Definition
“Tethered spinal cord syndrome” is an adaptation of the English term “the tethered spinal cord syndrome” (Yamada S., 1981). “tether” in the original name , which literally means a leash for pets , is associated with the desire to most accurately reflect the essence of the pathological process it describes. It is the stretching of the spinal cord, which develops as a result of restriction of its mobility, that is, fixation, that leads to the negative impact and development of clinical manifestations of FSM.
Yamada, S. (Ed.). (2010). 3 Pathophysiology of Tethered Cord Syndrome. Tethered Cord Syndrome in Children and Adults. doi:10.1055/b-0034-80501
“tethered spinal cord” first used by Hoffman to describe the results of treatment of 31 patients suffering from pelvic disorders in combination with motor disorders and decreased sensitivity in the lower extremities. Symptoms in all patients regressed after excision of the thickened filum terminale. Based on the data obtained, the authors concluded that the pathological process develops as a result of stretching of the caudal parts of the spinal cord (Hoffman HJ, 1976).
Pathogenesis
It is known that the spinal cord is protected from excessive stretching by the so-called “dentate ligaments” , which fix the spinal cord in the lumen of the spinal canal (Tunituri AR, 1977). While at the level of the cervical and thoracic spine they are significantly developed (Breig A., 1970; Tubbs RS, 2001), at the level of the lumbar spine they are not , and stretching of the caudal parts of the spinal cord is prevented only by the elastic properties of the terminal filament (Tani S., 1991 ).
Yamada, S. (Ed.). (2010). 3 Pathophysiology of Tethered Cord Syndrome. Tethered Cord Syndrome in Children and Adults. doi:10.1055/b-0034-80501
When the terminal filament was stretched in patients with FSM, its elongation was observed by no more than 10%, while normally it elongates by 50% or more (De Vloo P., 2016). Light microscopy of a section of a pathologically altered filament terminale in patients with FSM revealed a predominance of fibrous tissue; when stained for elastin, its content was minimal (Hendson G., 2016). Based on the data obtained, it was hypothesized that SFSM develops as a result of tension in the caudal parts of the spinal cord between the last pair of odontoid ligaments and any inelastic structure that fixes it caudally (Yamada S., 1981).
Yamada, S. (Ed.). (2010). 3 Pathophysiology of Tethered Cord Syndrome. Tethered Cord Syndrome in Children and Adults. doi:10.1055/b-0034-80501
In 1981, S. Yamada, in an experiment on cats, demonstrated a slowdown in metabolism in the tissues of the caudal parts of the spinal cord during stretching and its subsequent restoration when the tension was removed. A few years later, in 1987, it was officially proposed that “tethered spinal cord syndrome” be considered a scientifically based clinical diagnosis (McLone D., 1987), from which point this term began to appear more and more often in the literature.
Currently, most domestic and foreign specialists characterize FMS as a combination of motor, sensory, trophic disorders in the lower extremities, as well as pelvic disorders and musculoskeletal deformities that develop as a result of immobilization and stretching of the caudal parts of the spinal cord in pathologies of the filum terminale (“tight filum”) terminale” – inelastic filum terminale, filum terminale lipoma, etc.), myelodysplasias (MMC, spinal lipomas), complex spinal dysraphisms (diastematomyelia, dermoid, epidermoid, enteric cysts, dermal sinus), as well as post-inflammatory and postoperative scar-proliferative changes terminal cistern (leptopachine meningitis, arachnoid cysts, etc.) (McLone DG, 1997; Iskandar BJ, 1998; Tortori–Donati P., 2000;).
The reasons for the development of FSM are most often the consequences of correction of spina bifida, as well as Spina Bifida Occulta
Bone Marrow Transplant Awareness
We conducted a survey of a group of potential donors (141 people) from different cities of Russia (St. Petersburg, Moscow, Orel, Kazan, etc.). The questionnaire consisted of 17 questions, 7 of which were constructed using the method of semantic potential by Charles Osgood.
As a result of the survey, the average awareness of citizens on the issue of the structure of the bone marrow and its functions was established: more than half of the respondents (71%, that is, 100 people) gave the correct definition of bone marrow, of which 43% of respondents most fully and correctly listed its functions (Fig. . 4).
Figure 4. Diagram of analysis of awareness of bone marrow and its functions.
The majority of respondents (95.3%) are aware of the existence of bone marrow donation to varying degrees (from awareness of the very fact of such an operation to information about many details of the process). People are aware of the problem thanks to the media (43.4% of respondents), social networks (50.4%) and close circle (friends, relatives) - 24%. Less than half of the respondents thought that by becoming a donor they could save a life (48.3%). More than half of the respondents (62.4%) (Fig. 5) would not donate bone marrow and do not know about the existence of a donor registry (65.4%). Respondents in most cases would not agree to donate bone marrow due to fear of pain (47%) and irreversible traumatic changes in their own health (56.7%).
Figure 5. Diagram of analysis of the number of potential bone marrow donors
Classification
It is obvious that a significant contribution to the development of clinical symptoms in spinal dysraphism , in addition to stretching, can be made by volumetric effects (compression), deformation, as well as congenital disorders of cyto- and angiomyeloarchitecture (Kumar R., 2010). Based on the concept of FSM as a reversible pathological condition, S. Yamada and DJ Won proposed to separate processes caused by limited mobility of the spinal cord (true FSM) and conditions that have clinical manifestations similar to FSM, which include in their pathogenesis, in addition to stretching, other unfavorable factors effects (compression, deformation, etc.), as well as pathologies that are not at all related to SFSM, caused mainly by disruption of the formation of the spinal cord and having an unfavorable prognosis for surgery aimed at eliminating the fixation of the spinal cord (Yamada S., 2007). The first category included patients with anomalies of the filum terminale , hernias of the sacral localization and small caudal lipomas, in which the main contribution to the pathogenesis of clinical manifestations is made by longitudinal stretch of the spinal cord. The second category includes patients with myelomeningocele of the lumbar spine, lipomyelocele and repeated scar fixation of the spinal cord. In these patients, obviously, only part of the symptoms presented relates to FMS and can regress after surgery. The third category of patients included children with spina bifida of the thoracic spine, accompanied by congenital paraplegia and incontinence (Yamada, 2007).
Classification of SFSM according to Yamada, Won 2007
In accordance with the described categories, expected results and indications for surgery were distributed. When fixation was eliminated in the first category of patients, a complete regression of symptoms , and patients from the third category have practically no chance of restoring lost functions (Liptak GS, 1995).
Epidemiology
Despite the fact that the true incidence of FMS is unknown, and the number of patients with classic FMS caused by anomalies of the filum terminale, according to some data, does not exceed 0.1% in the pediatric population (Bademci G., 2006), only in the USA during the period From 1993 to 2002, more than 9,000 operations were performed to eliminate spinal cord tethering (Lad SP, 2007).
SFM manifests itself during periods of accelerated child growth
According to most authors, FMS is characterized by a progressive course , while the age at which deterioration of the condition may occur varies from 8 months to 16 years and does not always correspond to periods of accelerated growth. It is noted that at older ages, the manifestation of FMS may be associated with physical activity or injury (Pang D., 1982)
During the first year of life, a child grows by an average of 20 cm due to lengthening of the body
Experimental data suggest that timely removal of fixation can lead to restoration of spinal cord function (Yamada S., 1981; Schneider SJ, 1993). However, it has been shown that sudden excessive stretching of the spinal cord can lead to irreversible structural changes (Kocak A., 1997). In this case, in contrast to gradual long-term stretching (Pfister BJ, 2004), the formation of a persistent neurological deficit is most likely due to rupture of the spinal cord pathways (Yamada S., 2003).
In this regard, concern is raised by the fact that children suffering from FMS often remain under the supervision of orthopedists and urologists for a long time without receiving appropriate neurosurgical treatment. This can lead to the formation of irreversible neurological and orthopedic deficits, as well as persistent pelvic disorders
Spinal cord injuries and consequences
The spinal canal is maximally protected from damage. This means that a simple fall and impact on the spine will not lead to serious damage. But there are a number of actions that can significantly paralyze the work of this department, and therefore the entire organism.
- Spinal fracture. This disorder leads to paralysis of those parts of the body that are located below the fracture. This is due to the fact that the spinal cord controls the functioning of those organs that are located at its level; accordingly, a violation of the integrity leads to a failure in the conduction of impulses.
- Numbness without visible disturbances. The spinal cord roots exit through the vertebral canals. Often, if the salt balance is incorrect, salts are deposited in these places, which leads to clogged passages. In this case, nerve fibers become pinched and conductivity decreases. This leads to the symptoms described.
- Constant pain in the spine. This is due to wear and tear of the intervertebral discs. This leads to pinching of nerve fibers. A “short circuit” occurs in the clamp area, which is the cause of constant discomfort.
Health depends on the condition of the spine and spinal cord, so if pain appears in this area, you should immediately consult a doctor. Serious spinal injuries can leave a person permanently confined to a wheelchair.
Clinical diagnosis
Timely detection of FSM at the stage of the disease when the pathological process is still reversible is facilitated by alertness regarding the presence of skin stigmas of dysembryogenesis and musculoskeletal deformities in newborns (Aldana PR, 2009).
Skin manifestations are detected in 40% of children with FSM. These include local hypertrichosis (“faun’s tail”), subcutaneous lipoma, cutaneous angioma, age spots, rudimentary skin growths in the lumbosacral region.
Skin “stigmas” of dysembryogenesis: hypertrichosis, subcutaneous lipoma, cutaneous angioma.
Congenital musculoskeletal deformities in the form of shortening, hypotrophy of the lower extremities, and foot deformities may attract attention Asymmetrical deformations are considered characteristic of FSM - “hollow”, equinovarus foot, “trigger-shaped” toes, etc. Although asymmetry of the lower extremities is often detected with FSM, pronounced hypotrophy of one of the lower extremities (“stork leg”) is rare (Lagae L., 1990 )
“External” manifestations of FSM in children
FSM is manifested by progressive pelvic disorders (incontinence or retention of urine and feces). Parents may experience constant leakage in the child, as well as frequent constipation or episodes of stool.
At an older age, you can find out whether the gait has changed, whether awkwardness has appeared when walking or running, whether the sole of the shoe has changed over time, in which direction it has become thinner (outward or inward) (Elikbaev G.M., 2008). There may be pain when turning the body, flexing or extending. In pre-adolescence, the main clinical manifestations of FMS are weakness in the legs, gait disturbances, urinary incontinence, and newly developed foot deformities (Yamada S., 2004).
Clinical symptoms of FSM
Adolescents with FSM are characterized by progressive scoliotic deformity of the spine, as well as urinary incontinence, mainly in the form of episodes of gelastic incontinence, often interpreted as a manifestation of a urinary tract infection.
During periods of accelerated growth, spinal deformity may be the main complaint (Trivedi J., 2002). In this case, the development of deformation of one of the feet (hollow foot, clubfoot) on the side opposite to the arch of scoliosis, with a high degree of probability, should be interpreted as a manifestation of FSM (Yamada S., 2001).
When assessing neurological examination data, it is noted that FMS most often occurs in the form of asymmetrical, uneven sensory and motor disturbances, accompanied by a decrease in tendon reflexes, as well as pelvic disorders of a mixed type (Yamada S., 2004). However, in some cases, gross trophic disorders may be detected, accompanied by a violation of the integrity of the skin - trophic ulcers (Nikolaev S.N., 1996; Brand N., 1996).
Disorders of the function of the pelvic organs are detected in 40% of patients with FMS, being its only clinical manifestation in 4% of cases (Prityko A.G., 1997; Metcalfe PD, 2006). The majority of patients with FMS show signs of bladder detrusor hypotension due to damage to the parasympathetic micturition center. Depending on the degree of preservation of urethral resistance, pelvic disorders in them occur in the form of constant or periodic urinary incontinence with the accumulation of varying volumes of residual urine, which in some cases requires catheterization of the bladder (Khachatryan V.A., 2009). Most often, such urodynamic disorders are accompanied by chronic constipation and stool loss due to decreased tone of the rectal sphincters (Kayaba H., 2003).
A decrease in the volume of filling of the bladder against the background of an increase in the tone of its muscles is observed less frequently and may be a consequence of damage to the spinal cord above the level of the conus. In this case, there is a disconnection of the structures of the segmental apparatus and supraspinal centers. Hyperexcitability of the detrusor, manifested clinically in the form of imperative, false urges, is caused by irritation of the bladder wall while maintaining a sufficient number of functioning neurons of the parasympathetic sacral center. Often, in children with FSM, against the background of urodynamic disorders signs of chronic urinary tract infection , vesicoureteral reflux and ureterohydronephrosis are revealed (Elikbaev G.M., 2008).
Thus, the clinical diagnosis of FSM is based on the identification of skin stigmas of dysembryogenesis, musculoskeletal deformities, weakness, sensory disturbances in the lower extremities, as well as pelvic disorders.
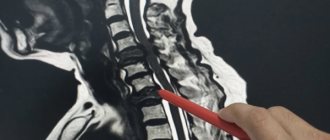
Instrumental diagnostics
Currently, MRI has almost completely replaced SCT myelography from the diagnosis of FMS, leaving ultrasound as a useful diagnostic method in newborns. Along with this, it is believed that the selection of candidates even for this non-invasive study should be based on a thorough clinical examination.
Previously, it was believed that all children with FSM have spina bifida (Boone D., 1985), but modern studies show that FSM also occurs in the absence of spina bifida (Ackerman LL, 2003). Thus, despite the fact that the occurrence of spina bifida occulta in the population is about 22%, only a small part of them have FSM (Nejat F., 2008).
It is known that during the period of intrauterine development, the growth of the spinal column outstrips the increase in the length of the spinal cord, forming a difference in length and a higher end of the spinal cord. The difference in their length increases most actively from the 12th to the 20th week of gestation, slowing down subsequently (Zalel Y., 2006).
It was previously believed that in newborns the spinal cord ends at the level of the L2-L3 vertebral disc, and then migrates cranially and reaches the level of the L1-L2 vertebrae by two months (Barson AJ, 1970). Subsequent studies showed that in most cases it ends at the level of the L2 vertebrae at birth (Wolf S., 1992; Robbin ML, 1994; Hill CA, 1995).
The level of the end of the spinal cord can normally vary from the middle of Th12 to the middle of the L3 vertebra, but in 94-98% of cases it is above the level of the L2-L3 vertebral disc (Reimann AF, 1944). Taking these data into account, the idea was formed that when the conus of the spinal cord is located below the level of the L2 vertebra, we can talk about radiological signs of SFSM. However, a low position of the conus spinal cord can be observed in some healthy newborns (Hughes JA, 2003; Thakur NH, 2011), and FSM can develop even with a normal position of the conus spinal cord (Warder DE, 1993).
Low location of the conus of the spinal cord in various forms of spinal dysraphism
End thread
Normally, the spinal cord ends in a filum terminale, which is a fibrovascular cord of parallel collagen bundles connected by a transverse network of collagen and elastin fibers and capillaries located between them (Fontes et al 2006). The diameter of the terminal filament normally ranges from 1.1 to 1.2 mm (Yundt KD, 1997). When its thickness is more than 2 mm, it was proposed to consider the diagnosis of FSM justified.
The filum terminale of the spinal cord is normal (left) and pathological (right)
However, thickening of the filum terminale, as it turned out later, is not a prerequisite for the development of FSM (Pinto FC, 2002), and its clinical manifestations can develop with a smaller diameter of the filum terminale (Nkhazar GB, 1995; Selden NR, 2006). Also, fatty infiltration of the filum terminale, which is normally detected in 5.8% of subjects (McLendon RE, 1988), is not a mandatory sign of the presence of FSM.
When fixing the spinal cord, the filum terminale is most often located behind the roots of the cauda equina, and the spinal cord is deviated posteriorly and adjacent to the arachnoid membrane (Fitz CR, 1975).
The tensioned final thread (indicated by the arrow) fits tightly from the inside to the thinned dura mater
As methods of additional differential diagnosis, MRI in the prone position, as well as standing with the torso flexed and extended (functional MRI), was proposed, but so far they have not become widespread (Levy LM, 1988; Zamani AA, 1998; Witkamp T.D., 2001; Niggemann P., 2011; Singh S., 2012).
In the prone position (image on the right), the dorsal deviation of the conus and filum terminale of the spinal cord remains.
The experience of performing DWI tractography in patients with FSM allowed us to assume its role in terms of differential diagnosis of spinal cord structures and scar tissue, and also allowed us to put forward the assumption that, based on the indicators of fractional anisotropy, one can judge the degree of preservation of the spinal cord conductors and evaluate the prognosis of surgical treatment of FSM (Filippi CG, 2010).
DWI tractography of the spinal cord and cauda equina roots (right)
Thus, none of the previously proposed neuroimaging criteria for diagnosing FMS is currently absolute.
Data from electrophysiological examination methods are also not believed to be of decisive importance in the diagnosis of FMS (Yamada S., 2007). In particular, the study of somatosensory evoked potentials (SSEPs) and motor evoked potentials (MEPs) in children is often uninformative, and the traditionally considered electroneuromyogram (ENMG) patterns, despite the identified clinical picture of SPS, may be within normal limits (Gusev A.R., 1990) . It is reported that registration of SSEPs from the tibial nerves can be used as a screening method of examination, as well as to assess the long-term results of surgical treatment of SSEP in adults (Li V., 1996; Kale SS, 1998).
It should be noted that many authors point to the importance of urodynamic examination data in diagnosing FMS, including in cases of relapse of spinal cord fixation (Meyrat BJ, 2003; Metcalfe PD, 2006; Rendeli C., 2007; Maher CO, 2009).
Anatomical features
A rather thick tourniquet, white in color, located in the spinal canal - this is the human spinal cord. Its diameter is about 1-1.5 cm, and its length almost reaches half a meter (up to 45 cm). This organ weighs about 38 g.
The narrow spinal canal is not only the location of an important organ, but also its protection. The core of the organ consists of a gray substance
It is covered by a white substance, which is also covered with protective and nourishing shells for the core. This is the general plan of the structure of the spinal cord.
Topography
The structure and functions of the spinal cord are quite complex. Neurosurgeon students study it in detail. Experts very carefully consider the development of the spinal cord. Ordinary people are interested in the question of what its topography is and familiarity with the leading role of this organ.
So, it is quite simple to describe the essence and goals that this body serves. The cervical spinal cord at the level of the back of the head in the area of the foramen passes into the cerebellum. The spinal cord ends at the level of the first 2 lumbar vertebrae. The conus spinal cord is located where a pair of vertebrae are located in the lumbar region. Next is the well-known “terminal thread”.
But this fragment is considered atrophied. It is called the “end” region. Nerve endings called “roots” are distributed along the entire circumference of the thread. The filum terminale is equipped with a substance containing a small proportion of nervous system tissue. But the outer part is not even equipped with a similar fabric.
The topography of the organ includes a pair of thickenings where the innervating processes emerge (cervical thickening of the spinal cord and lumbar). The outer and rear surfaces of the bundle are separated by slits called “middle”. The one in front is deeper, the back one is smoothed.
External structure
The general structure of the spinal cord suggests its division into a number of surfaces: posterior, anterior and two lateral. The spinal cord has faint grooves on the lateral surface. They are located longitudinally, and nerves extend from the grooves. They are also called “roots”. In the lumbar area, together with the terminal filament, they form a tail, which is commonly called a horse's tail. The grooves divide half of this cord into the following structures:
- front;
- lateral;
- posterior (cords).
The grooves of the spinal cord extend along the canal. The roots are divided into anterior ones - they are formed by efferent neurons, and posterior ones, created by afferent neurons. Their bodies converge into a knot. The roots unite and form a nerve. So, on all sides of the tourniquet there are over 30 nerve endings, forming exactly the same number of pairs. This is the external structure of the spinal cord.
White matter
All cords are made entirely of white matter of the spinal cord. They consist of longitudinal nerve fibers. These threads converge, forming peculiar conductors. Based on their functional purpose, fibers are divided into 3 types:
- motor;
- associative;
- sensitive.
The first are represented by short bundles and combine all parts into a single system. The second ones are called ascending. They give signals to the centers. Still others are descending. They provide signals from central structures to areas of the horns.
Gray matter
It structurally resembles grouped longitudinal plates consisting of homogeneous neurons. It contains not only neuronal bodies, but also neuropil, glial cells and capillaries. Along the entire spine it forms 2 columnar types, left and right. They are connected by gray adhesions.
The anterior horns contain the largest neurons. They form the motor nuclei of the spinal cord and inhibitory neurons. The structure of the gray matter of the background horns is not the same. It contains a huge number of intercalary type neurons.
The lateral horns of the spinal cord fill the centers of the ANS, the dilation of the pupil, the bases of innervation of the digestive system and other important organs of the human body. In the nucleus of the gray matter of the spinal cord there is a canal that neurosurgeons call “central.” It is filled with liquor. In adults, in some places it is filled with cerebrospinal fluid, and in others it is overgrown.
Shells
Anatomy of the spinal cord describes the membranes of the spinal cord:
- vascular soft;
- hard;
- avascular or arachnoid.
The characteristics of shell 1 are as follows: soft, penetrated by vessels and nerves. It is enveloped by the avascular part. There is some space here called “subarachnoid”. The cerebrospinal fluid generated in one of the systems flows into this niche. The last shell is made up of connective tissue; it is strong and flexible. The membranes of the spinal cord and brain are identical and form a single structure.
From the editor: Methods of treating schizophrenia
Surgery
The polyetiology of FSM, according to a number of experts, often leads to an unreasonable expansion of indications for its surgical treatment (Kulkarni AV, 2004). In this regard, the indications for surgery were proposed to be considered justified with a combination of characteristic radiological and clinical manifestations of FMS and the progressive course of the disease (Drake JM, 2007; Wykes V., 2012). Along with this, most researchers note the predominantly reversible nature of the changes during early correction of SFM (Yamada S., 2007) and the rare improvement in condition after surgery in patients with long-term symptoms (McLone D., 1997; Iskandar BJ, 1998; Haro H., 2004; Hajnovic L., 2007). It should also be noted that in patients considered “asymptomatic”, signs of the development of FMS may include undiagnosed changes in gait, scoliosis, as well as urodynamic disorders that occur under the guise of a chronic urinary tract infection (Sanchez T., 2014).
Previously considered appropriate expectant management was apparently due to the risk of general anesthesia, as well as the conditions of manipulation on the relatively small and seemingly more vulnerable structures of the spinal cord in children. The development of anesthesia, microsurgical equipment and intraoperative neurophysiological monitoring, of course, made it possible to successfully perform surgical interventions at any age immediately after introscopic verification of pathology, even with an asymptomatic course of the disease (Hoffman HJ, 1985; Tamaki N., 1988; Kanev PN, 1990; Koyanagi I., 1997; Schoenmakers MA, 2003; George TM, 2005; Rinaldi F., 2005). Thus, at present, an idea has formed about the advisability of early preventive surgical treatment of FSM, aimed at preventing possible irreversible damage to the spinal cord. It seems especially relevant to eliminate fixation in adolescents before the onset of a period of accelerated growth.
Surgical treatment of FSM consists of eliminating caudally located fixation factors, in particular: pathologically altered filament terminalis (fatty degeneration, thickening, shortening, decreased elasticity), pathological formations of the spinal canal (lipoma, dermoid, dermal sinus, bone, fibrous, septum), and also cicatricial and arachnoid adhesions (Caldarelli M., 2013):
Transplantation of a pathologically altered filament terminale
Removal of conus lipoma
Dermoid cyst removal
Elimination of diastematomyelia
Preference is given to “organ-saving” techniques - laminotomy, microsurgical techniques. As additional options, a number of authors report the effectiveness of using a CO2 laser and an ultrasound aspirator for tissue dissection, indicating minimal energy dispersion and minor traumatic effects of laser and ultrasound compared to traditional methods (McLone DG, 1986; Browd SR, 2009), as well as the feasibility of intraoperative neurophysiological monitoring (Sala F., 2002).
Operating room view Operating microscope
Hypoglossal nerve (XII) - Anterior branch
1.
HYPOGLOUS NERVE (XII)
, n. hypoglossus. Twelfth cranial nerve. It leaves the brain through numerous roots between the pyramid and the olive, passes through the canal of the same name and descends between the internal jugular vein and the internal carotid artery. Above the posterior edge, the m.mylohyoideus enters the muscles of the tongue. Rice. B.
2.
Lingual branches
, rami linguales. They arise from the trunk of the hypoglossal nerve and innervate the stylohyoid, hypoglossus and genioglossus muscles, as well as the muscles lying inside the tongue. Rice. B.
3.
Radicular threads
, fila radicularia. They emerge from the spinal cord and join into bundles that form the anterior and posterior roots of the spinal nerve. Rice. A.
5.
Anterior root (motor)
, radix anterior (motoria). Contains axons of neurons in the anterior and lateral columns of the gray matter of the spinal cord. Rice. A.
6.
Spinal (sensitive) node
, ganglion spinale (sensorium). Located in the intervertebral foramen as part of the dorsal root near the junction with the radix anterior. Consists of pseudounipolar neurons. Rice. A.
8.
Spinal nerve trunk
, truncus nervi spinalis. It starts from the junction of the anterior and posterior roots and continues to the level of origin of the first branch. Rice. A, Fig. IN.
9.
Anterior branch
, ramus anterior. The largest branch of the spinal nerve. Connecting with the anterior branches of adjacent spinal nerves it forms plexuses. The anterior branches of the thoracic nerves are called intercostal nerves. Rice. A.
From the editor: Causes, diagnosis and treatment of occipital neuralgia
10.
, ramus posterior. A smaller branch of the spinal nerve, compared to the anterior one, which innervates the skin and autochthonous muscles of the back. Rice. A.
11.
Meningeal branch
, ramus meningeus. Contains sensory and sympathetic fibers. It passes in front of the spinal nerve, enters the spinal canal through the intervertebral foramen and, together with other meningeal branches, forms a plexus that innervates the membranes of the spinal cord. Rice. A.
13.
Ponytail
, cauda equina. It is formed by the roots of the caudal spinal nerves (starting from the 1st and 2nd lumbar) and the filum terminale. Rice. IN.
14.
Medial branch
, ramus medialis. Each of them begins from the posterior branch of the corresponding spinal nerve. Contains motor and sensory fibers. Rice. A.
17.
Suboccipital nerve
, n. suboccipitalis. Posterior branch of the 1st cervical spinal nerve. Passes between the vertebral artery and the posterior arch of the atlas, innervates the short suboccipital muscles. Rice. G.
19.
Greater occipital nerve
, n. occipitalis major. Posterior branch of the 2nd cervical spinal nerve. First it passes between the axial vertebra and the inferior oblique muscle of the capitis, then pierces the trapezius muscle and goes to the semispinalis capitis muscle and the skin of the back of the head. Rice. G.
20.
Third occipital nerve
, n. occipitalis tertius. Posterior branch of the 3rd cervical spinal nerve. Innervates the skin of the posterior neck near the midline. Rice. G.
21.
CERVICAL PLEXUS
, plexus cervicalis. Formed by the anterior branches of the first four cervical spinal nerves (C 1 - 4). Innervates the skin and muscles of the neck.
23.
Cervical (hyoid) loop
, ansa cervicalis (hypoglossi). It consists of fibers from the hypoglossal nerve and the first three cervical spinal nerves. Innervates the hypoglossal muscles. Rice. B.
24.
Anterior root
, radix anterior. It arises from the hypoglossal nerve and contains efferent fibers of the first to third segments of the spinal cord. Rice. B.
25.
Lesser occipital nerve
, n. occipitalis minor. The most superior cutaneous branch. It rises along the posterior edge of the sternocleidomastoid muscle to the skin of the back of the head, lateral to the n.occipitalis mayor. Rice. G.
28.
Greater auricular nerve
, n. auricularis magnus. It crosses vertically the middle of the sternocleidomastoid muscle and goes to the auricle. Rice. G.
29.
Anterior branch
, ramus anterior. Innervates the skin over the parotid gland between the anterior surface of the auricle and the angle of the lower jaw. Rice. G.
Intraoperative neurophysiological monitoring
Due to the fact that the incidence of neurological loss during surgical treatment of FSM is on average 10.9% (Choux M., 1994), various methods of intraoperative neurophysiological monitoring aimed at identifying and assessing the function of excitable conductive structures ( roots) of the spinal cord . For this purpose, we combined registration of somatosensory, motor evoked potentials, bulbocavernosus reflex, as well as electromyography (free-run EMG) and stimulation electroneuromyography (DNS) from the muscles of the lower extremities and the external sphincter of the rectum. According to the literature, monitoring of evoked motor potentials in combination with stimulation electroneuromyography demonstrated the greatest information content (Paradiso G., 2006).
Multimodal intraoperative neurophysiological monitoring
Features of neurophysiological monitoring in children with FMS are due to impaired formation and immaturity of the spinal cord, as well as its stretching, deformation and ischemia. Against this background, registration of evoked potentials and the bulbocavity reflex is extremely difficult (Rodi Z., 2001), and the main method of neuromonitoring remains stimulation electroneuromyography, with the goal of electrical stimulation mapping of the spinal cord roots (ESC) (Deletis V., 1992).
Electrical stimulation mapping of the spinal cord roots
Despite the known threshold current values for the anterior and dorsal roots of the spinal cord, their values for functionally significant structures in conditions of spinal cord malformations have not yet been established. Analogies with the results of studies in which, when stimulating the filum terminale, the voltage required for a muscle response exceeded that when stimulating the motor root by 100 times (von Koch CS, 2002), it was not possible to draw, since when the root is involved in a mass of adipose tissue or scar the magnitude of the threshold irritation can increase significantly. This is believed to be due to excitation dissipation or partial loss of conductive properties by the spine.
How do you find a bone marrow donor today?
World practice has shown that it is better to store data on HLA-typed donors in the form of a single information base. The World Marrow Donor Association registry contains data from 37 million volunteers from 55 countries.
The formation of the RDKM (bone marrow donor registry) in Russia is just beginning to gain momentum. For example, Rusfond together with the First St. Petersburg State Medical University. Academician Pavlov created a database of bone marrow donors. The register was named after Vasya Perevoshchikov, a patient who died of leukemia at the age of nine due to the lack of a donor. Today there are 40,258 potential donors in the registry. However, there is no register that unites all cities in Russia, which complicates the search for a donor throughout the country. The database is scattered across cities and institutions, so the chance of meeting a genetically suitable donor is 1:10,000.
Turning to foreign registers is not always possible, since the donation procedure from a foreign citizen can cost about 20–50 thousand dollars. In addition, due to the multivariance of genotypes (associated, for example, with the multinationality of Russia), the search for a donor may end in failure, because a person matching the HLA type will not be found.
As a result, in 20–40% of cases, searches in European registers end in failure.
“There is no general database of bone marrow donors in Russia,” comments Viktor Andronov, Honored Donor of Russia, founder of the Energy of Life movement. “They communicate with each other, exchanging data, but not all are friends. The problem is that we still do not have a legislative framework - there is no law on bone marrow donation. The Rusfond organization has created a large donor base, which is now the most promising in the country.
In addition to the lack of an all-Russian register, the problem is the lack of awareness of people. Many people confuse the bone cord with the spinal cord, believe that the procedure is painful, and sometimes do not know about donation at all.
Ideally, everyone should be on the register. We should live by the slogan: “Everyone helps everyone.” In the context of coronavirus, this is extremely important, because... It’s very difficult for us and foreign donors during this period.
The number of donors in the registry is a matter of national security and the index of human responsiveness.”
The creation of a single registry is a solution to problems with transplantation, since it will reduce the cost of finding and activating a donor, which will increase the life chances of those in need of a transplant.
People will be saved by responsiveness and involvement in a common cause. Donation can unite against the common problem associated with serious diseases. Bone marrow transplantation is a chance for life.
Latent tethered spinal cord syndrome
One of the pressing problems of pediatric neurosurgery is the choice of optimal treatment tactics for latent tethered spinal cord syndrome, in which, despite the characteristic clinical picture of FMS, there are no such criteria as low location of the spinal cord conus (below the level of the L2 vertebral body), as well as thickening ( more than 2mm in diameter) and/or shortening of the terminal thread
Patient with hidden SFM, conus spinal cord at the L1 vertebral level
Considering that the observational groups of latent FSM described in the literature are relatively small, to date there has been no consensus regarding the optimal treatment tactics for this pathology. Most experts point to the advisability of excision of the terminal filament and provide data on the high effectiveness of this manipulation, while a number of authors, on the contrary, express doubts about the existence of sufficient indications for surgical intervention. Their skepticism is based, among other things, on the fact that urinary disorders in children, which is considered the most characteristic sign of latent FMS, are associated with stretching of the conus of the spinal cord in no more than 1.5% of cases, and its true causes are other pathologies.
When the torso is flexed, the height of the spinal canal increases by more than 7%. In this case, damping of the longitudinal tension transmitted to the spinal cord is ensured due to the elastic properties of the final thread, caused by a balanced combination of elastin, collagen and reticular fibers. One of the possible reasons for the development of latent FSM is considered to be invasion of adipose tissue, sclerosis and dystrophic changes, as a result of which the elasticity of the terminal filament decreases. With insufficient compensation for stretching, it is transmitted to the caudal parts of the spinal cord, and with a further increase in vertebromedullary disproportion, it spreads to the higher segments of the spinal cord. The formation of a detailed clinical picture of FMS can take a long period of time and be remitting in nature against the background of periods of slowed growth and reflex limitation of motor activity, while some of the formed motor, sensory or orthopedic deficits may be irreversible. It is obvious that early diagnosis and timely correction of latent FSM has a significant impact on the prognosis of the disease. In the case of a combination of pelvic disorders and/or pain syndrome that are resistant to drug therapy, as well as in the presence of characteristic neurological and orthopedic disorders in children with spina bifida occulta, in our opinion, there are indications for excision of the filum terminale, even with a normal location of the caudal parts of the spinal cord.
Electrostimulation identification and intersection of the tense terminal filament with hidden SFSM
What functions does the circulatory system perform?
Stable blood circulation is necessary for every body. Blood performs many different functions:
- Transport (associated with the transfer of various substances). Includes a number of private functions, which include:
- respiratory - transfer of gases (oxygen and carbon dioxide) both in dissolved and chemically bound states;
- trophic - transfer of nutrients from areas of their absorption and accumulation to tissues;
- excretory - removal of metabolic products from tissues and their release from the body (with urine formed in the kidneys as a blood filtrate);
- regulatory - transfer of hormones, growth factors and other biologically active substances that regulate various functions to cells of different tissues; distribution of heat between organs and its release into the external environment (thermoregulatory function).
- Homeostatic (associated with maintaining a constant internal environment of the body, including acid-base and osmotic balance, water balance, body temperature, biochemical composition of tissue fluids, etc.).
- Protective (associated with the neutralization of foreign antigens, neutralization of microorganisms by various immune mechanisms) [3].
Blood can perform such a wide variety of functions due to the unusualness of its histological structure: (1) formed elements (erythrocytes, leukocytes and platelets) and (2) plasma (Fig. 3). The source of formed elements is bone marrow. Most of the cell pool is formed by red bone marrow, the rest by yellow bone marrow. [4].
Figure 3. Diagram of a blood vessel with formed elements
[5]
Results and forecast
It is believed that surgical treatment of FSM allows to achieve improvement or stabilization of the condition of 70-80% of patients (Herman JM, 1993; Sarwark JF, 1996; Koyanagi I., 1997; Sharif S., 1997; Lee GY, 2006; Lad SP, 2007; Bowman RM, 2009; Ostling LR, 2012). According to various data, pain syndrome regresses in most cases (Maher CO, 2007; Bowman RM, 2009; Romagna A., 2013), while improvement in motor function is observed in no more than 80% of patients. According to JM Herman et al., within a period of up to 4 years after surgery, the condition of 93% of children operated on for MMC and 100% of children operated on for spinal lipomas improved or stabilized (Herman JM, 1993).
Short-term and long-term results of surgical treatment of children with FMS at the Pediatric Neurosurgery Clinic of the Russian Scientific Research Institute named after. prof. A.L. Polenova
A decrease in spinal deformity as a result of correction of the spinal spinal cord is observed in 20-50% of cases, and its stabilization in 10-20% (Herman JM, 1993; Bowman RM, 2001). At the same time, it has been noted that when the Cobb angle of deformation is more than 40°, eliminating fixation, as a rule, does not lead to improvement (Pierz K., 2000; McGirt MJ, 2009). There are also descriptions of observations in which scoliosis progresses in patients with MMC at the level of the thoracic spine, despite the elimination of fixation (Reigel DH, 1994).
Regarding the function of the pelvic organs, the authors’ data differ significantly. Their improvement is reported (in 30-60% of cases), including after repeated interventions (Herman JM, 1993; Bowman RM, 2001; Metcalfe PD, 2006; Tarcan T., 2006; Abrahamsson, K., 2007; Maher CO, 2009), and about the absence of changes compared to the preoperative level (Fone PD, 1997). Improvement in capacitance characteristics is most expected in patients with urodynamic disorders such as an “overactive” bladder (Khoury AE, 1990; Nogueira M., 2004; Guerra LA, 2006).
The development or increase in neurological deficit after surgery has been established, according to various sources, in 9.5-35% of cases, more often with repeated interventions (Herman JM, 1993; Albright AL, 1999; Wang B., 2002). We are mainly talking about urological complications (2.2%) (Lad SP, 2007). O are less common than other undesirable consequences of surgery (cerebrospinal fluid leak, meningitis, etc.) (Cochrane DD, 1998; Al-Holou WN, 2009; Bowman RM, 2009;) and are most expected during repeated interventions (Maher CO, 2007). The development of postoperative wound complications is most expected in patients operated on for myelomeningocele, which is apparently due to impaired soft tissue trophism and unsatisfactory wound consolidation. The likelihood of meningitis increases significantly with the formation of a cerebrospinal fluid fistula. When detecting liquorrhea in these patients, hydrocephalus or shunt dysfunction should first be excluded (Rostotskaya V.I., 1962; Orlov Yu.A., 1993; Khachatryan V.A., 1995; Hudgins RJ, 2004). Other complications include failure of the sutures and dehiscence of the surgical wound, which occur in 7-10% of cases (Bowman RM, 2009).
Why do people need bone marrow?
The bone marrow is one of the central organs of both the circulatory and immune systems [5]. As noted earlier, it contains hematopoietic stem cells that are capable of differentiating into various blood cells, for example, red blood cells, macrophages or T-lymphocytes.
The occurrence of pathologies of this organ leads to a decrease in the efficiency of its activity, which leads to a deterioration in the performance of the immune and circulatory systems. The human body becomes more vulnerable. There is a need for transplantation of donor material.
Violation of the integrity of the bone marrow can occur, for example, during the treatment of cancer. Due to the use of chemotherapy and radiation therapy, cancer cells are destroyed, but along with them, other actively dividing cells of the body, including components of the bone marrow. The body loses the ability to produce blood cells.
Without a bone marrow transplant, such treatment can often do more harm than good, as it ultimately leads to serious disruptions in the functioning of the entire body. People with leukemia, aplastic anemia, malignant lymphomas, autoimmune diseases, etc. need transplantation.
Repeated (recurrent, scar) fixation of the spinal cord
Clinical manifestations of FSM, detected after surgery aimed at eliminating spinal cord fixation, are associated with its re-fixation (Inoue HK, 1994; Colak A., 1998; Ohe N., 2000; Blount JP, 2007; Al-Holou WN, 2009; Yong R.L., 2011; Caldarelli M., 2013). According to the literature, the clinical and neuroimaging (MRI) picture of relapse of spinal cord fixation can develop in 5-50% of operated patients, while reoperation may be required in 30% of them (Herman JM, 1993; Filler AG, 1995; Archibeck MJ, 1997 ; Kang JK, 2003; Morimoto K., 2005; Ogiwara H., 2011).
The main reason for the development of re-fixation is considered to be a local violation of the circulation of cerebrospinal fluid (Kang JK, 2003). This is indirectly confirmed by the high frequency of relapse of fixation after repair of spina bifida and lipomyelocele and relatively low for other anomalies (Caldarelli M., 2013). Apparently, the size and shape of the spinal cord (neural placode), the residual volume of tumor (fatty) tissue, as well as the narrowing of the spinal canal in the anteroposterior direction do not always allow restoration of the spinal cord membranes with the formation of a sufficient volume of subarachnoid spaces for adequate circulation of cerebrospinal fluid in the terminal cistern (Hudgins RJ, 2004), as a result of which the spinal cord fuses with the membranes, and sometimes with scarred soft tissues, spreading beyond the dural sac and even the spinal canal (Caldarelli M., 1995).
Relapse of spinal cord tethering is the second most common cause of deterioration in the condition of patients with myelomeningocele , with a progressive deterioration of 60% of them observed during a follow-up period of up to 5 years (Phuong LK, 2002; Talamonti G., 2007). It is noted that with incomplete elimination of fixation, the relapse rate can reach 80% (Huttmann S., 2001), while in 10% of cases three or more operations may be required to stabilize the condition of patients (Al-Holou WN, 2009; Maher CO, 2007, 2009). According to research results, an increase in the detection of relapse of FSM occurs at ages from 2 to 4 and from 8 to 11 years, regardless of the primary pathology (Herman JM, 1993; Caldarelli M., 1995).
Considering that surgical intervention at the initial stages of the pathological process, according to various authors, leads to improved treatment results, it was proposed to consider a progressive deterioration in the child’s condition or the appearance of new symptoms as indications for surgery . (Bowman RM, 2001; George TM, 2005). Along with this, making a decision about surgical treatment is extremely difficult in chronically “symptomatic” patients with persistent neurological deficits. At the same time, emphasis is placed on the need to exclude other causes of deterioration of the patient’s condition, such as shunt dysfunction, Chiari malformation, syringomyelia, etc. (Bowman RM, 2001; Talamonti G., 2007). It is emphasized that relapse of FMS can occur with erased, slowly progressing symptoms, which also complicates the recognition of the pathological process and is the reason for its late diagnosis . It is reported that the most common clinical manifestation in older age is progressive spinal deformity (Carstens C., 1996). However, other signs are fair to consider contractures of the lower extremities, deterioration of gait, and back pain (Herman JM, 1993; Bowman RM, 2009). Thus, the clinical picture of recurrent FSM is in many ways similar to that of primary FSM. At the same time, the onset of the disease is often associated with pain, and the deterioration of the condition with progressive spinal deformation (Caldarelli M., 1995).
Surgical treatment for re-fixation of the spinal cord is aimed at eliminating tension and deformation of the spinal cord and roots, as well as restoring cerebrospinal fluid circulation in the fixation area.
Elimination of scar fixation of the spinal cord
The area of scar adhesions during re-fixation may depend on the method of wound closure during primary intervention (Caldarelli M., 2013). In cases where neural tube reconstruction was performed during the primary operation, the scar is usually located in the midplane over a limited area (Caldarelli M., 2013).
Thus, the main measure to prevent re-fixation of the spinal cord during surgical correction of MMC and spinal lipomas is considered to be reconstruction of the neural placode (Pang D., 2010; Talamonti G., 2007). Expanding plastic surgery of the dura mater with various artificial substitutes is also used (Inoue HK, 1994; Ohe N., 2000). In addition, after surgery, bed rest in a prone position is recommended in order to avoid gravitational contact of the spinal cord with the dura mater.
Filum terminale of the spinal cord
The same banned issue for which Ernst fired Malakhov!
Joints and cartilage will be cured in 14 days with the help of ordinary...
The spinal cord is a cylindrical, elongated cord with a narrow central canal inside. Its outer shell, as in all parts of the central nervous system, has three layers - experts distinguish between the soft, hard and arachnoid membranes.
Anatomy Basics
Have you been trying to heal your JOINTS for many years?
Head of the Institute for Joint Treatment: “You will be amazed at how easy it is to heal your joints by taking every day...
Read more "
The spinal cord is located in the cavity of the spinal canal, which is formed by the bodies and processes of the vertebrae. Its origin comes from the brain in the foramen magnum (at its lower border). The end of this formation occurs in the area of the I-II lumbar vertebrae. At this point it narrows into the conus medullaris, from which the filum terminale branches downwards. In the upper sections of the thread there are elements of nervous tissue.
The conus medullaris below the second lumbar vertebra is a formation of connective tissue that consists of three layers. The end of the terminal filament falls on the second coccygeal vertebra, at the place of its fusion with the periosteum. The roots of the lower spinal nerves wrap around the filum terminale and form a bundle called the cauda equina. The length of the adult spinal cord ranges from 41 to 45 cm, and its mass is 34 to 38 g.
Thickenings and grooves
Two sections in this part of the nervous system have noticeable thickenings, namely the cervical and lumbosacral thickening, which are a collection of nerve fibers responsible for the movement of the upper and lower extremities.
Between the symmetrical halves of the human spinal cord there are dividing boundaries - the anterior median fissure and the posterior sulcus. On both sides of the median fissure stretches the anterior lateral groove, from which the motor root originates. This groove separates the lateral and anterior cords of the spinal cord. In the same way, the posterior lateral groove is located behind, which also plays the role of a kind of border.
Roots and substance, their relative position
The gray matter in this part of the central nervous system contains nerve endings - the anterior roots of the spinal cord. At the same time, the dorsal roots of the spinal cord are a collection of processes of sensitive cells that penetrate this part of the nervous system. These cells create the spinal ganglion, located at the junction of the anterior and posterior roots. In total, a person has 62 roots, which extend along the entire length in both directions (31 roots on one side). The part of the organ that is located between two pairs of roots is called a segment. Consequently, each person has 31 segments of the spinal cord - of which 5 segments are in the lumbar region, 5 in the sacral region, 8 in the cervical region, 12 in the thoracic region and 1 segment in the coccyx. The duration of this organ is somewhat shorter than the spinal column, therefore the location of the segment and its serial number do not coincide with the same number of the vertebra.
The SM includes both white and gray matter. In this case, nerve fibers form the white matter of the spinal cord, and the gray matter of the spinal cord is formed by both nerve fibers and nerve cells not only of the spinal cord, but also of the brain.
Gray matter SM
The gray matter is located in the middle of the white matter (on a cross section of the spinal cord it resembles a butterfly), and in its center there is a central canal filled with cerebrospinal fluid. The central canal of the spinal cord and the ventricles of the brain, as well as the spaces located between the meninges, communicate with each other, ensuring the circulation of cerebrospinal fluid. The production of cerebrospinal fluid and its reabsorption are regulated by the same laws as the production of cerebrospinal fluid by the plexuses located in the ventricles of the brain. The study of the fluid washing the SM is effectively used to diagnose many diseases affecting the central part of the human nervous system - this equally applies to infectious, inflammatory, parasitic, demyelinating and tumor diseases.
The gray matter of the spinal cord is formed from gray columns, which are interconnected by a transverse plate. This is the name given to the gray commissure, in the middle of which the opening of the central canal is noticeable. A person has two such adhesions: anterior and posterior, located respectively in the anterior and posterior parts of the central canal. If you analyze a cross section of the spinal cord, it is noticeable that the gray columns at the junction resemble the letter “H” or a butterfly with open wings.
In addition, it is easy to see projections that extend away from the gray matter. These are horns. They are divided into paired wide ones, which are located on the front part, and paired narrow ones - the place of their branch is on the back part. The anterior horns contain motor neurons. The anterior roots of the spinal cord are formed from neurites - long processes of motor neurons. The nuclei of the spinal cord are created from the neurons located in the anterior horn. There are five of them: the central nucleus, two lateral and two medial nuclei, from which cell processes extend towards the skeletal muscles.
The dorsal horn has its own nucleus located in the middle - it is formed by intercalary neurons. The processes of these neurons (axons) are directed towards the anterior horn. They pass through the anterior commissure, thus reaching the opposite side of the brain. Large interneurons have branched dendrites and form another nucleus located at the base of the dorsal horn. The intervertebral spinal nodes contain nerve cells, the ends of whose processes are located on the nuclei of the dorsal horns.
The intermediate part of the spinal cord is located between the anterior and posterior horns. In this area, the lateral horns branch off from the gray matter. This phenomenon is observed starting from the VIII cervical segment and ending with the II lumbar segment. These horns have a lateral intermediate substance consisting of nerve cells that are responsible for the sympathetic division of the autonomic nervous system.
White matter SM
The white matter is formed by three pairs of cords: anterior, posterior and lateral. The location of the anterior cord is between the anterior lateral sulcus and the medial sulcus, at the exit of the anterior roots. The lateral funiculus is located in the interval of the posterior and anterior lateral grooves, and the posterior, respectively, in the interval of the posterior median and lateral grooves. The white matter is formed by nerve fibers that carry nerve impulses. The impulses are directed up to the brain or down to the lower parts of the spinal cord. The gray matter also contains intersegmental nerve fibers, which are short in length and connect nearby segments. These fibers form the segmental apparatus of the spinal cord, because it is with their help that the connection between the segments is carried out.
The dorsal roots of the spinal cord are formed from fibers of neurons of the spinal ganglia. Some of these fibers enter the dorsal horn, others are directed in other directions. Another part of the fibers is part of the posterior cords, it is directed to the brain. These are the so-called ascending pathways. The endings of the remaining fibers fall on the neurons of the autonomous parts of the nervous system in the lateral horns or on the intercalary neurons of the dorsal horns.
What are the SM pathways for and their types?
The ascending tracts of the spinal cord are located outside of its bundles. Impulses from sensory and intercalary neurons are sent upward along them. From the brain down towards the motor center of the spinal cord, impulses also follow along these pathways. Sensory neurons are formed by a thin and wedge-shaped bundle, the functions of which are to supply an impulse from the nerve endings on the muscles and joints to the medulla oblongata.
The conduction function of the spinal cord is carried out by bundles. The wedge bundle is responsible for conducting impulses from the upper limbs and upper torso, and the thin bundle carries impulses from the lower body. The anterior and posterior spinocerebellar tracts carry out the conduction function of the spinal cord, as they conduct impulses to the cerebellum from the skeletal muscles. The posterior part of the spinocerebellar tract originates from the cells of the thoracic nucleus, which is located in the medial part of the dorsal horn. The location of the posterior spinocerebellar tract is on the posterior side of the lateral cord.
The same banned issue for which Ernst fired Malakhov!
Joints and cartilage will be cured in 14 days with the help of ordinary...
The branches of interneurons located in the intermedial nucleus, which is located in the dorsal horn, form the anterior part of the spinocerebellar tract. On the opposite side of the horn, the fibers of the intercalary neurons form the lateral spinothalamic tract, which performs the function of conducting pain sensations and temperature sensitivity initially to the diencephalon, after which the impulse is sent to the cerebral cortex.
How does the human spinal cord function?
The red nuclear spinal tract and the lateral corticospinal tract form the descending tracts. Their location is in the lateral funiculus. Some of them fall on the anterior cord and form the anterior part of the corticospinal tract. A person also has a tegmental and vestibulospinal tract.
These pathways perform similar functions to the spinal cord. The red nucleus spinal tract provides involuntary motor impulses. The path originates in the red nucleus, gradually descending to motor neurons localized on the anterior horns. This is where the name of the path comes from. Voluntary motor impulses are provided by the lateral corticospinal tract, which includes neurites of cells of the cerebral cortex. Closer to the bottom, the path becomes thinner, which can easily be explained by the fact that on each part of the SC, part of the fibers of the path end on motor cells located on the anterior horn.
The reflex function of the spinal cord is also provided by the anterior corticospinal tract, the purpose of which coincides with the purpose of the lateral tract, with the exception of the location of the axons of the cells of the cerebral cortex (they are localized in the anterior cord). The tegnospinal tract originates at the top and bottom of the roof of the brain, and its end is at the level of the anterior horns. The direction of the vestibular spinal tract runs from the vestibular nuclei to the forebrain. The functions of the human spinal cord at this level are to maintain the balance of the body.
The blood supply to the brain and spinal cord is closely related. Blood enters the spinal cord through the anterior and paired posterior spinal arteries, as well as through the radicular-spinal arteries.
As in the brain, choroid plexuses form in the corresponding meninges. Each spinal nerve root extending from the brain is accompanied by an artery and a vein - this is how a neurovascular bundle is formed, if the elements of which are damaged, various pathological conditions can develop. Actually, to diagnose a specific condition that manifests itself as a pain syndrome, it is necessary to perform a whole set of diagnostic tests - only their results make it possible to determine which of the links in the neurovascular bundle is damaged as the cause of the patient’s complaints.
That is why doctors of various specialties - neurologists, neuropathologists, vertebrologists, and orthopedic traumatologists - can identify and treat pathological conditions and diseases of the spinal cord. It often turns out that all these specialists must observe such a patient - only in this case can one provide the patient with effective assistance and alleviate his condition. Neglect of complaints that arise causes the development and progression of various diseases that can cause disability or death of the patient.
In general, the functions of this part of the human nervous system correspond to its structure.
- Ligamentosis of the ankle joint - how to treat it?
- Why is it difficult to breathe with osteochondrosis and what can be done?
- Manifestations and treatment of knee meniscopathy
- Manifestations and treatment of hydromyelia of the cervical spine
- What is spinal angiolipoma?
- Arthrosis and periarthrosis
- Pain
- Video
- Spinal hernia
- Dorsopathy
- Other diseases
- Spinal cord diseases
- Joint diseases
- Kyphosis
- Myositis
- Neuralgia
- Spinal tumors
- Osteoarthritis
- Osteoporosis
- Osteochondrosis
- Protrusion
- Radiculitis
- Syndromes
- Scoliosis
- Spondylosis
- Spondylolisthesis
- Products for the spine
- Spinal injuries
- Back exercises
- This is interesting
- March 16, 2019
- How to get rid of leg pain that appeared after surgery?
- There is tingling and numbness in the feet - what to do?
- What to do and which doctor to go to for shoulder pain?
- When can you sit down after a fracture of two vertebrae?
- My back started to hurt periodically - what to do and what to do?
March 16, 2019
March 15, 2019
March 15, 2019
March 14, 2019
Directory of clinics for spine treatment
List of drugs and medicines
© 2013 — 2021 Vashaspina.ru | Sitemap | Treatment in Israel | Feedback | About the site | User Agreement | Privacy Policy The information on the site is provided solely for popular information purposes, does not claim to be reference or medical accuracy, and is not a guide to action. Do not self-medicate. Consult your healthcare provider. The use of materials from the site is permitted only if there is a hyperlink to the site VashaSpina.ru.
There are procedures to help cope with pain in the back or various diseases of the musculoskeletal system, but in some cases they turn out to be ineffective or dangerous. Detensor therapy is a painless alternative to many spinal traction methods.
How the method works
The author of the technique is the German scientist Kurt Kienlein. He himself suffered from spinal pain, so he took up work on the project. The result was the creation of a moderately soft mattress made of polyurethane foam. The mattress consists of ribs directed in different directions. The central part falls on the lumbar region.
The principle of detensor therapy is to gently and without injury stretch the spinal column, stretch the intervertebral spaces, relax the muscles, and relieve pain. Since weight in this case determines the therapeutic effect, 3 types of material hardness were developed for adults, 2 types for children.
When a person lies down on a traction mat, his body fits tightly against the moving ribs, and the intervertebral spaces appear in their spaces. Thus, from the lower back, the vertebrae begin to stretch in different directions. The technique is safe and is aimed at solving several problems at once, but it must be used regularly to obtain a sustainable result.
The session lasts from 45 minutes. The patient is placed on the movable ribs of the couch in a supine position, a cushion is placed under the head with the same principle of traction, and a special pillow is placed under the legs. The design easily adapts to the required height. A person may experience discomfort or nagging pain in the lower back in the first minutes, but this feeling quickly passes. Therapy involves about 12 procedures, the frequency depends on the severity of the disease.
In what cases is it used?
The popularity of detensor therapy is due to its gentle action, a large list of indications, as well as the versatility of use by people of different ages and body types. The technique can help in the following cases:
- scoliosis at any stage (both congenital and acquired);
- osteochondrosis;
- pain syndrome associated with regular muscle tension;
- prolapse of intervertebral discs;
- the presence or possible appearance of bedsores;
- intervertebral hernia (one or more);
- headache;
- bronchial asthma;
- delayed physical development in children;
- fractures in the spinal column;
- osteoporosis;
- sciatica;
- pathological lordosis;
- radicular syndrome;
- spondylosis deformans;
- various postural disorders.
Therapy may also be indicated for those who lead a sedentary lifestyle, spend a lot of time at the computer and feel back pain, as well as those who regularly experience high physical activity.
How does the procedure affect the spine?
When the spine is stretched, compressed nerve endings are released and posture is corrected. The increase in interdisk spaces from session to session causes them to be fixed at their maximum physiological distance from each other. Cartilage tissue is restored and intervertebral hernias disappear.
During therapy, a person’s body relaxes, the spine is not loaded. Blood supply improves. The spinal column becomes more mobile, natural relaxation of all muscles occurs, and the muscular corset of the back relaxes. The pumping mechanism of the intervertebral discs is restored - fluid begins to flow into them again in the required quantity.
Contraindications
Traction of the spine through detensor therapy is a non-traumatic method of improving the condition of the spine, but even for such a procedure there are a number of contraindications. They can be divided into unconditional, in which traction is impossible, and conditional, providing for individual exceptions.
Unconditional contraindications:
- occlusion of the vertebral arteries;
- end-stage neoplasms of the spinal column or spinal cord;
- inflammatory processes in the spinal cord;
- spinal column infections;
- acute spinal injuries;
- the presence of a large hernia, as well as disruption of the functioning of internal organs due to its presence;
- problems with the functioning of the pelvic organs;
- disc myelopathy.
Conditional contraindications are considered to be abnormal skeletal development, rheumatism in the acute stage, unstable condition of individual parts of the spine and spondylolisthesis above stage 2. Diagnosis of problems with the spine is carried out by qualified doctors - only they can determine whether detensor therapy is necessary in each individual case.
Reviews
The preventive and therapeutic effectiveness of the technique became the basis for a large number of positive reviews.
Anna, 39 years old, Cherepovets: “I was treated for osteochondrosis of the cervical and lumbar regions at a dispensary. There the doctor recommended taking a course of detensor therapy. It turned out that you need to lie on a special structure for 40 minutes, but the main thing is to get down and stand up on it correctly. My back and neck stopped hurting. I bought a pillow with a similar effect for home.”
Vitaly, 47 years old, Moscow: “At first I was skeptical about this therapy. I thought that relaxing on a couch, even a special one, couldn’t have any effect. The first experience was also not impressive, but the vertebrae and joints began to remind themselves more often, so I decided to take a second course. I liked the natural principle of the method, in which my weight turned out to be useful. The effect is achieved through the correctness of all movements and following the doctor’s recommendations. For example, you cannot sit for an hour after the procedure.”
Oksana, 28 years old, Serpukhov: “I spend a lot of time at the computer, my back and neck constantly hurt. I rented a detensor mat from a friend. After just two therapy sessions I felt relief: the headache subsided, the feeling of fullness went away, and my neck didn’t hurt. You can lie on the half-roll separately. I decided to buy a similar complex for home - I will treat the whole family. My grandfather and father also suffer with their spine.”
Alexandra Pavlovna Miklina
- Site Map
- Diagnostics
- Bones and joints
- Neuralgia
- Spine
- Drugs
- Ligaments and muscles
- Injuries
Consultation with a neurosurgeon
neurosurgeon, leading researcher at the Department of Pediatric Neurosurgery, Ph.D. Sysoev Kirill Vladimirovich
author of FEDERAL CLINICAL GUIDELINES FOR THE TREATMENT OF SPINAL BIFIDAS AND FSM IN CHILDREN, approved by the decision of the XXXX Plenum of the Board of the Association of Neurosurgeons of Russia, St. Petersburg, 04/16/2015.
CONTACTS: e-mail
REVIEWS ON SITES: https://prodoctorov.ru/spb/vrach/144441-sysoev/ https://spb.napopravku.ru/doctor-profile/sysoev-kirill-vladimirovich/
The site is for informational purposes only, is not the site of a medical organization, and is not a public offer as defined by the provisions of Article 437 (clause 2) of the Civil Code of the Russian Federation. Interaction with a medical specialist is regulated by the rules of the clinic in which he works.