Make an appointment by phone: +7 (343) 355-56-57
+7
- About the disease
- Cost of services
- Sign up
- About the disease
- Prices
- Sign up
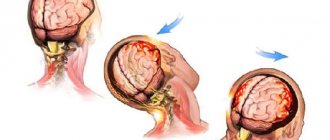
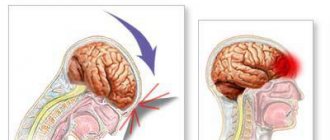
A concussion is a form of traumatic brain injury. In which short-term memory loss may occur, brain dysfunction is reversible. Usually the cause is various traumatic situations. In case of injury, the protective fluid is not able to prevent the impact of brain tissue on the bone tissue of the skull. The injury requires hospitalization and consultation with a specialist.
Classification
Concussion is classified into three degrees:
1.
Mild degree.
The victim is conscious, and within half an hour after the injury there are typical complaints of headache, dizziness, nausea, and disorientation in space. After half an hour the condition returns to normal. 2.
Average.
Consciousness is preserved, short-term memory loss occurs, the symptoms are similar to mild, dizziness persists, there may be a headache, nausea, the victim is disoriented in space. 3.
Severe degree. For her, loss of consciousness lasting a couple of minutes, maybe several hours, is accompanied by retrograde amnesia. Symptoms of headache, dizziness, nausea, disorientation in space can remain for two or three weeks, problems with sleep, and loss of appetite occur. Organic brain lesions lead to the appearance of vascular dementia. This is a secondary disease, that is, occurring against the background of some pathological process. The main reason is a previous ischemic or hemorrhagic stroke.
First aid
For minor head injuries (from a fall from a height no greater than human height) without loss of consciousness, provide first aid to the victim and monitor the symptoms. If you fall from a greater height, bleeding and loss of consciousness, you should immediately call an ambulance.
First aid for concussion:
— Examine the victim; — If there are wounds, treat them and bandage them;
Article on the topic
Concussion: what to do with head injuries
— If you have any symptoms, call a doctor; - Ensure peace. Lay the victim in a comfortable position and do not let him sleep for 30-60 minutes or until the doctor arrives; — Constantly monitor the condition of the victim; - If the victim has lost consciousness, lay him on his side with his knees bent, hands under his head; — If the victim feels well, the incident should not be left unattended and allowed to move actively.
Symptoms of a concussion
General symptoms:
The victim complains of memory loss, dizziness, tinnitus, double vision, intense headache, nausea leading to vomiting, and fatigue. There is sleep disturbance, daytime sleepiness, irritability, and emotional lability. After the injury, confused speech appears, short-term memory loss (retrograde, anterograde amnesia), increased sensitivity to light, noise, balance is disturbed, uncoordinated movements, smell and taste are lost.
Symptoms that may bother you for a longer period:
- intense headache, may be migraine;
- difficulties with reading, remembering, writing;
- absent-mindedness, difficulty concentrating;
- nausea, vomiting;
- drowsiness, weakness;
- dizziness.
Mild traumatic brain injury is considered to be cases of direct or indirect mechanical damage to the brain with a Glasgow Coma Scale (GCS) score of 13-15 30 minutes after injury
Mild traumatic brain injuries in the vast majority of cases occur without consequences, or with transient disturbances that persist for several days/weeks.
Brain concussion
Concussion is defined as a complex pathophysiological process caused by traumatic biomechanical forces. Traumatic changes in the brain have a number of common clinical, pathophysiological and biomechanical characteristics.
Brain concussion
- can be caused by a direct blow to the head, face, neck and other parts of the body with kinetic energy transferred to the head.
- as a rule, leads to the acute development of short-term neurological disorders that resolve spontaneously.
- A concussion may be accompanied by pathohistological changes in the brain tissue, however, the development of symptoms is primarily based on functional disorders. Standard neuroimaging procedures do not reveal any traumatic changes.
- leads to the sequential appearance of clinical syndromes, among which there may not be loss of consciousness. Characteristic is a consistent decline in the severity of the disorders. However, it is important to remember that some of them can persist for a long time.
In addition to a concussion, a mild traumatic brain injury includes a mild brain contusion.
Symptoms of mild traumatic brain injury
Neurological
- Headache
- Nausea
- Vomit
- Double vision and “fog” in the eyes
- "Flashes" or "stars" in the eyes
- Balance disorders
- Dizziness
- Photo and sound sensitivity
- Noise in ears
Behavioral or emotional
- Lethargy
- General weakness or drowsiness
- Irritability
- Depression
- Anxiety
- Increased sleep duration, more than usual
- Difficulty falling asleep
Cognitive
- Feeling slow
- Feeling “numb”, “as if in a fog”
- Difficulty concentrating
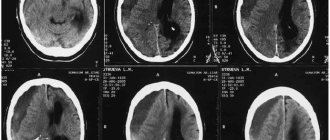
Deterioration of the condition of a patient with a mild traumatic brain injury (appearance/intensification of headache, appearance/worsening of neurological symptoms, appearance of confusion and depression of consciousness) may indicate the development of an intracranial hematoma and requires urgent neuroimaging
For most patients, short-term symptomatic treatment is sufficient:
- for headaches, analgesics and NSAIDs (paracetamol, ibuprofen, naproxen) are used,
- for nausea and vomiting - anti-sickness medications and sedative antihistamines - for mild severity - Dramamine, Atarax, for severe - antiserotonergic drugs - ondansetron, granisetron (Avomit, Kitril).
Many famous people have practiced boxing and have likely suffered repeated traumatic brain injuries.
From this list, I am most impressed by Ernest Hemingway and Vladimir Vladimirovich Nabokov.
It was boxing that “discovered” Charlie Chaplin to the world; he worked as a sparring partner in the lightweight division, was noticed by the director of the Chicago Circus and invited him to perform the act “Boxing in the Arena.”
Exceptions: after 3 months, persistent sequelae in the form of cognitive, mental or neurological impairment remain in 10-15% of individuals who have suffered mild traumatic brain injury (Iverson, 2005). This condition is called "post-concussion syndrome."
Post-concussion syndrome includes at least three of the following groups of syndromes that developed within no more than 4 weeks after injury:
- Headache, dizziness, malaise, general weakness, increased sensitivity to loud sounds;
- Irritability, depression, anxiety, emotional lability;
- Memory and attention disorders, thinking disorders, which are perceived subjectively by the patient and are not recorded by neuropsychological tests
- Insomnia
- Decreased tolerance to alcohol
- Increased preoccupation with the symptoms described above with a hypochondriacal attitude and a painful sense of self
In patients with focal brain lesions, including traumatic ones, as well as in alcohol abusers, repeated, even mild, traumatic brain injuries significantly increase the risk of post-traumatic seizures and epilepsy.
The development of “boxer dementia” is rarely observed in individuals with repeated mild traumatic brain injuries. People with ApoE ε4 (a subtype of lipoprotein, a protein-lipid complex) are predisposed to this complication.
A small proportion of patients develop second-impact syndrome (SIS), a diffuse swelling of the brain after repeated trauma. More often it occurs in athletes against the background of symptoms of a previous concussion. In 1998, 17 cases were described, in 12 of them the description was incomplete. The 2013 paper did not identify conditions that could be clearly considered risk factors for SIS.
- perform craniography if it is possible to perform a computed tomography (CT) scan of the brain - skull fractures without brain contusion - casuistry. If a fracture is detected, a CT scan of the brain is necessary to exclude a bruise and hematoma; if not, the study does not exclude dangerous manifestations of injury in the patient.
- In practice, doctors often have difficulty assessing the bones of the facial skeleton based on radiographs, which also requires repeat CT scanning.
- If you have a tomograph, there is no need to waste time on echoencephaloscopy.
- If access to CT or MRI is limited, it is necessary to reasonably select those who really need the study.
Below, for your reference, are the different sets of indications:
Canadian set of indications*
- GCS score < 15 points;
- Suspicion of an open or depressed skull fracture;
- Clinical signs of a fracture of the base of the skull (hemotympanum, “raccoon eyes,” liquorrhea from the ears and nose, bruising in the parotid region “Battle’s sign”;
- Two or more episodes of vomiting;
- Age ≥65 years;
- Duration of anterograde amnesia ≥30′ from the moment of injury;
- Hazardous mechanism of injury (motorcycle injury, fall more than 3 feet (about 1 meter), or more than five steps;
*The scale is not suitable for cases with the possibility of developing disorders of consciousness due to causes not related to trauma, with a GCS score <13 points, patient age <16 years, if the patient is taking oral anticoagulants (warfarin, Pradaxa, Xarelto, etc.) or suffers from diseases with an increased tendency to bleeding.
New Orleans set of readings
- Headache;
- Vomit;
- Drug or alcohol intoxication;
- Persistent antegrade amnesia (impaired short-term memory)
- Traumatic injuries above the collarbone;
- Convulsive seizures;
- Age ≥60 years;
The risk of detecting brain pathology is higher in patients with a Glasgow Coma Scale score of 13-14 points 30 minutes after injury than 15 points. The following groups are identified according to the severity of risk:
Low risk - 15 GCS points after injury, without loss of consciousness, amnesia, nausea, vomiting, headache - risk of developing intracranial hematoma requiring neurosurgical treatment 0.1:100
Average risk - 15 points on the GCS in combination with loss of consciousness, amnesia, nausea, vomiting, headache - the risk of identifying an intracerebral hematoma requiring neurosurgical intervention is 1-3:100, a CT scan of the brain is necessary.
High risk - GCS score of 14-15, signs of a skull fracture, neurological deficit. The risk of detecting a hematoma requiring neurosurgical intervention is 6-10:100.
The group of high-risk patients, regardless of the clinical manifestations of the injury, includes persons with a history of taking anticoagulants before injury, and persons > 60 years of age.
In cases where a CT scan of the brain was not performed, it is recommended:
- for two weeks from the moment of injury, refrain from taking alcohol and painkillers, driving a car or other vehicles;
- inform your loved ones about the traumatic brain injury you have suffered and warn that if behavioral disturbances and increased drowsiness appear, you must call an ambulance,
- seek help yourself if your headache worsens, double vision, nausea and vomiting, weakness of the limbs and other neurological disorders occur.
“Qu'ils mangent de la brioche”, French - verbatim. “Let them eat brioche” - “If they have no bread, let them eat cake!”, Queen of France, Marie Antoinette, 1769
- conduct a CT scan of the brain after receiving a negative result from an MRI of the brain (the institution where the care is provided has an MRI, but no CT scan)
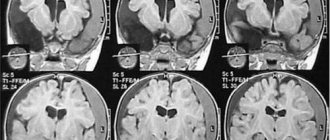
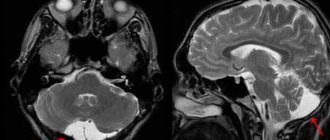
Due to the heterogeneity of conditions caused by biomechanical damage to the brain, which are characterized by impaired memory and orientation, sometimes with loss of consciousness (2013 definition of a concussion), the issue of neuroimaging of traumatic brain injury is complex. The diagnosis is based on the clinical characteristics of the patient; in most cases, conventional CT and MRI studies do not reveal changes in the brain substance in individuals with mild traumatic brain injury.
If a magnetic resonance imaging scanner is available, the method is sufficiently sensitive to detect focal traumatic changes in the brain and intracranial hemorrhages.
MRI, compared with CT of the brain, has greater sensitivity in detecting focal brain lesions. However, neither study provides results that correlate with the degree and nature of neuropsychological impairment.
Both research methods do not accurately detect signs of diffuse axonal damage.
In practice, it is important to identify conditions requiring neurosurgical intervention: hematomas, skull fractures.
The use of data on the nature and prevalence of brain contusions in forming a prognosis and rehabilitation treatment plan has not been developed.
— perform repeated neuroimaging studies (CT and MRI) without medical indications
Unreasonable anxiety from the attending physician is not an indication. Repeated examinations are indicated for patients with progression of disorders of consciousness and focal neurological symptoms, with the development of convulsive seizures. Performing a CT scan exposes the patient to ionizing radiation, which increases the risk of tumor diseases.
The harm from MRI of the brain to health has not been proven, but to the wallet of the patient and the medical institution it is undeniable.
— use rheoencephalography when examining a patient, both after injury and in the long-term period
The study does not provide valuable information, its results will differ with repeated studies, is not needed for the treatment of patients, and acts as an additional source of anxiety.
- perform electroencephalography in patients who have suffered a TBI and have not had epileptic seizures or their equivalents
After TBI, nonspecific changes are more often observed: single sharp waves, groups of sharp waves, less often, peak-wave complexes, uneven alpha rhythm; greater sensitivity to functional tests. The risk of epileptic seizures in people without focal brain damage is low, and the risk of developing epilepsy in people who have suffered early post-traumatic seizures within the first week after injury is also low.
— perform duplex scanning of the brachiocephalic arteries in all patients who have suffered a TBI
dissection of cerebral arteries is a rather rare complication of traumatic brain injury, usually accompanied by clinical signs of cerebrovascular insufficiency, headache and neck pain. Strokes caused by dissection of the precerebral arteries are benign.
Treatment
Treatment of a concussion lasts from 10 days to a month.
Treatment at home is only possible for minor head injuries with the permission of a doctor. When treating at home:
- bed rest and long sleep;
| Protection! | |
| A helmet helps reduce the risk and severity of an impact and can save you from skull fractures. Important! Remember that a helmet will not prevent a concussion. | |
- listen to music (but not through headphones), reading is not recommended; - use sedative folk remedies or light herbal infusions; - long-term dairy-vegetable diet with limited salt intake.
IT IS FORBIDDEN
- watch TV, videos, play on the computer, Gameboy or Tetris - flashing frames irritate the brain; - exercise.
What should you not do if you have a concussion?
Medical staff report that most complications after a brain injury are associated with people’s ignorance of the rules of first aid to the victim. Doctors report that it is strictly forbidden to move the patient abruptly; without examination by a competent physician, there is no need to carry out transportation. Do not give water, food or pharmacological drugs. A person who has suffered brain damage needs a thorough examination by a neurologist. Only he will be able to draw a correct conclusion, based on the patient’s existing complaints and the clinical picture as a whole. It is imperative to take into account that changes in the central nervous system may appear several hours after the accident, and sometimes even days. Therefore, observation by a doctor and timely diagnosis are considered an important rule. You can sign up for a body scan through the search portal mrt-mozga.ru. With us you can take advantage of promotional offers and discount points to save on the procedure.
First aid for a concussion
The first thing you need to do is to ensure that the victim is at rest, lay him down on a flat area, unbutton his clothes and make sure that there is free passage of air into the lungs - turn the patient’s head to the side and take out his tongue, if necessary. Trying to eat or drink anything will result in vomiting. If there is a buzzing in the ears and dizziness, the patient should take a horizontal position. If damage to the cervical spine is suspected, it should be fixed using available means. To create a splint, any fabric that needs to be rolled up in several layers and placed under the neck is suitable.
As soon as a concussion has been received, you need to dial the emergency number. The victim can only be moved by a medical team; independent transportation is dangerous. When it is not possible to call an ambulance, careful transportation of the patient in a supine position is allowed. If a person is unconscious, you need to give him ammonia to sniff. When he is conscious, but reports severe pain in the head area, to which nausea and vomiting are added, this indicates the possibility of developing intracranial hemorrhage. In this situation, first aid will not have any effect, so the patient must be taken to the hospital immediately.
How does the disease manifest itself?
Concussion can present in varying degrees of severity. With a mild injury, the patient exhibits the following symptoms:
- bruise of a strong nature;
- formation of glare in the eyes;
- loss of consciousness for a short period (quite rare);
- dizziness, which increases with sudden movements, bending or turning the head.
After 7 days, the patient may experience a feeling of recovery, but it is usually false. Full rehabilitation occurs only after 2-3 weeks. If the ophthalmologist discovers fundus deformities at the appointment, recovery will take even more time.
A moderate concussion is accompanied by the following symptoms:
- loss of consciousness;
- gag reflexes;
- darkness in the eyes;
- irritable reaction to noise, bright light;
- formation of subcutaneous hematomas or lumps;
- feelings of fear, delirium, or hallucinations for no apparent reason;
- disruptions in the coordination of movements as a result of lack of air.
The patient needs immediate hospitalization. Doctors prescribe bed rest for 14-21 days. An important condition is that the victim be in a darkened room during the first days. This type of injury is characterized by symptoms of lung injury.
A severe degree means that the patient should be urgently taken to intensive care. Delays can cause irreversible processes, which will lead to the slow death of the organ. The result is disability. Typically, patients need to spend at least 24 hours in the intensive care unit. The recovery period takes a long time - at least 3 months.