Pathogenesis
The causes of the onset and development of the disease include multiple factors. These include:
- disruption of lipid (fat) metabolism;
- excess cholesterol in the blood (this condition has its own reasons);
- slow elimination of cholesterol;
- persistent increase in blood pressure for a long time;
- genetic predisposition;
- increased blood viscosity;
- diabetes mellitus (therapy is carried out by an endocrinologist);
- weakness of the vascular wall;
- general condition of the body;
- diseases of unspecified genesis (origin).
The group of those at risk of cerebral atherosclerosis includes:
- smoking and alcohol abusers;
- obese;
- leading a sedentary lifestyle;
- having frequent or prolonged experiences, stress. (Consultation with a psychologist will help to cope with the problem)
What happens in the vessels?
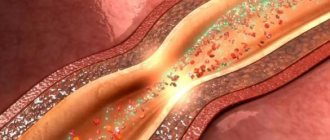
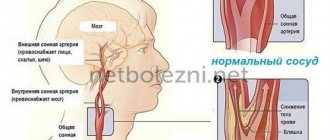
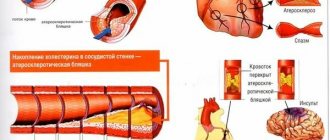
As a result of a failure in lipid (fat) metabolism in the body, cholesterol begins to be deposited on the vascular wall, gradually increasing and forming atherosclerotic or lipid plaques. Over time, they become larger and clog the channel, slowing down the normal flow of blood, and with it delaying the supply of oxygen to all parts of the brain.
Next, loose and then dense blood clots form in the vessels of the brain tissue, which accumulate near the nodes where the lateral branches depart from the arteries and in the cerebral cortex.
The main and middle arteries are at risk of overgrowing with thrombotic plaques. Thrombosis results in cysts, scars, and areas of dead cells (necrosis).
When nerve cells suffering from a lack of oxygen are destroyed, mental activity is disrupted.
Causes of vascular atherosclerosis
There are many theories about the development of atherosclerosis, they are mainly associated with lipid metabolism disorders, hereditary factors, inflammation, poor environmental conditions, etc. For example, according to one version, the cause of the pathology lies in the presence of an infection in the body (chlamydia, cytomegalovirus, etc. ). The theory is supported by the fact that an immune test in the blood of some patients with atherosclerosis detects antibodies to these pathogens. However, what really leads to vascular atherosclerosis is not known for certain.
The causes of atherosclerosis are usually divided into correctable (depending on the person) and non-correctable .
The first group includes:
- Hypertonic disease;
- smoking;
- obesity, craving for fatty foods;
- diabetes;
- adynamia.
The second group includes:
- Gender - men get sick earlier and under 50 years of age - more often; women usually “join” them after menopause and quickly “catch up” in terms of incidence;
- age - aging of the body inevitably causes changes in blood vessels;
- hereditary factor.
1 Bicycle ergometry for atherosclerosis
2 VEM for atherosclerosis
3 ECG - diagnosis of atherosclerosis
Symptoms at different stages of the disease
The disease manifests itself in constantly developing brain failure, chronic circulatory disorders in the vessels, ischemic and hemorrhagic strokes.
The main external signs of developing dystrophy and necrosis of brain cells are disturbances in the human psyche and mental activity, paresis, paralysis, urinary or fecal incontinence.
In this case, three base periods are distinguished.
First stage
Its signs are:
- weakness, fatigue;
- problems with remembering information;
- noise, ringing in the ears;
- dizziness, lightheadedness (for other causes of dizziness, read here);
- feeling of constriction, dull pressure in the head,
- sensation of “goosebumps” on the skin, numbness;
- “flies” before the eyes;
- unsteadiness of gait;
- flushes of heat and sweat on the face;
- increased cholesterol (cholesterol levels are described here).
During the development of atherosclerosis it is characteristic:
- memory impairment (especially for numbers, names, dates);
- decreased performance;
- problems with switching attention to different thoughts and activities;
- neurotic manifestations;
- low mood, pessimism;
- lack of desire to do anything;
- inhibition of reactions and thoughts;
- unmotivated tearfulness, touchiness, and for some, euphoria for no reason.
Period of progression and clear clinical symptoms
Signs may be:
- trembling hands, unsteadiness of gait, unintelligibility of speech;
- problems with coordination, slow pace (motor skills);
- anxiety, suspicion, the emergence of fears (stalking, spying, theft, death at the hands of relatives and neighbors);
- preoccupation with imaginary diseases;
- soreness while eating;
- intense constant headache;
- nightmares;
- complaints of strange sensations - tingling in the legs, “burning in the back of the head.”
Manifestations of psychopathic states:
- short temper, irritability, malice, hysterical reactions with exacerbations;
- development of stinginess, pettiness, constant grumpiness, sloppiness;
- obsessive thoughts (fixed ideas) about money, dangers, thieves;
- interests are narrowed to physiological needs for food and sleep.
This phase is characterized by anxiety-delusional, depressive syndromes, degenerative changes in brain tissue (atherosclerotic encephalopathy). If you have symptoms, seek help from a psychologist.
Period of dementia (dementia)
Among the signs are the following:
- temporary memory loss, deterioration in thinking ability;
- trembling of the head and hands;
- narrowing, tortuosity of the vessels of the fundus;
- increased pulse in the arteries of the neck (even with normal pressure);
- impaired memory of present events;
- problems with self-service (gas, iron, electricity, water turned on);
- violations of hygiene (during defecation, urination);
- disorientation in time and location.
At this stage, a person is practically unable to do without help, care, and constant supervision.
At this stage, an acute circulatory disorder in the cerebral vessels may occur in the form of strokes:
- Ischemic occurs due to blockage of blood vessels by a thrombotic substance. Oxygen does not reach the brain, cells begin to die. There is trembling and changes in the shape of the pupils, sensory disturbances, movements in the limbs, disturbances in speech, swallowing, vision, asymmetry on the face, a constricting headache with dizziness.
- Hemorrhagic stroke occurs less frequently, but its development is more rapid. In this case, the vessel does not close, but bursts, and blood flows out of it into the brain tissue. There are 2 areas of damage - a bloodless area and brain tissue, compressed by the resulting hematoma.
The complexity and danger of the last two stages of the disease is that it is very difficult to accurately determine the type of stroke in a patient based on the signs.
New cholesterol controversy
When do you really need to lower cholesterol and who can live long with high levels? The material about this, prepared by KP, was among the top most read on the newspaper’s website.
Dossier "KP"
Philip Kopylov is a professor at the Department of Preventive and Emergency Cardiology, Director of the Institute of Personalized Medicine at Sechenov University, Doctor of Medical Sciences, researcher, cardiologist.
THE MAIN CHALLENGE FOR DOCTORS
Recently, an international group of cardiologists from Sweden, Italy, France, Japan and other countries made a revolutionary statement: there is no evidence to conclusively support the connection between high levels of “bad” cholesterol and cardiovascular disease. The researchers came to this conclusion after studying data from 1.3 million patients. Their health status was monitored for a total of about 50 years. Even more surprising, according to cardiologists, was that older people with high levels of low-density lipoproteins (the same “bad” cholesterol) live on average longer than others! How is this possible? Does this mean that scrambled eggs, butter and fatty meats have been finally rehabilitated, and doctors need to reconsider their approaches to treating heart patients with statin drugs?
“There may be two people standing in front of us, both of them have high cholesterol, only one needs to be treated, and the second can be left alone,” says Philip Kopylov. - Essentially, this is a solution-explanation of the results of a study on the role of cholesterol, which surprised many. The secret is that monitoring people from different risk groups gives different results. And medications act in different ways: if you give them to a sick person according to medical indications, his condition will improve. But if you feed someone who is healthy or who is not so sick that they really need serious medications, then there will be no improvement. The main task, I would even say a challenge, for modern doctors is to determine those who really need to lower cholesterol and when such patients really need statins. Because other people can live longer without treatment, including those with relatively high levels of “bad” cholesterol.
CHECK YOURSELF
What is your risk of cardiovascular disease?
A person is at low risk if they:
a) no high blood pressure. That is, the pressure is not higher than 130/80 mm Hg. Art. under the age of 65 and not higher than 140/80 after 65 years;
b) no excess weight. That is, the body mass index is not higher than 29 (we talked about how to calculate it in the first part of the publication);
c) no diabetes;
d) no atherosclerosis.
- Under such conditions, the patient usually does not need to be treated even if the level of “bad” cholesterol is elevated. That is, if the level of LDL (low-density lipoprotein) in the blood is up to 4.9 mmol/l, explains Philip Kopylov.
If a person is at high risk of cardiovascular disease, including a high risk of heart attack and stroke, then the cholesterol level should be no more than 2.6 mmol/l. And at a very high risk - a maximum of 1.8 mmol/l . If the indicators are higher, they need to be reduced, including with the help of medications.
into the high and very high risk group (depending on the number of risk factors and the degree of neglect) if:
1) is obese. The most dangerous thing is abdominal, that is, in the abdomen. Measure your waist width: for men the critical mark is 102 cm and more, for women – 88 cm and more;
2) high blood pressure (see point “a” above);
3) there is a diagnosis of diabetes mellitus (as a general rule, it is made when the blood sugar level is above 6.7 mmol/l on an empty stomach);
4) the patient abuses salt - exceeds the norm of 5 mg per day, including salt in all dishes and products;
5) overindulges in alcohol. Let us remind you that, according to the latest data, up to 14 servings of alcohol per week for men and up to 8 servings for women are considered relatively safe for health (how much this will be in different types of drinks - see the “Health” section on kp.ru);
6) male gender - the risk of cardiovascular diseases in men is a priori higher;
7) age - for women over 50 - 55 years old; for men - from 45 years old, and if the above factors are present - then starting from 35 years old.
CHOLESTEROL PLAQUE DIFFERENCES PLAQUE
- If I am not in a high or even medium risk group, does this mean that I can unlimitedly eat foods with animal fats - butter, fatty meat, etc.?
— The question is not easy. When we begin to lean on foods rich in animal fats, with a modern sedentary lifestyle, this often results in obesity. You receive at least one risk factor and move from a more “favorable” group to a less favorable one, with a higher risk. And in general, we must admit: the regulation of the system of production and metabolism of cholesterol in the body still partially remains a mystery to scientists. We don't know everything about her.
— Is it undeniable that cholesterol plaques in blood vessels are harmful and dangerous? Or do you also have doubts?
— In humans, already from adolescence, damage to the internal lining of blood vessels begins. And atherosclerotic plaques develop with age in the vast majority of people (essentially, such plaques are accumulations of cholesterol deposits in places of vascular damage. - Author) . However, the problem is that plaques are not all the same. They can be of two types: stable and unstable. And the most serious challenge in cardiology now is to learn to identify and calculate unstable plaques.
- What is their danger?
- At least half of myocardial infarctions occur due to plaques that do not narrow the lumen in the blood vessels or narrow it less than 50%. Such plaques have a thin covering film and a liquid core, where inflammation constantly occurs. Eventually the tire simply breaks. A blood clot forms at this site and blocks the lumen of the vessel. And everything downstream of the blood begins to die.
TO EXERCISE OR NOT TO EXERCISE?
- It is often said that aerobic exercise - brisk walking, running, swimming, ice skating - is useful for increasing blood circulation. And if the plaques are unstable, then it turns out that increased blood flow can worsen the situation?
— Purely theoretically, yes. However, if these loads are regular and reasonable (see below for the “golden” formula for calculating heart rate. - Author) , then they will have a positive effect. Weight and blood pressure will decrease. Also, as a rule, there is a decrease in cholesterol. That is, risk factors are eliminated, and due to this, competent physical exercise brings undeniable benefits. And if you exercise from time to time, and even try to set an Olympic record in the rare moments of your appearance at the gym, then the threat of rupture of plaques and a heart attack really increases significantly.
ON A NOTE
How to determine safe exercise intensity
Use the “golden formula” for calculating your optimal heart rate: 220 minus your age. the resulting figure by 65% - this is the pulse at a moderate load; multiply by 80% - heart rate during intense physical activity. If it is higher, there is already an excessive load, unfavorable for the blood vessels and heart.
QUESTION: WHO NEEDS STATINS?
— Philip Yuryevich, what about statins? Recently, there has been heated debate; the authors of an international study claim that the benefits of such drugs are very doubtful. To whom and why should they be prescribed from your point of view - as a researcher and cardiologist?
- Let's remember: cholesterol enters our body not only with food, 60 - 70% of it is produced in the liver, even if you are on a lean diet. The effect of statins is, on the one hand, to inhibit the production of cholesterol in the liver. At the same time, a mechanism is launched that turns existing unstable plaques into stable ones. And this actually cuts the risk of heart attacks in half.
— It turns out that if a person’s plaques are stable and do not block the lumen of blood vessels, then there are no indications for taking statins? After all, these drugs have serious side effects - from muscle and joint pain to increased blood sugar. When the task is to protect against a real threat, a fatal heart attack, then such “costs” are the lesser of the evils. Are there any current developments to determine the type of plaque in a particular patient?
— There is an intravascular method, when we insert a special sensor into the vessel and use ultrasound or optical coherence tomography to determine the structure of the plaque.
- Do you need to check every plaque?
- Yes. And the sensor, unfortunately, is expensive. Another approach is computed tomography. We put the patient in a computer scanner and do an X-ray examination with contrast of the heart vessels. The resolution of computed tomographs today makes it possible to determine what kind of plaque it is - stable or unstable.
The third approach is a blood test. Now it is actively developing. Very interesting research work is being carried out on microRNAs, that is, small molecules that are responsible for inflammation and the development of atherosclerosis. Based on their presence, concentration and combination, they are trying to build diagnostic systems to identify unstable plaques.
— Are any of these methods used in Russia?
- So far - on a minimal scale, only in large cardio centers, and then as research work for the most part. In general, the problem of determining the type of plaques is solved in different ways throughout the world. The latest international recommendations propose the introduction of computed tomography with contrast as a method of primary diagnosis.
CONGRATULATIONS!
“Sechenovka” has an anniversary!
In 2021, Sechenov University, First Honey, the legendary “Sechenovka”, as it is often called among the people, turns 260 years old. Over these centuries, they worked, taught, treated, created breakthrough methods for saving people here, and most Russian medical luminaries continue to do so. Among the stars of the university is the founder of the school of military field medicine, Nikolai Pirogov ; famous surgeon, professor Nikolai Sklifosofsky ; the founder of Russian forensic psychiatry Vladimir Serbsky ; founder of the medical examination system Nikolai Semashko ; founder of neurosurgery Nikolai Burdenko; founder of the school of cardiovascular surgery Alexander Bakulev . Now among the professors at Sechenovka are academician Leo Bockeria , the chief transplantologist of the Russian Ministry of Health, academician Sergei Gauthier , one of the leading Russian oncological surgeons, an expert on head and neck tumors, academician Igor Reshetov , and many others.
«
Komsomolskaya Pravda" congratulates Sechenov University and wishes new scientific and medical breakthroughs!
Link to publication:
Diagnosis of cerebral atherosclerosis
Suspicion of this disease arises when examining the patient based on characteristic symptoms in accordance with the stage of the disease and his age.
A refined diagnosis is made based on the results:
- duplex ultrasound examination of extracranial vessels (assessment of their condition, absence or presence of narrowings, lipid plaques, blood clots);
- transcranial Dopplerography (analysis of the condition of intracranial arteries);
- magnetic resonance imaging;
- angiography of veins and arteries.
Is it possible to drink wine if you have cerebral atherosclerosis?
Sweet, semi-sweet, semi-dry and dry red wine for cerebral atherosclerosis in moderation probably reduces the risk of stroke. Wine for cerebral atherosclerosis has a positive effect on blood vessels by simultaneously increasing the concentration of high-density lipoproteins (HDL), which are responsible for clearing veins and arteries of low-density lipoproteins (LDL), which in oxidized form form cholesterol (atherosclerotic) plaques, and reducing coagulability blood.
However, excessive consumption of dry or semi-sweet white or red wine, or any other alcohol, on the contrary, leads to an increased risk of stroke. Red wine (dry, semi-sweet, sweet or semi-dry) has an advantage over other alcoholic beverages in the form of resveratrol and other polyphenols it contains - strong antioxidants, which, moreover, also prevent blood clotting, improve the health of the walls of blood vessels, increasing their elasticity.
More elastic vessels are less likely to be damaged and, as a result, less cholesterol plaques form in them. A decrease in blood viscosity and coagulability prevents the formation of blood clots and blood clots when atherosclerotic deposits are torn off or destroyed on the walls of blood vessels in the brain, carotid artery or other veins and arteries of the body.
Purple and red grape juice, non-alcoholic red wine, and red grape extract contain the same beneficial nutrients as red wine.
Treatment
Therapy involves the use of medication (conservative) and surgical techniques.
Surgery
If an ultrasound reveals more than 70% reduction in the diameter of a cerebral artery, the question arises about the need for surgical treatment of the damaged vessel. The most commonly used method is carotid endarterectomy. During the procedure, the vessel is dissected at the site of the blood clot, which is removed, and the integrity of the vessel is restored using sutures.
Other methods are endovascular operations, stenting.
Drug treatment
It is prescribed only by a doctor, taking into account contraindications, medical history and based on the results of studies and tests.
Therapy for cerebral atherosclerosis is aimed at:
- harmonization and restoration of lipid metabolism;
- lowering cholesterol levels (find out the norm from the table);
- elimination of metabolic disorders;
- treatment of concomitant diseases.
To solve these problems, several groups of medications are prescribed:
Statins are an active group of drugs that block cholesterol synthesis in the body, reduce its amount and prevent the formation of plaques. These drugs are Lovastatin, Mevacor, Fluvastin, Mekafor, Simvastatin, Pravastatin.
Means for improving microcirculation , dilating blood vessels, relieving spasms and at the same time preventing platelets from aggregating (sticking together) into clots:
- "Actovegin", "Cavinton", "Curantil".
- “Parmidin”, “Anginin”, “Aspirin” restore blood flow in small vessels, reduce the permeability of the walls, suppress the adhesion of platelets into clots, stimulate the resorption of blood clots, and prevent the deposition of fats and cholesterol on the vascular wall.
Vasodilators:
- “Nicotinic acid”, Nikoshpan” - expand small capillaries, strengthen the cells of the arterial wall, and effectively help reduce cholesterol concentrations. From simple standard means - “Papaverine”, “Eufillin”.
- Among the more progressive medications: Isoptin, Lomir, Amlodipine, Diazem. Cinnarizine and Nimodipine are suitable for long-term use.
- Medicines containing the alkaloid of the periwinkle plant - Vinpocetine (Cavinton, Bravinton) allow you to dilate blood vessels and stimulate metabolism.
- Dietary supplements based on the Gingko Biloba plant are good at relieving vasospasm, stimulating the work of brain cells, and reducing blood viscosity. Taking Gingium, Tanakan, Ginkor Fort is not combined with medications containing aspirin (Trombass, Cardio-magnyl) due to the risk of a serious increase in blood flow and bleeding.
Nootropic drugs activate the process of energy exchange in brain cells, improve memory, mental activity, cerebral circulation and cell resistance to oxygen deficiency.
They treat problems of mental disorders, senile dementia: Piracetam, Nootropil, Bemitil, Cerebrolysin, Aminalon, Sermion (nicergoline), Meclofenoxate, Phezam, Biotredin, Vinpocetine.
Medicines that activate energy metabolism and remove lipids - Lipostabil, Omacor, Eikonol, Thioctic acid.
Medicines to prevent the formation of blood clots when blood viscosity increases and the content of prothrombin in it increases - “Trental”, “Aspirin-cardio”, “TrombASS”, “Pentoxifylline”, “Cardiomagnyl”.
Doctor's advice
There are risk factors for developing stroke and heart attack in the next 5 years that have long been studied and taken into account, called the “SCORE Scale”, in which the higher the cholesterol, the greater the risk. Accordingly, cerebral atherosclerosis increases the risk of sudden cardiovascular accidents. In the first place in the treatment regimen are statins - drugs that lower cholesterol and help reduce the volume of plaques.
Victoria Druzhikina Neurologist, Therapist
Additional tools:
Fibrates – suppress the formation of fats and total cholesterol: “Clofibrate”, “Gemfibrozil”, “Fenofibrate”, “Atromid”, “Bezafibrate”, “Atromidine”.
Fibrates currently cause much controversy in the treatment of cerebral atherosclerosis. When used uncontrolled, fibrates are dangerous, so the dosage regimen and therapy regimen are agreed upon with a cardiologist.
“Nicotinic acid” and “Enduracin” are recommended in cases where atherosclerosis is associated with an increased amount of high-density cholesterol. They dilate blood vessels, but cause a rush of blood to the skin, so their use should be carried out under the supervision of a doctor.
Hypocholesterolemic drugs - Neomycin, Guarem, Colestipol, Probucol, Lipostabil, Eikonol, Benzaflavin - reduce cholesterol, stabilize metabolism, and suppress the formation of blood clots.
In addition to the main treatment medications, it is advisable to take:
- Antioxidants that suppress oxidation processes: Mexidol, vitamins A, E, Aevit, P (strengthen the walls and increase the density and elasticity of blood vessels), microelements - potassium, silicon, selenium, vitamin C, which prevents the formation of fat deposits on the walls of arteries , group B improves the functioning of nerve cells. The use of Ascorutin (vitamin C plus rutin) requires monitoring the level of blood viscosity.
- For neurological manifestations and depression, antidepressants are used: Paxil, Azafen, Amitriptyline.
- When phobias, panic attacks, or severe anxiety appear, tranquilizers are prescribed: Alprazolam, Diazepam, Atarax, Phenazepam.
- If sleep is disturbed, sleeping pills and antidepressants (Donormil, Nitrazepam) are prescribed.
- For headaches and myalgia, the use of drugs that relieve pain and spasms is indicated: “Spazgan”, “Spazmalgon”, “Pentalgin”.
Among the more progressive medications: Isoptin, Lomir, Amlodipine, Diazem. Cinnarizine and Nimodipine are suitable for long-term use. Nootropics are prescribed with caution for dementia, as well as in older people - they activate the nervous system, and thus, as a side effect, can cause hyperexcitability, irritability, and aggression.
Physiotherapy for cerebral atherosclerosis
Aimed at activating blood circulation in the brain and processes in nerve cells, increasing arterial tone, and improving adaptive capabilities. This:
- Electrophoresis with medications.
- Hydrotherapy using carbon dioxide, oxygen, iodine-bromine, sodium, radon baths.
- Electrosleep procedures to strengthen and restore the nervous system.
- Special therapeutic exercises to improve and stimulate proper motor skills, motor functions, and relieve muscle spasms.
Diet therapy
The main provisions of the diet for cerebral atherosclerosis:
- Salt per day up to 3 g.
- Meals are frequent, in small portions.
- The amount of fat is no more than 65 g per day, of which 72% is vegetable.
- The amount of protein is not limited. Animal protein prevents fatty liver and cholesterol deposits in blood vessels.
What you can do:
- lean veal, pork, beef, turkey, fish;
- eggs in the amount of 1 pc. per day: in the form of steamed, baked, soft-boiled omelettes; milk, low-fat cottage cheese, kefir, peas, beans, buckwheat, wheat, oatmeal;
- once a week a little caviar and tongue are allowed. 10-20 g per week of butter is allowed;
- sunflower, rapeseed, corn, cottonseed, olive seeds promote intestinal motility and remove excess cholesterol;
- seafood is very healthy (up to 6 times a week): fish, squid, shrimp, mussels, seaweed, kelp;
- vinaigrettes, salads from cucumbers, zucchini, cabbage, tomatoes, potatoes, pumpkin, soybeans, eggplant, pumpkin, dill;
- You can have low-fat sausage, ham, mild cheeses, dry cookies, marmalade, dried fruit candies, muesli.
What not to do:
- animal fats, offal products saturated with cholesterol, including liver, brains, kidneys are excluded;
- limit sweet dishes, fresh white bread, pure sugar, jam, honey, jams, cakes, buttery sweet cookies;
- Rich meat and mushroom soups, cream, ice cream, butter and custard creams, mayonnaise and sauces based on it, dark chocolate, strong coffee, tea, and alcohol are not recommended.
Folk remedies
In complex therapy of atherosclerosis, traditional methods are used with caution and after consultation with a doctor. They must be combined with medications
Among them:
- Collection for spasms of cerebral vessels, nervous tension. A collection is prepared from valerian root, cudweed, and St. John's wort in equal parts. Drink as an infusion.
- Honey and lemon juice are mixed equally with vegetable oil and taken a teaspoon in the morning (dangerous for allergies and gastritis).
- Drink 100 g of freshly squeezed potato juice for frequent headaches (harmful for stomach diseases).
- An alcohol tincture with garlic and lemon along with zest is known (extremely dangerous for gastritis, peptic ulcers, inflammation of the pancreas).
- Dill seeds (teaspoon), brewed in a glass of boiling water. Drink as tea for headaches.
Despite the fact that atherosclerosis occupies only the walls of blood vessels, the consequences for the brain, the entire body, psyche and intellect are devastating. A person gradually loses his personal qualities and turns into a thoughtless organism that requires constant care and regular feeding.
To prevent such an existence, you should pay attention to the very first signs of the disease, do all the necessary examinations and take timely the whole range of measures aimed at recovery.
How to recognize and how to treat cerebral atherosclerosis, watch the video:
This article has been verified by a current qualified physician, Victoria Druzhikina, and can be considered a reliable source of information for site users.
Bibliography
1. https://www.angiolsurgery.org/recommendations/2013/recommendations_brachiocephalic.pdf
Rate how helpful this article was
4.5 10 people voted, average rating 4.5
Did you like the article? Save it to your wall so you don’t lose it!
What kind of alcohol is possible for cerebral atherosclerosis
If you don't like red wine, you can get enough resveratrol from dietary supplements or a glass of dark grape juice a day. To thin the blood and prevent LDL oxidation, any alcohol is suitable - alcoholic drinks have an identical effect on cerebral atherosclerosis, regardless of their form.
Moderate alcohol consumption has a beneficial effect on the course of atherosclerosis of the vessels of the neck, heart and brain: the number of beneficial HDL particles increases, the elasticity of the walls of blood vessels increases, the oxidation of LDL is suppressed and blood (upper) pressure is slightly reduced. Alcohol for cerebral atherosclerosis, of course, will not destroy already accumulated cholesterol plaques, will not eliminate the risk of stroke (although it will noticeably reduce it, including the risk of a recurrent stroke), but will help fight the disease.
Alcohol in cerebral atherosclerosis also helps reduce the amount of fibrinogen in the blood - this protein is especially important in the formation of a blood clot, and reducing its concentration reduces the risk of blood clot formation. Alcohol from any type of alcoholic beverage has a beneficial effect on HDL cholesterol, blood clotting and suppression of inflammatory processes in the walls of blood vessels in the brain, coronary vessels of the heart, carotid artery of the neck and other arteries and veins of our body.
See also:
Does alcohol have cholesterol?