Radiation diagnostics
CT semiotics
A soft tissue infiltrate is detected in the area of the cavernous sinus, spreading through the optic canal, the superior orbital fissure into the orbit; through the inferior orbital fissure, the infiltrate spreads into the pterygopalatine fossa and paranasal sinuses.
MRI semiotics
T1-weighted images: granulomas have an isointense MR signal
T2-VI, FLAIR: granulomas are iso-, slightly hyperintense
Contrast-enhanced T1-weighted images: granulomas usually accumulate contrast agent
MRA, CT angiography: narrowing of the lumen of the internal carotid artery may be observed.
Differential diagnosis
It is carried out with various pathological processes leading to the development of secondary superior orbital fissure syndrome. These include primary or secondary (metastatic) tumors of the anterior or middle cranial fossa (meningioma, non-Hodgkin's lymphoma), neurosarcoidosis, vascular anomalies (carotid-cavernous anastomosis, dissection of the ICA wall, ICA aneurysms), orbital myositis, cavernous sinus thrombosis, hypertrophic basal pachymeningitis, Wegener's granulomatosis, polyarteritis nodosa, etc.
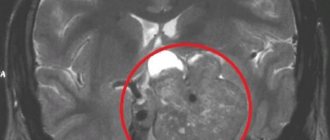
Fig.1. MRI of the brain, T2-VI in the coronal plane: in the projection of the left cavernous sinus an isointense infiltrate is determined, partially narrowing the lumen of the left ICA.
Fig.2. MRI of the brain in the axial plane, a – T1-FS after IV contrast, b – T2-VI. In the area of the right cavernous sinus, a zone of accumulation of contrast agent is determined with a partial narrowing of the lumen of the right ICA (a, green arrows); on T2-WI this zone has a hypointense MR signal (b, green arrows) due to fibrotic changes.
Fig.3. MRI of the brain, T1-VI in the axial plane after intravenous contrast (a, b): a - state before treatment: in the projection of the left cavernous sinus, apex of the orbit and superior orbital fissure, a tissue component is visualized, intensively homogeneously accumulating contrast agent: b – after treatment with glucocorticosteroids, there is a significant decrease in the size of the infiltrate.
Introduction
Tholos-Hunt syndrome (HTS) is a rare disease characterized by a combination of dysfunction of one or more cranial nerves (oculomotor, first or second branches of the trigeminal nerve, optic nerve) with pain of varying severity in the orbital or periorbital region.
This syndrome was first described by the Spanish neurologist ES Tolosa in 1954 and supplemented in 1961 by a group of American neurosurgeons led by WE Hunt, which is how the modern name of this clinical syndrome, CTX, was historically established [1, 2].
In clinical practice, STX occurs equally often in men and women, mainly in the elderly and senile. Most rarely, CTX occurs during the first two decades of life; descriptions of such clinical cases are sporadic [3]. The incidence of STX is 1–2 cases per 1,000,000 adults; there are no statistical data in pediatric practice [4].
Clinical manifestations develop acutely or subacutely after a viral infection, hypothermia, or stress. As a rule, the first neurological symptom is pain of varying intensity, localized retrobulbar, in the frontal, superciliary or temporal regions. A few days later (less often simultaneously), diplopia, strabismus and limited mobility of the eyeball on the side of pain appear. The development of total ophthalmoplegia is associated with damage to all nerves passing through the superior orbital fissure and occurs in 25% of cases of STX [5].
The basis for diagnosis is follow-up data on the periodic occurrence of unilateral symptoms of damage to the superior palpebral fissure and/or cavernous sinus. Routine general clinical and biochemical tests are not informative. When analyzing cerebrospinal fluid, 50% show normal or a slight increase in protein levels up to 1 g/l with a rare minimal change in cytosis; the main method for confirming CTX is MRI or multislice computed tomography [6].
Practice shows that similar clinical signs are observed in a wide range of neurological and somatic diseases: bacterial, viral and fungal inflammation of the outer wall of the cavernous sinus or meninges; primary or secondary tumors of the brain and orbit (pituitary adenoma, sphenoid wing meningioma, craniopharyngioma, neurinoma, metastases to the brain and/or orbit); vascular malformations (arteriovenous aneurysms of the internal carotid artery, carotid-cavernous anastomosis, etc.) and dissections of the branches of the internal carotid artery; thrombosis; lymphoma; epidermoid cysts of the cavernous sinus; orbital myositis; sarcoidosis; some blood diseases; ophthalmic migraine; systemic autoimmune diseases such as Wegener's granulomatosis, systemic lupus erythematosus; with Crohn's disease. For this reason, patients with a characteristic clinical picture require careful examination to exclude other organic pathology [7, 8].
Most often, STX is based on autoimmune mechanisms of the formation of granulomas (granulomas) in the area of the outer wall of the cavernous sinus and/or in the projection of the superior palpebral fissure, identified by neuroimaging using MRI of the brain or during transnasal biopsy. Particular attention is paid to cases of so-called idiopathic CTX, when there are no inflammatory or autoimmune causes, MRI data are normal, or the existing changes are nonspecific - such patients require follow-up observation to exclude other genesis of the disease [9].
We present our own clinical experience of diagnosing CTX in a child, believing that a description of the disease in childhood is of undoubted interest for practicing neurologists and pediatricians.
Description example
Descriptive part (brain): in the projection of the outer wall of the right cavernous sinus, soft tissue formations (granulomas) up to 0.6 cm in diameter with a diffuse-homogeneous type of accumulation of contrast agent are determined.
Conclusion: The MR picture of a focal infiltrative lesion in the wall of the right cavernous sinus, taking into account the location, signal characteristics and accumulation of contrast agent, may correspond to the manifestations of Tolosa-Hunt syndrome.
Descriptive part (MRA): multiple small parietal filling defects are determined at the level of the subclinoid segment of the right ICA (ascending part) and siphon, the minimum diameter of the artery at the level of the subclinoid segment on the right is 0.2 cm.
Conclusion: MRA picture of narrowing of the lumen and decreased blood flow of the intracranial section of the right internal carotid artery, multiple small parietal filling defects at the level of the subclinoid segment (ascending part), siphon of the right internal carotid artery.
Clinical observation
Patient S., 6 years and 3 months. At the time of hospitalization, she complained of pain in the right eye, lacrimation, drooping upper eyelid, dizziness, and increased body temperature to 37.2–37.4 °C. These clinical manifestations persisted for three days.
From the medical history, according to the mother, it is known that a similar condition arose in the child for the third time. At the age of 1 year and 2 months. the girl was hospitalized in the hospital with the same focal symptoms. However, given that at the time of hospitalization the girl had symptoms of acute respiratory viral infection, a rise in body temperature to subfebrile levels and a slight increase in protein levels to 0.6 g/l in the cerebrospinal fluid without an increase in cytosis, a diagnosis was made: encephalitis of viral etiology, with a predominant localization in the posterior cranial fossa, with ophthalmoplegic syndrome. Neuroimaging of the brain using MRI revealed only signs of incomplete myelination. An examination by an ophthalmologist did not reveal any pathology. During treatment with glucocorticosteroids (GCS) for 2 weeks. focal symptoms regressed.
Similar symptoms were observed again at the age of 3 years and 2 months. Despite being completely healthy, the child developed pain in the orbit of the right eye with ptosis of the upper eyelid. The girl was hospitalized with suspected acute cerebrovascular accident. An MRI examination was performed: no organic signs of brain damage were detected. Pathology of the organ of vision is excluded. A diagnosis was made: acute neuropathy of the oculomotor nerve of unspecified etiology. After two weeks of treatment, which, as before, included corticosteroids, the clinical manifestations completely regressed.
After discharge from the hospital, she was under the supervision of a neurologist at her place of residence and received courses of nootropic and dehydrating therapy.
From the life history it is known that the child was born from the second full-term pregnancy; during pregnancy, the woman had two episodes of acute respiratory infection without fever, with mild catarrhal symptoms, and received symptomatic treatment. Childbirth is physiological independent. In the first year of her life, the girl grew and developed in accordance with her age. She was not registered at the dispensary with narrow specialists.
At the age of four years, the patient was diagnosed with bronchial asthma, for which she receives specific therapy, including courses of hormonal therapy (GCS). At the time of hospitalization, bronchial asthma was in remission. Vaccinated according to the vaccination calendar of the Russian Federation.
Neurological status.
Consciousness is clear, the patient is communicative, oriented in time and space, but emotionally labile and tearful. There are no meningeal signs. Palpebral fissures D
Data from general and biochemical blood tests, general urine analysis without any features. Consulted with an ophthalmologist: no gross disturbances of oculomotor function were detected. There are no changes in the fundus.
MRI study of the brain with angiography of cerebral vessels.
No evidence was obtained for the presence of focal changes in the brain substance. MR angiogram: asymmetry of the diameters of the intracranial segments of the vertebral arteries (D>S); non-linear course of the main artery; variant of the circle of Willis structure in the form of incomplete posterior trifurcation of the right internal carotid artery and decreased blood flow along the right posterior communicating artery.
Electroencephalographic video monitoring: without pathology. Examined by an endocrinologist: endocrine pathology was excluded. Myasthenia gravis, local (ocular) form, was excluded. Chest X-ray: no focal or infiltrative changes in the lungs.
Taking into account complaints upon admission, medical history (third episode of ophthalmoplegia), clinical manifestations and additional examination data, the final diagnosis was made: acquired idiopathic right-sided ophthalmoplegia, STX.
During his stay in the department, complex treatment was carried out: pulse therapy with corticosteroids (dexamethasone sodium phosphate 4 mg/day) for 12 days, cholinomimetics with anticholinesterase action (neostigmine methyl sulfate 0.6 ml/day) and vitamins with microelements. During treatment, clinical manifestations completely regressed.
List of used literature and sources
- Diagnostic imaging. Brain / Anne G. Osborn, Karen L. Salzman, and Miral D. Jhaveri. 3rd edition. ELSEVIER. Philadelphia, 2021. P.1237. ISBN: 978-0-323-37754-6
- Rohini Nadgir, David M.Yousem. Neuroradiology. 4th edition. ELSEVIER. Philadelphia, 2021. P.630. ISBN: 78-1-4557-7568-2
- Tolosa-Hunt syndrome [Electronic resource] / Radiopaedia.org: website. – URL: https://radiopaedia.org/articles/tolosa-hunt-syndrome-3 (06/11/2018)
- Neurology: national guide / ch. ed. E.I. Gusev, A.N. Konovalov, V.I. Skvortsova, A.B. Gekht. – M.: GEOTAR-Media, 2009. – 1035 p.
- Ponomarev V.V. Tolosa-Hunt syndrome: definitions, clinical picture, diagnosis, treatment // Medical news. – 2015. – No. 1. – P. 6-9.
Treatment methods
To relieve pain, corticosteroids are used, which are the drugs of choice and improve the patient's condition 24-72 hours after the start of therapy. The mechanism of action of prednisolone is associated with the suppression of the activity of granulocytes and lymphocytes, the synthesis of antibodies and increased capillary permeability.
Important! Treatment should be continued for 7-10 days and, after pain relief, the dosage of the drug should be gradually reduced. If symptoms do not improve within 72 hours of starting treatment, the diagnosis of Tolosa-Hunt syndrome is questioned.
Ophthalmoparesis does not resolve quickly and, as a rule, several months are needed to restore the motor function of the muscles of the eyeball. In severe cases, when the inflammatory process has caused severe damage, function may not be restored to its original state. If hormonal therapy is ineffective, drugs with an immunosuppressive effect are used - methotrexate and azathioprine, as well as radiation therapy. Azathioprine has a suppressive effect primarily on T lymphocytes. About 10% of patients have idiosyncrasy (congenital hypersensitivity to the drug), so it is necessary to monitor the level of leukocytes and lymphocytes. A decrease in blood leukocytes to 3000 cells per microliter (µl), and lymphocytes to 1000 cells per µl is considered unfavorable.
Surgical treatment of Tolosa-Hunt syndrome is rarely used and is used more for the purpose of histological examination of the tissue samples obtained.
Possible complications are associated with the spread of the inflammatory process to the optic nerve, which in severe cases leads to loss of vision.