating the disease as quickly as possible.
Treatment of pineoblastoma
Modern treatment includes 3 fundamental stages:
- Surgery. The pineoblastoma needs to be removed as much as possible. The reason for excluding this intervention is the growth of the tumor into the brain stem, threatening to damage the vital centers, as well as the involvement of the choroid plexuses, which can lead to severe bleeding during surgery.
- Radiation therapy. Due to the rapid nature of the spread, total irradiation of the spinal cord and brain is used. The frequency, quantity, and radiation exposure are regulated by the radiologist depending on the individual characteristics of the patient.
- Polychemotherapy. It is used in combination with radiation therapy, as palliative treatment, or after neurosurgery. Determined by a chemotherapist, it contains 2-3 cytostatic drugs. Side effects are accompanied by additional symptomatic treatment.
Treatment
The optimal treatment strategy for pineal region tumors still needs to be determined.
Hydrocephalus
The best treatment for patients admitted for acute HCF is external ventricular drainage (EVD). It allows fluid control, prevents peritoneal contamination, and, in a significant number of patients, avoids the need for a permanent shunt system, which is no longer required after surgical removal of the tumor (although ≈90% of patients with germ cell tumors require a shunt). It is important to have access to the ventricle in the postoperative period in case of acute HCF (through the NVD or Fraser burr hole).
Stereotactic techniques
Can be used to establish a diagnosis (biopsy). Caution is required during the procedure, because this area is rich in vessels (vein of Galen, basal vein of Rosenthal, internal cerebral veins, posterior medial choroidal artery), which may be displaced from their normal location.
Complication rate during stereotactic interventions: mortality ≈1.3%, complications ≈7%, 1 case of contamination per 370 patients. Diagnosis rate ≈94%.
A limitation of stereotactic biopsy is that it may not reveal the histological heterogeneity of some tumors. The study showed that there is an association between intervention trajectory and the occurrence of complications. Therefore, they recommend the inferior frontal approach, which passes below the internal cerebral veins. However, another study did not confirm this connection. But they found that complications occurred more often with solid tumors (pineocytoma, teratoma, astrocytoma). Therefore, if difficulties are encountered when first attempting to penetrate the tumor to take a biopsy, they recommend using an open approach. SRS can be used to treat some of these lesions.
Outcomes of surgical interventions Mortality: ≈5-10%. Postoperative complications: new visual field impairment, epidural fluid accumulation, infection, cerebellar ataxia
Prognosis and prevention
Pineoblastoma is predicted to have serious consequences. The course of the disease can be fatal due to compression of the brain, hemorrhage in the ventricles, or damage to certain areas of the medulla oblongata. Three-stage therapy has the potential to prolong the patient's life.
The prognosis is determined by the age criterion and the degree of progression of the tumor process. A patient under 5 years of age is characterized by increased malignancy; surviving to 5 years is possible only in 15% of cases. Children over 6 years of age have a more favorable prognosis. Since the causes and organization of pinaeocyte transformation are unknown, it is impossible to prevent the disease.
But it is important to listen to your body and once again consult with a specialist. At the slightest suspicion of the disease, an MRI or CT scan should be done. You can select a medical center using the service. The patient can choose a clinic based on his own needs (geolocation, price, rating, patient’s age, type of tomograph used, type of study). Registration is carried out by calling the phone number posted on the website. As a bonus, the patient receives a discount on examination in the amount of up to 1,000 rubles.
How are these types of tumors treated?
Children with embryonal brain tumors or pineoblastoma should be treated only by doctors from children's clinics specializing in pediatric oncology. It is there that highly qualified specialists (doctors, nurses) with a specialization in pediatric oncology work and are proficient in modern therapy programs. In these hospitals, doctors of different specialties belong to different working groups, which are constantly in close contact. Together they create treatment plans, discuss and manage their patients. Therapy programs are regularly improved. Their goal is to treat the child as gently as possible, that is, with minimal side complications and long-term consequences.
Treatment of children with embryonal brain tumor or pineoblastoma consists of surgery, courses of chemotherapy and, depending on the age of the child, radiation therapy (irradiation).
Operation
The first step in the treatment of children with an embryonal tumor of the central nervous system or pineoblastoma is surgery. Its goal is complete removal of the tumor without “microscopically visible” remains. This means that after surgery, tumor remnants are not visible under a neurosurgical microscope. At the same time, the neurosurgeon strives, as far as possible, not to damage/affect healthy brain tissue. However, it is often impossible to completely remove an embryonal tumor of the central nervous system or pineoblastoma of the brain due to the complex location of the tumor (that is, the specific place where it grew).
When the tumor is removed, in most children the outflow of cerebrospinal fluid (CSF) is restored if it was disrupted. If the child had dropsy of the brain (hydrocephalus), then even before surgery to remove the tumor, additional surgery may be required to normalize the outflow of cerebrospinal fluid. Some children have a permanent drainage system installed.
Non-surgical treatment stage
Since embryonic tumors of the central nervous system and pineoblastomas of the brain grow into neighboring tissues (experts call in this case “infiltrative tumor growth”), and they often diverge along the cerebrospinal fluid pathways (cerebrospinal fluid system) to other parts of the central nervous system, then one treatment the visible part of the tumor is not enough. Therefore, after the operation, the stage of non-surgical treatment begins. This stage consists of radiation therapy [radiation] and/or courses of chemotherapy [chemotherapy]. During chemotherapy courses, children receive drugs that block cell growth (cytostatics). The goal of this treatment is to stop the growth of cancer cells or destroy them. Radiation therapy is done using high-energy electromagnetic [electromagnetic] radiation. It is applied externally through the skin to the region that needs to be irradiated. The radiation destroys the DNA of cancer cells and they begin to die.
The decision on how exactly the child will be treated (what treatment methods the doctors will choose, how intense the courses of chemotherapy/radiation therapy will be) depends on the age of the patient, what specific type of tumor was found in the child, what molecular biological features the tumor has, and also depends on whether the child has metastases. In addition, they take into account whether it was possible to completely remove the tumor during the operation.
How are children with pineoblastoma of the brain treated?
Usually, after the maximum possible removal of the tumor, children over 4 years of age, in whom pineoblastoma has not had time to metastasize, receive radiation therapy to the entire central nervous system (in this case, doctors use the term craniospinal irradiation). And then they additionally irradiate the tumor region. After the radiation stage, children receive courses of so-called maintenance chemotherapy. They use several different cytostatics. If pineoblastoma has managed to metastasize, treatment becomes more intense. For example, radiation therapy is performed with a higher dose of radiation, and before it begins, the child additionally receives a course of so-called induction chemotherapy.
In children under 4 years of age, the development of brain tissue has not yet been fully completed. Therefore, doctors refuse radiation therapy or seek to postpone it to a later date in order to minimize the risks of serious long-term complications. Instead of this stage of treatment, children after surgery receive courses of chemotherapy consisting of several drugs. Some children may be given courses of high-dose chemotherapy [high-dose chemotherapy] to increase their chances of being cured of the disease. And after it, specialists perform an autologous bone marrow transplantation [autologous bone marrow transplantation].
How are children with other types of embryonal brain tumors treated?
New information has accumulated on other types of embryonal tumors of the central nervous system. Researchers were able to identify many new subgroups. Therefore, experts strive to individualize treatment, which is planned depending on the characteristics of each of these subgroups.
It is important to know: how exactly a particular child will be treated is decided by the attending physician after a detailed discussion with the sick person or his relatives.
Occipital transtentorial approach
There are two main modifications of this approach:
1) with exposure of only the posterior parts of the superior sagittal sinus and lateral displacement of the occipital lobe from the falx process;
2) with simultaneous exposure of the sagittal and transverse sinuses.
In the latter case, the occipital lobe rises above the tentorium of the cerebellum and moves laterally. From our point of view, in most cases there is no need to expose the transverse sinus, since retraction of the occipital lobe laterally from the falciform process allows for sufficiently wide exposure of the pineal region. Puncture and drainage of the lateral ventricle facilitates displacement of the occipital lobe.
The operation can be performed in a sitting position or in a lateral position - the so-called. pronation by 3/4.
Soft tissue incision
The occipital transtentorial approach is performed on the side of the non-dominant hemisphere. A horseshoe-shaped skin incision in the occipital region is made in such a way that trepanation exposes the posterior sections of the sagittal sinus for approximately 7-8 cm (Fig. 24). Following the incision of the soft tissues and skeletonization of the squama of the occipital bone, it becomes possible to accurately determine the midline, the landmark of which is the sagittal suture.
Fig.24. Schematic representations of the stages of the occipital transtentorial approach: a, b) general access schemes: c) osteoplastic trepanation in the right occipital region. The flap of soft tissue is folded down. The bone is cut out in such a way as to expose the superior sagittal sinus in its posterior third (1) and part of the sinus drainage (2).
The skin flap should be large enough to expose the sagittal and lambdoid sutures and the attachment of the cervical muscles to the squama of the occipital bone.
Trepanation
To ensure convenient surgical access and prevent excessive traction of the occipital lobe, it is necessary to perform trepanation as follows: the first two trephination holes are placed along the midsagittal line, 0.5 cm to the left of it.
The distance of these holes from the external occipital protrusion is 0.5-1 and 8-9 cm, respectively. Using bone cutters, the burr holes are expanded to the right above the sagittal sinus. This technique allows you to use a conductor or dissector to separate possible adhesions between the sinus and the bone, and also, under visual control, to pass the conductor of a Gigli file or trephine head over the sinus. The remaining two burr holes are superimposed at a distance of 5-6 cm to the right of the sagittal sinus, at the level of the previous holes (Fig. 25).
Fig.25. Tremanation window and proposed line of cut of the dura mater. The dura mater is sutured to the bone along the perimeter of the trepanation window. The arrow indicates the place of confluence of the superior sagittal sinus with the sinus drainage
.
A conductor and a saw are alternately inserted through the milling holes and the bone flap is cut out using the latter. In order to prevent blood loss during trephination, it is advisable to cut the bone over the sagittal sinus last, i.e. just before flap elevation.
If trepanation was performed using a pneumatic or electric trephine, then only the first two milling holes are superimposed. In this case, the holes can be placed over the sagittal sinus. Initially, using a trephine, a horseshoe-shaped cut is made between these holes in the squama of the occipital bone, and then a slightly curved cut is made to the left of the sinus.
Before raising the bone flap, it is necessary to have hemostatic agents and suture material ready in case of bleeding from the sinus. Typically, the bone in the projection of the superior sagittal sinus is quite tightly sealed to the dura mater, especially in elderly patients, as well as after shunt operations.
Therefore, fairly careful separation of the bone flap from the dura mater is required. For this purpose, first, using an elevator, the edge of the bone flap opposite to the sagittal sinus is slightly raised, under which a dissector is inserted and then the bone is slowly peeled off from the adjacent shell. The greatest care is required when separating the outer wall of the sagittal sinus from the bony structures.
In order to reduce blood loss after raising a bone flap, quick action by the surgeon is required, since quite intense bleeding can occur from the wall of the sagittal sinus and parasinus veins. After lifting the bone flap, the anesthesiologist compresses the jugular veins in the neck. This increases venous pressure and makes it possible to more accurately determine the location of the sinus. In addition, bleeding veins are identified, which can be a source of air embolism.
For the purpose of hemostasis, surgical hemostatic gauze or sponge is used, and the surface of the bone cut is lubricated with wax, regardless of whether there is bleeding from the diploic veins or not. After careful hemostasis, the dura mater around the perimeter of the trepanation window is sutured to the bone in order to prevent the formation of epidural hematomas in the postoperative period.
Dura section
Of the various proposed cut lines for the dura mater, from our point of view, the optimal one is a semi-oval cut with the base facing the sagittal sinus.
The line of incision of the membrane along the sagittal sinus proposed by some authors is impractical, since the risk of damage to the parasinus lacunae increases. A semi-oval incision of the dura mater is made with the base facing the sagittal sinus, while the ends of the incision of the dura mater are as close as possible to the sinus.
In case of damage to the sinus wall, the resulting small defect can be closed with hemostatic gauze or suture. The dura mater flap is retracted in the opposite direction using ligatures (Fig. 26).
Fig.26. Occipital transtentorial approach. The dura mater is dissected in an arcuate manner, with the base facing the superior sagittal sinus and folded in the opposite direction. A ventricular catheter was inserted into the right lateral ventricle.
In the case of hydrocephalically dilated ventricles of the brain, the posterior horn of the lateral ventricle is punctured and drained using a soft ventricular catheter. After removing the required amount of cerebrospinal fluid, brain relaxation is achieved. This creates optimal conditions for atraumatic abduction of the occipital lobe away from the falx process.
In cases where the ventricular system is not dilated or the removal of cerebrospinal fluid is not accompanied by the desired effect - sufficient relaxation of the brain, before traction of the occipital lobe, the patient is administered intravenous manitol at the rate of 0.5-0.75 g/kg or 40 mg of furosemide.
Veins passing from the hemisphere to the sagittal or transverse sinuses in the occipital region are usually absent, and existing parasagittal venous granulations are easily separated from the sinus wall.
The occipital lobe is displaced laterally, exposing the falciform process and the medial part of the tentorium cerebellum. Gradually, the spatula moves deeper into the gap until the free edge of the cerebellar tentorium opens (Fig. 27).
Fig.27. Occipital transtentorial approach. The occipital lobe is displaced laterally and slightly upward. The falxtentorial angle and structures of the pineal region are exposed: 1 - falxoid process, 2 - straight sinus, 3 - tentorium cerebellum, 4 - vein of Galen, 5 - splenium of the corpus callosum, 6 - internal vein, 7 - basal vein, 8 - tumor, 9 - medial surface of the occipital lobe, 10 - posterior medial villous artery.
This creates a fairly wide corridor for access to the pineal region along the falcus-stentorial angle. It must be remembered that the spatula applies pressure to the area of the calcarine groove, i.e. location of the cortical visual analyzer. For this reason, it is necessary to avoid rough traction of the brain to prevent the development of postoperative visual disturbances in the form of homonymous hemianopia. The purpose of surgical access, in addition to achieving maximum visibility of the tumor and adjacent nerve formations, is good visualization of the venous system of this area.
During tumor removal, every effort must be made to prevent damage to the functionally important venous trunks of this area. In case of damage to the walls of large veins, bleeding is stopped using hemostatic gauze or sponge. Coagulation of veins in such cases is dangerous, since it can lead to an increase in the defect in the vessel wall or its thrombosis.
The key step is to dissect the tentorium to achieve good exposure of the pineal region. This stage of the operation is carried out as follows: the tentorium is perforated with a long thin scalpel at a point located 0.5-1 cm lateral from the straight sinus and 2-3 cm posterior to the free edge of the notch of the cerebellar tentorium.
The cerebellar tentorium at the site of perforation is lifted with a blunt hook from the cerebellum adjacent below and dissected with scissors in the anterior direction to the free edge of the notch. The section line of the tentorium is parallel to the course of the straight sinus or goes at a slight angle outward (see Fig. 27). The flap thus formed, after coagulation of the edges of the incision, is moved to the falx using a ligature (Fig. 28). In order to prevent damage to the vein of Millet, excessive traction of the flap should be avoided.
Fig.28. Stages of removal of apaplastic astrocytoma tamponing the quadrigeminal cistern using an occipital transtaporial approach. The schematic image (b) shows the structures of the pineal region: 1 - vein of Galen, 2 - right basal vein, 3 - precentral cerebellar vein, 4 - branches of the posterior medial villous artery, 5 - tumor, 6 - cerebellum, 7 - internal occipital vein, 8 - cerebellar tentorium, 9 - cavity of the third ventricle and its left wall (10), 11 - quadrigeminal plate, 12 - dissected tentorium of the cerebellum. 13 - splenium of the corpus callosum. MRI and CT scan of the same patient before (d,e) and after (f) tumor removal.
Most authors believe that the length of the section of the cerebellar tentorium should be no more than 2-3 cm. C. Lapras recommends cutting the tentorium half its width, while WKClarck cuts the tentorium almost completely - to the transverse sinus. In our opinion, for optimal visualization of the pineal region, a 2-3 cm dissection of the tentorium is usually sufficient. If necessary, the incision can be increased
Sometimes between the leaves of the cerebellar tentorium there are large venous lacunae - parasines, some of which, as the cerebellar tentorium is dissected, have to be crossed. The resulting bleeding is stopped by coagulation, clipping or suturing the edges of the dura mater at the incision site. When choosing the location of the incision of the cerebellar tentorium, problems may arise if there are no clear boundaries between the falciform process and the tentorium.
This happens in cases where the cerebellar tentorium passes into the falcine process under an acute angle and the straight sinus is poorly differentiated. To avoid damage to the straight sinus and ampulla of the vein of Galen, it is important not to bring the cut line at the free edge of the tentorium closer to the straight sinus closer than one centimeter. After dissection of the cerebellar tentorium, the area of the quadrigeminal cistern is examined. When the tumor grows into the surrounding cistern, already at this stage the posterior pole of the tumor, covered by the arachnoid membrane, is clearly visible (Fig. 28).
In most cases, the arachnoid membrane of the quadrigeminal cistern is thickened and has the appearance of an opaque white membrane. To widely expose the pineal region, the arachnoid membrane of the quadrigeminal cistern is dissected, first at the apex of the vermis, then laterally on both sides above the dorsal surface of the midbrain. Near the veins, preparation of the arachnoid membrane must be done with great care.
After opening the arachnoid membrane, a rather large precentral cerebellar vein is exposed, which passes from the apex of the vermis to the ampulla of the vein of Galen. In rare cases, there may be not one, but several precentral veins. Dissection of the arachnoid membrane and intersection of the precentral vein provides fairly wide access to the formations of the pineal region. At this stage of the operation, the vein of galena, the right basal and medial occipital veins are widely exposed (Fig. 29, 30).
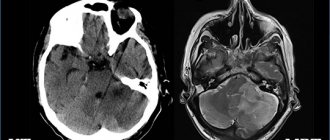
Fig.29. Removal of pineoblastoma using the occipital transtentorial approach. Intraoperative schematic representation (b) of the structures of the pineal region: the cerebellar tentorium is dissected and retracted with ligatures (1); the vein of Galen (2) and its main tributaries, the basal vein (3), are clearly visualized; internal occipital vein (4); precentral cerebellar vein (5); below the vein of Galen, the posterior pole of the tumor is visible (6); splenium of the corpus callosum (7); quadrigeminal plate (8). MRI before (d) and after (e) tumor removal.
Fig.30. Removal of germinoma of the pineal region using the occipital transtentorial approach. MRI before (a) and after removal (b,c) of the tumor. Postoperative MRI visualizes the zone of blood imbibition of the structures of the pineal region.
Figure 31 shows a case of subtotal removal of large pineoblastoma using an occipital transtentorial approach.
Fig.31. CT scan of a patient with large pineoblastoma before (a) and after (b,c) subtotal tumor removal using the occipital transtentorial approach.
Closing the surgical wound
After tightly suturing the dura mater, the bone flap is placed in place and secured with bone sutures. Soft tissues are sutured in layers. To prevent the formation of a subcutaneous hematoma, active drainage is left under the skin flap.