How does infection occur and who is at risk?
The routes of infection with polio mainly come down to the penetration of the virus through the digestive tract - if water, food or hands have previously come into contact with contaminated substances. For example, feces of a sick person get into a pond, and then when swimming, the patient gets the virus along with the contaminated water. The causative agent of the disease is poliovirus.
You can become infected through water, food, dirty clothes, etc. At risk are:
- children under 7 years old. Poliomyelitis occurs much more often in children than in adults;
- Pregnant women;
- people with very weakened immune systems. This can be facilitated by various diseases, as well as disorders at the endocrine level, periods after operations, etc.;
- people suffering from immunodeficiencies.
The risk of infection is higher during the warm season: summer or autumn. The virus is very tenacious; in a humid environment it can live up to 4 months.
Modes of transmission and symptoms
Poliomyelitis can be transmitted in various ways, often by water, food or household contact, but the possibility of transmitting the disease by airborne droplets or airborne dust cannot be ruled out. You can become infected through water, food or household items that an infected person has come into contact with. Poliomyelitis most often affects children under 10 years of age, with more than half of cases occurring in children under 4 years of age.
The disease does not appear immediately; in some cases, the incubation period can last more than a month, but most often the first symptoms of the disease can be seen already in the first two weeks after infection. Initially, the symptoms of polio are similar to acute respiratory infections, so there is a high probability of not showing proper attention to the patient. In the first three days, the patient feels a headache and general malaise, and a runny nose appears. pharyngitis, sometimes stomach upsets occur. During this period, medical care can be especially effective, but not everyone seeks it because they consider the disease to be harmless.
On days 2-4, the patient’s condition deteriorates sharply, and paralysis occurs. The muscles of the legs and arms are the first to suffer. If complications occur, paralysis is irreversible, and up to 10% of paralyzed people die, since in addition to paralysis of the limbs, paralysis of the respiratory muscles occurs.
Symptoms of polio and course of the disease
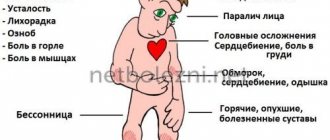
The polio virus causes the following symptoms:
- signs of intoxication: nausea, vomiting, diarrhea, rash;
- cold-like disorders: cough, runny nose, sore throat, difficulty breathing and swallowing;
- fluctuations in blood pressure, fatigue, general poor health, headache;
- in rare cases - various types of paralysis that can lead to the death of the patient.
It is important to note that in 90% of cases, polio has no symptoms and does not affect the nervous system. And in 10% of cases there are very severe forms, involving inflammation of the membranes of the brain - with serious consequences, even fatal.
The incubation period of polio is quite short - it does not exceed 5 days. In this case, recovery in the case of a mild form occurs within 3 days. However, as we have already said, there are also complex forms - they are quite rare, but extremely dangerous. In this case, treatment may last for months, years, or may be completely useless.
Are you experiencing symptoms of polio?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Poliomyelitis or Heine-Medina disease
Vomit
Diarrhea
2531 September 13
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Poliomyelitis: causes, symptoms, diagnosis and treatment methods.
Definition
Poliomyelitis (polios - gray, myelos - spinal cord) is an acute viral disease characterized by damage to the nervous system (mainly the gray matter of the spinal cord).
Thanks to vaccination, polio is now extremely rare. In 2021, about 180 cases of disease caused by wild virus were reported worldwide.
Causes of polio
The causative agents of poliomyelitis are polioviruses. People of any age who are not vaccinated in a timely manner are at risk of contracting polio caused by wild poliovirus. However, children under 1 year of age are predominantly affected.
Humans are the only carrier of wild polioviruses. Infection can occur by airborne droplets, neural and fecal-oral (by consuming contaminated food or water) routes.
The patient sheds viruses during the incubation period and the first week of the disease through the nasopharynx and for 1–6 months with feces. Flies usually serve as carriers of infection.
Polioviruses are stable in the external environment, persist for a long time in water, milk and feces, and do not lose viability at low temperatures. In the human body, it multiplies in the motor cells of the anterior horns of the spinal cord and the motor nuclei of the cranial nerves.
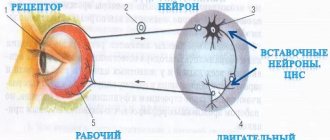
Wild poliovirus, entering the pharynx and/or gastrointestinal tract, attaches to receptors on epithelial cells, where it multiplies and accumulates. The virus then enters the lymphatic system, subsequently into the blood, spreads throughout the body and replicates (multiplies) in many organs and tissues: lymph nodes, spleen, liver, lungs, heart muscle and brown fat. Subsequently, through the endothelium of small vessels or along peripheral nerves, the virus penetrates into the central nervous system and the process involves motor neurons of the anterior and posterior horns of the spinal cord, motor cells of the cranial nerves (glossopharyngeal, vagus, facial, trigeminal), and proximal parts of the peripheral nerves. The reticular formation, vestibular nuclei and deep structures of the cerebellum in the brain are damaged. Nerve cells undergo dystrophic-necrotic changes, disintegrate and die. Cells of the brain stem, subcortical nuclei of the cerebellum and, to an even lesser extent, cells of the motor areas of the cerebral cortex and dorsal horns of the spinal cord undergo less pronounced changes. Paresis and/or paralysis of various muscle groups occur.
Restoration of the functions of paralyzed muscles initially proceeds at a rapid pace, and then slows down and can last from several months to 1-3 years.
After the end of acute events, the dead cells are replaced by scar tissue. The size of the spinal cord decreases.
The stage of residual effects is characterized by persistent flaccid paralysis, muscle atrophy, contractures and deformities of the limbs and trunk.
The transferred disease leaves a stable, type-specific immunity.
Classification of the disease
According to ICD-10, polio is divided as follows:
- acute poliomyelitis;
- acute paralytic poliomyelitis associated with vaccine virus;
- acute paralytic poliomyelitis caused by wild imported poliovirus (type I, II or III);
- acute paralytic poliomyelitis caused by wild local (endemic) poliovirus (type I, II or III);
- acute paralytic poliomyelitis of other and unspecified etiology;
- acute non-paralytic poliomyelitis.
Wild polio virus can be of three serotypes (1, 2, 3) - the presence of immunity from one serotype does not protect against infection by the other two.
Symptoms of polio
The incubation period of the disease lasts from 2 to 35 days. Poliomyelitis can occur with or without damage to the central nervous system (CNS). The prognosis depends on the clinical form and severity of the disease. The most unfavorable prognosis is for the paralytic form of poliomyelitis with respiratory failure.
Poliomyelitis without central nervous system involvement
may have two clinical forms: inapparent (virus carriage) and visceral (“minor disease”). The inapparent form is caused by virus carriage within the pharyngeal ring and intestines. This form has no clinical manifestations, so diagnosis is possible only on the basis of a virological examination.
The visceral form is manifested by a short-term increase in temperature, catarrhal (cough, runny nose, sore throat) and dyspeptic symptoms (nausea, vomiting, loose stools). The disease lasts about 3-5 days and is characterized by a favorable outcome. Diagnosis is possible only on the basis of epidemiological and virological data. From an epidemiological perspective, these two forms of polio are the most dangerous, since the patient, as a rule, is not aware of the disease and does not take precautions.
Poliomyelitis with central nervous system involvement
can occur in the form of a non-paralytic or paralytic form.
The non-paralytic form is manifested by serous meningitis or severe meningeal-radicular syndrome (with pain) without signs of inflammation of the soft meninges. The meningeal form is characterized by general cerebral symptoms (headache, repeated vomiting), fever and intoxication (weakness, weakness, malaise, decreased performance). The meningeal form can have a one- or two-wave course. In a single-wave course, against the background of high temperature and intoxication, meningeal and cerebral symptoms appear on the 1st-3rd day of illness. In a two-wave course, the first wave occurs as a visceral form without signs of damage to the meninges, and after 1-4 days of absence of elevated temperature, a second febrile wave is observed with the development of meningeal symptoms.
The course is favorable, recovery occurs in the third week of the disease.
The paralytic form occurs only in unvaccinated or incompletely vaccinated individuals. Depending on the level of damage, it is divided into several forms:
- spinal (cervical, thoracic, lumbar spinal cord);
- bulbar (nuclei of motor nerves located in the brain stem - III, IV, VI, VII, IX, X, XI, XII pairs);
- pontine (isolated lesion of the nucleus of the facial nerve - VII pair - in the area of the Varoliev bridge);
- mixed forms (bulbospinal, pontospinal).
The course of the paralytic form of polio has four stages:
1 - preparalytic (1-6 days), 2 - paralytic (1-3 days), - restorative (up to 2-3 years), - residual (over 3 years).
The preparalytic period lasts from the onset of the disease until the appearance of the first motor disorders. The disease begins acutely, and body temperature rises significantly. During the first 3 days, headache, malaise, runny nose, pharyngitis are observed, and gastrointestinal disorders (vomiting, loose stools or constipation) are possible. Then comes a period of temperature normalization, which lasts 2-4 days. In some patients this period may be absent. Then the temperature rises again to 39-40°C, the headache intensifies, pain in the back and limbs appears, severe hyperesthesia, confusion and meningeal phenomena, spontaneous pain in the spine, in the muscles of the neck, back, along the nerve trunks and roots, fascicular twitching of the muscles of the limbs, involuntary oscillatory movements of the eyes.
Then paralysis or paresis appears, which in most patients develops within a few hours.
The clinical picture of the paralytic period is determined by the localization of the central nervous system lesions. The legs are most often affected: the quadriceps, adductors, flexors and extensors are affected. On the arms there are the deltoid and triceps muscles, the instep supports of the forearm. Cyanosis, shortness of breath, limited mobility of the chest, retraction of the intercostal spaces and epigastric region during inspiration are characteristic of damage to the diaphragm and intercostal muscles.
With the development of paralysis, spontaneous muscle pain occurs. No sensory disturbances are observed.
When the bulbar form occurs against the background of fever, the functions of swallowing and speech are impaired, the pharyngeal reflex disappears, and asymmetry or immobility of the palatine arches, uvula, and soft palate is noted. There is increased secretion of mucus, which can accumulate in the upper respiratory tract and lead to breathing problems.
When the respiratory and cardiovascular centers of the brain are damaged, arrhythmic breathing with pauses, pathological breathing rhythms, cyanosis, fever, increased or decreased blood pressure, collapse, bradycardia or tachycardia appear. Possible death on the 1st-7th day of the disease.
From the 2nd week, the patients’ condition improves, bulbar symptoms decrease and subsequently may completely disappear.
The pontine form of polio is characterized by damage to the facial nerve. Asymmetry of the facial muscles appears, smoothness of the nasolabial fold on the affected side, drooping of the corner of the mouth, drooping of the eyelids. The course of the disease is favorable, with complete or partial restoration of the functions of facial muscles.
Of the mixed forms, the bulbospinal one is the most severe, since damage to the brain stem occurs in combination with paresis and paralysis of skeletal muscles. In 15% of patients, 10 years after the acute phase, after a period of stabilization, a progressive increase in muscle weakness and atrophy in previously unaffected muscles is detected.
Poliomyelitis in those vaccinated with oral live polio vaccine develops from 4 to 30 days after vaccination. Poliomyelitis can also develop in those in contact with vaccinated people up to the 60th day. Poliomyelitis progresses similarly to the disease caused by a wild virus. To eliminate vaccine-associated polio, WHO recommends switching to vaccination with inactivated polio vaccine.
Diagnostics
The diagnosis is established on the basis of clinical symptoms (meningeal symptoms, weakness of certain muscle groups, weakened tendon reflexes), epidemiological prerequisites (presence of polio in the patient’s environment), and laboratory test data.
All patients with acute flaccid paralysis under the age of 15 years, regardless of the suspected cause of the disease, are subject to examination for poliomyelitis.
Immediately after paralysis is detected, information about this is sent to the Territorial Department of Rospotrebnadzor. Two fecal samples collected (with an interval of 24–48 hours between samples) are sent to the laboratory for poliovirus diagnosis.
The final diagnosis is made by a special commission upon receipt of laboratory data. The final diagnosis is 60 days from the onset of the disease after repeated electroneuromyography.
Laboratory diagnosis of polio includes:
- virological study (study of nasopharyngeal swabs, feces, less often cerebrospinal fluid, blood);
- serological test (blood test for paired sera with an interval of 2-3 weeks; a 4-fold increase in antibody titer is considered diagnostic);
- antibodies to polio virus types 1 and 3;
How the disease is treated in Moscow
Treatment of polio is carried out in an infectious diseases hospital and involves an integrated approach, including:
- strict bed rest. The patient should remain calm, in a favorable environment;
- protection of paralyzed muscles. For this purpose, special splints can be applied;
- physiotherapy. This includes physical therapy, swimming in the pool under the supervision of a trainer, and massage. This also includes electrical stimulation, paraffin applications, UHF therapy and much more. The procedures are aimed at stabilizing the nervous system, helping paralyzed muscles;
- Ventilation Clinical guidelines for polio also suggest major life-sustaining interventions. The use of a mechanical ventilation device is indicated for patients whose paralysis has affected the respiratory system, and therefore threatens respiratory arrest;
- use of special medications.
It is very important that a polio patient be closely monitored, especially when the disease is progressing or not showing significant improvement.
Polio. Causes. Symptoms Diagnostics. Treatment.
Poliomyelitis (infantile paralysis, Heine-Medin disease) is an acute infectious disease caused by a virus that has a tropism for motor neurons of the anterior horns of the spinal cord and motor neurons of the brain stem (nuclei of the cranial nerves), the destruction of which leads to muscle paralysis and atrophy.
Epidemiology
Until the middle of the 20th century. Epidemics of polio occurred, but now, thanks to widespread immunization of children with the polio vaccine, only sporadic cases occur. The number of healthy carriers and aborted cases, when recovery occurred before the development of paralysis, significantly exceeds the number of patients in the paralytic stage. It is healthy carriers and aborted cases that are the main spreaders of the disease, although you can also become infected from a patient in the paralytic stage. The main routes of transmission are personal contact and fecal contamination of food. This explains the seasonality with maximum incidence in late summer and early autumn. At the age of 5 years, susceptibility decreases sharply. The incubation period is 7-14 days, but can last 5 weeks. In the 21st century There is a sharp decrease in incidence in those countries where preventive inoculations are carried out with the Salk, Seibin and A.A. Smorodintsev vaccine.
Etiology and pathogenesis
Three strains of the virus have been identified: types I, II and III. The virus can be isolated from the mucous membrane of the nasopharynx of patients in the acute stage, healthy virus carriers, convalescents, as well as from feces. In humans, the most common route of infection is through the digestive tract. The virus reaches the nervous system along autonomic fibers and perineurally along axial cylinders in the peripheral nerves and in the central nervous system. It is believed that it can spread through the blood and lymphatic system. The site of entry of the virus may be the pharynx, especially the tonsil bed after tonsillectomy. The virus is resistant to chemical agents, but is sensitive to heat and drying. It can be grown in monkey kidney cell culture. Specific serological tests are used, including complement fixation and antibody neutralization tests.
Pathomorphology
The spinal cord is congested with blood, swollen, soft, and there are small areas of hemorrhage in the gray matter. Histological changes are most pronounced in the gray matter of the spinal cord and medulla oblongata. The basal ganglia and cortex are slightly affected. Various changes are observed in the motor cells of the anterior horns - from mild chromatolysis to complete destruction with neuronophagy. The essence of inflammatory changes is the formation of perivascular couplings, mainly from lymphocytes, with a smaller number of polymorphonuclear cells, and diffuse infiltration of gray matter by these cells and cells of neuroglial origin.
Recovery is characterized by a return to normal of those ganglion cells that were not very severely damaged. Other cells disappear completely. The anterior horns show a small number of cells with secondary degeneration of the anterior roots and peripheral nerves. In the affected muscles, varying degrees of neurogenic atrophy are found with an increase in connective and adipose tissue.
Clinical picture
There are 4 types of reactions to the polio virus:
- development of immunity in the absence of symptoms of the disease (subclinical or silent infection);
- symptoms in the viremia stage, which are in the nature of a general moderate infection without involvement of the nervous system in the process (abortion cases);
- the presence of fever, headache, and malaise in many patients (up to 75% during the epidemic); There may be meningeal phenomena, pleocytosis in the cerebrospinal fluid. Paralysis does not develop;
- development of paralysis (in rare cases).
In the subclinical form there are no symptoms. In the abortive form, the manifestations are indistinguishable from any general infection. Serological tests are positive and the virus can be isolated. In the remaining patients, it is possible to distinguish two stages of the clinical picture: preparalytic and paralytic.
Preparalytic stage
. During this stage, two phases are distinguished. In the first phase, fever, malaise, headache, drowsiness or insomnia, sweating, pharyngeal congestion, and gastrointestinal disorders (anorexia, vomiting, diarrhea) are observed. This phase of “minor illness” lasts 1-2 days. Sometimes it is followed by a temporary improvement with a decrease in temperature for 48 hours, or the disease moves into the second phase - the “big illness”, in which the headache is more pronounced and is accompanied by pain in the back, limbs, and increased muscle fatigue. Symptoms resemble other forms of viral meningitis. In the absence of paralysis, the patient recovers. In the cerebrospinal fluid, the pressure is increased, pleocytosis (50-250 in 1 μl). Initially, there are both polymorphonuclear cells and lymphocytes, but after the 1st week there are only lymphocytes. The level of proteins and globulins increases moderately. Glucose levels are normal. During the 2nd week, the level of protein in the cerebrospinal fluid increases. The preparalytic stage lasts 1-2 weeks.
Paralytic stage
.
Spinal shape.
The development of paralysis is preceded by pronounced fasciculations. Pain in the limbs and increased muscle sensitivity to pressure are noted. Paralysis may be widespread or localized. In severe cases, movements are impossible, except for very weak ones (in the neck, torso, limbs). In less severe cases, attention is drawn to the asymmetry of the paralysis: muscles may be severely affected on one side of the body and spared on the other. Typically, paralysis reaches a maximum during the first 24 hours, less often the disease progresses. With the “ascending” variant, paralysis from the legs spreads upward and threatens life due to the addition of respiratory distress. There are also descending variants of the development of paralysis. It is necessary to monitor the function of the intercostal muscles and diaphragm. A test to identify respiratory paresis is a loud count in one breath. If the patient is unable to count to 12-15, there is severe respiratory failure and forced breathing volume should be measured to determine the need for assisted breathing.
Improvement usually begins by the end of the 1st week from the onset of paralysis. As with other peripheral motor neuron lesions, there is loss or reduction of deep and cutaneous reflexes. There are no disturbances of sensitivity, the function of the sphincters of the pelvic organs is rarely upset.
Stem form (polioencephalitis).
Paralysis of the facial muscles, tongue, pharynx, larynx and, less commonly, the extraocular muscles are observed. Dizziness and nystagmus are possible. There is a great danger of involving vital centers (respiratory, cardiovascular) in the process. It is very important to distinguish respiratory disorders due to the accumulation of saliva and mucus during paralysis of the pharyngeal muscles from true paralysis of the respiratory muscles.
Diagnosis and differential diagnosis
Sporadic cases must be differentiated from myelitis of other etiologies.
In adults, poliomyelitis should be differentiated from acute transverse myelitis and Guillain-Barre-Strol syndrome. However, in the first case, flaccid paralysis of the legs is combined with pathological foot signs, sensitivity disorders, and loss of control over the sphincters of the pelvic organs. In infectious-allergic Guillain-Barre-Strol polyradiculomyeloneuritis, paresis is asymmetrical and predominates in the distal extremities, the protein content in the cerebrospinal fluid is increased, but pleocytosis is rare. The bulbar form of polio should be differentiated from other encephalitis, which is clarified using serological tests and virus isolation.
Treatment
If polio is suspected, it is necessary to immediately give the patient complete rest, since physical activity in the preparalytic stage increases the risk of developing severe paralysis. In the presence of paralysis, treatment tactics depend on their extent to the respiratory and tabulus muscles. When treating patients without respiratory disorders, intramuscular administration of ribonuclease, as well as convalescent serum, is indicated. In the acute stage, give a sufficient amount of fluid. A lumbar puncture is necessary for diagnostic purposes and may also relieve headaches and back pain. Analgesics and sedatives (diazepam) are used to relieve pain and reduce anxiety.
Prevention of polio
The main preventive measure is vaccination of children, which is carried out at an early age and then again. There is a special vaccination calendar, on the basis of which pediatricians recommend undergoing this procedure. When vaccinated correctly, lifelong immunity and resistance to poliovirus are developed.
If we talk about the prevention of polio at the household level, it means:
- refusal to swim in dirty bodies of water that are not suitable for this;
- compliance with personal hygiene rules;
- refusal of potentially dangerous products. In this sense, raw milk is undesirable - a pathogen is often found in it;
- Quarantine measures if a child with a disease is detected in a children's group. At the same time, all objects and things are processed and disinfected.
Now polio is quite rare - this is due to centralized vaccination, thanks to which children from an early age develop immunity to the polio virus, and therefore calmly tolerate contact with it.
Poliomyelitis: routes of infection, prevention
Polio
is a viral infectious disease that affects the human nervous system and causes complete paralysis. The virus enters the body through the mouth and multiplies in the intestines.
Poliovirus is widespread, but most often it manifests itself in the countries of Africa and Asia, Ukraine and the Russian Federation (the Republic of Dagestan and the Chechen Republic), where year-round circulation of its strains is observed. In 1988 WHO has set itself the task of completely eliminating this pathology in the next 12 years. The only solution was to vaccinate over 85% of the child population. It was not possible to completely achieve the set goals, although it is impossible not to note the huge reduction in the incidence of polio.
Currently, isolated cases of the disease are periodically recorded. They are associated with non-compliance with the regulated vaccination schedules, as well as with the refusal of some parents to immunize their children against polio, which results in incomplete coverage of the population with preventive vaccinations and an insufficient percentage of the immune layer. All this generally contributes to the preservation and circulation of “wild” strains of the virus in nature.
Is polio contagious?
Polio
- a contagious (infectious) infectious disease, the greatest susceptibility to which is in preschool children.
The source of infection is a sick person or a virus carrier who secretes a pathogenic virus in the stool or nasopharyngeal mucus.
Routes of infection
· fecal-oral. The cause of infection is mainly food contaminated with microorganisms. Flies play a major role in the spread of infection, which is perhaps why in countries with temperate climates there is a summer-autumn seasonality.
· airborne. Patients shed the virus when sneezing or coughing.
Particularly dangerous in terms of infectious diseases are persons who suffer from diseases asymptomatically or with nonspecific manifestations (slight fever, general weakness, increased fatigue, headache, nausea, vomiting) without signs of central nervous system damage. Such people can infect a large number of those in contact with them, because It is very difficult to diagnose sick people, so these people are practically not isolated.
Poliovirus enters the human body through the nasopharynx, multiplies in the epithelial lining of the pharynx and intestines, and then penetrates the cervical and peritoneal lymph nodes. Next, the poliovirus enters the liver, spleen, and bone marrow through hematogenous (through the blood) and lymphogenous (through lymphatic vessels) routes and accumulates there. When it enters the blood a second time, causing another wave of fever, the poliovirus leaks through the blood-brain barrier and damages the central nervous system.
Prevention of polio
Primary prevention, measures aimed at preventing the onset of the disease, is divided into nonspecific and specific.
Nonspecific is aimed at general strengthening of the body, increasing its resistance to various infectious agents (hardening, proper nutrition, timely sanitation of chronic foci of infection, regular physical activity, optimization of the sleep-wake cycle, etc.), combating insects that are carriers of pathogenic microorganisms ( various types of disinfestation), compliance with personal hygiene rules (primarily washing hands after going outside and after visiting the toilet), careful processing of vegetables, fruits and other products before eating them.
Specific prevention consists of vaccination against polio. In order for polio as a disease to be completely defeated, it is necessary to cover 95% of the entire world population with preventive vaccinations.
Currently, vaccination against polio is included in the national compulsory immunization schedule and is given to children starting from the age of three months. Children are vaccinated three times with an interval of 45 days. Shortening the time between vaccinations is unacceptable, with the exception of emergency cases. Then each child is revaccinated with polio vaccines at 18 months, 20 months, and 14 years.
The first two stages of vaccination are carried out by injection with inactivated drugs. The most common single vaccine is Imovax-polio, but complex vaccines, for example, Infanrix, can also be used. Next, the child is vaccinated and revaccinated orally with an attenuated (weakened) live vaccine.
All polio vaccines are low-reactogenic and are usually easily tolerated by children. Rarely, there is a disturbance in general health (fever, loose stools, loss of strength), as well as local changes (the appearance of infiltration and redness at the injection site). Such conditions do not require treatment and resolve on their own within three days.
PARENTS, KNOW:
ONLY VACCINATIONS CAN PROTECT YOUR CHILDREN FROM POLIOMYELITIS
AND ITS SEVERE CONSEQUENCES.
TAKE CARE OF YOUR CHILDREN'S HEALTH!
Prepared material
local pediatrician Ubushieva D.V.
Questions and answers on the topic of polio
Is it necessary to get the OPV vaccine?
Parents have the opportunity to refuse such vaccination - they can write a written refusal and not undergo this procedure. However, doctors warn against such a decision: remember that if 10% of children get sick, the consequences will be irreversible, and for some children such a refusal will cost their lives. Currently, OPV vaccination is the only way to be 100% protected against the polio pathogen.
How is the polio vaccine given?
The vaccination is done twice, starting from the age of three months. The injection is given intramuscularly and contains the virus killed by formaldehyde.
How effective is vaccination against this disease?
Since the active fight against polio (1988), thanks to vaccination, it has been possible to reduce the number of cases from 350 thousand people per year to 359 cases (in 2014). These data speak for themselves: after receiving the vaccine, the disease becomes harmless and no longer threatens the person.
Frequently asked questions about polio
What is polio?
Poliomyelitis is a highly contagious disease caused by the poliovirus. It attacks the nervous system and can cause paralysis or even death in just a few hours.
How is polio transmitted?
Wild poliovirus (WPV) enters the body through the mouth through water or food that has been contaminated with feces from an infected person. The virus multiplies in the intestines and is shed in the feces of an infected person, through which it can be transmitted to other people.
What are the symptoms of polio?
The initial symptoms of polio are:
- heat
- fatigue
- headache
- vomit
- neck stiffness
- pain in the limbs.
Who is at risk of contracting polio?
Polio mainly affects children under 5 years of age.
What are the consequences of polio?
Poliomyelitis causes the following consequences:
- One in every 200 people infected with polio will experience permanent paralysis (usually in the legs).
- Of those paralyzed, 5% to 10% die from respiratory muscle paralysis caused by the virus.
Is there a cure for polio?
No, there is no cure for polio. Polio can only be prevented through immunization. There is a safe and effective polio vaccine, oral polio vaccine (OPV). OPV provides essential protection for children against polio. If used repeatedly, it protects the child for life.
Global fight against polio
What is the Global Polio Initiative?
In 1988, governments created the Global Polio Eradication Initiative (GPEI) to rid humanity of the disease forever. The initiative is a global partnership involving national governments, WHO, Rotary International, the US Centers for Disease Control and UNICEF. Since the creation of the GPEI, the number of polio cases worldwide has decreased by more than 99%. Just 20 years ago, polio caused paralysis in 1,000 children every day. In 2010, 1,349 children were paralyzed.
Where is wild poliovirus still circulating today?
Polio transmission has never stopped in 3 countries - Afghanistan, Nigeria and Pakistan. However, polio can and does spread from these countries to neighboring and more distant countries. It must be remembered that the emergence of polio anywhere is a threat to children throughout the world. He has no regard for boundaries or social status and moves easily.
Can polio spread to other polio-free countries?
Polio does not respect borders: any unvaccinated child is at risk. For every case of paralysis, between 200 and 1,000 children become infected asymptomatically. Therefore, identifying polio is difficult, as is preventing its movement. Children living in areas where immunity levels are low are especially vulnerable. The best defense against imported polio is eradication of the virus. Only in this case will all children be safe.
What needs to be done to eradicate polio?
To stop polio we must:
- engage the entire community in efforts to reach every child left behind;
- develop special plans to reach children from mobile, migrant, conflict zones or remote areas;
- strengthen routine immunization, which is the nation's best defense against polio;
- improve surveillance in high-risk areas;
- encourage governments to reach the poorest people with other public services;
- continue to have the highest level of political commitment from national governments and multilateral institutions;
- close the funding gap - US$590 million is still required to fund activities in 2011-2012;
- make a donation.
Why is so much attention paid to polio and not to other diseases?
Polio is one of the few diseases that can be completely eradicated, as was the case with smallpox. By eradicating polio, we will benefit children around the world, and no child will ever have to suffer the pain of paralysis caused by polio. Most diseases, such as HIV and malaria, cannot be eradicated because the ability to do so does not yet exist. Polio does not have a direct host (i.e. it does not affect animals, and its virus cannot exist in animals, in the same way that malaria exists in mosquitoes, for example); There is a safe and effective vaccine to protect children from polio; it does not survive for long periods of time in the environment and although it is contagious, its infectious period is relatively short. Polio eradication efforts are also helping to strengthen routine health care. Polio eradication efforts have created an active polio surveillance network in all countries, which is now integrating other diseases, including measles. Polio eradication infrastructure is also used to provide other health services, such as the distribution of deworming tablets, vitamin A and mosquito nets.
Oral polio vaccine (OPV)
Why are children given oral polio vaccine?
The polio vaccine is the only means of protection against polio, a paralyzing disease for which there is no cure. It is important to ensure that every child under 5 years of age is immunized against polio. The oral polio vaccine is safe and effective, and because it is administered orally, it can be given by volunteers.
Are there any side effects of the oral polio vaccine?
Oral polio vaccine (OPV) is one of the safest vaccines ever created. It is so safe that it can be given to sick children and newborns. It is used worldwide to protect children from polio and has saved at least 5 million children from permanent paralysis caused by polio. In extremely rare cases, the attenuated virus in the oral polio vaccine may mutate and become virulent again. The risk of getting polio for children is much higher than the risk of side effects from using the polio vaccine.
What are the teachings of Islam regarding the polio vaccine?
Oral polio vaccine (OPV) is safe and has been declared halal by Islamic leaders around the world - Grand Sheikh Tantawi of Al-Azhar University, the Grand Mufti of Saudi Arabia and the Indonesian Ulema Council.
Is it safe to give multiple doses of OPV to children?
Yes, it is safe to give children repeated doses of polio vaccine. This vaccine is intended to be given multiple times to provide complete protection. In tropical regions, several doses of polio vaccine, sometimes more than 10, must be used to ensure complete protection for a child. This vaccine is safe for all children. Each additional dose further strengthens the child's immunity against polio.
How many doses of OPV does a child need to provide protection?
The oral vaccine must be given several times to be fully effective. The number of doses needed to immunize a child depends entirely on the child's health and nutritional status and the number of other viruses to which he has been exposed. Until a child is fully immunized, he or she is at risk of contracting polio. This highlights the need to immunize all children during each round of national immunization days. The polio virus can be hidden in the body of every unvaccinated child.
Should a child be given OPV during polio campaigns and routine immunization?
Yes. Oral polio vaccine (OPV) is safe and effective, and each additional dose means the child receives additional protection against polio. Multiple doses of OPV are required to achieve complete immunity against polio. If the child has received the vaccine previously, additional doses received during national or subnational immunization days will provide valuable additional immunity against polio.
Is OPV safe for sick children and newborns?
Yes. Oral polio vaccine is safe for sick children. In fact, it is extremely important to vaccinate sick children and newborns in campaigns because their level of immunity is lower than that of other children. All sick children and newborns should be vaccinated in upcoming campaigns to give them the protection they need from polio.
Why do some industrialized countries use a different polio vaccine than developing countries?
All but two countries in the world (Sweden and Iceland) used oral polio vaccine (OPV) to eradicate polio and continued to use OPV generally until the late 1990s, when some switched to inactivated polio vaccine due to progress made towards the eventual eradication of polio. (when the risk of wild poliovirus has decreased). Most countries use OPV because it has the unique ability to induce local gut immunity, meaning it can interrupt transmission of wild poliovirus in the natural environment. This is not possible with IPV, an inactivated polio vaccine that stimulates only a very low level of immunity against poliovirus in the intestine, resulting in individual protection against polio, but, unlike OPV, cannot prevent the spread of wild poliovirus.