Dyscirculatory encephalopathy of the brain (DEP) is a progressive lesion of cerebral structures against the background of vascular diseases. It manifests itself as worsening intellectual, psycho-emotional and movement disorders. Widespread, observed to varying degrees in 5–6% of Russians.
An appointment with a neurologist is made by phone 8(969)060-93-93.
How to treat dyscirculatory encephalopathy of the brain
Discirculatory encephalopathy is a chronic damage to the nervous tissue of the brain, the cause of which is a circulatory disorder.
This is a progressive pathology. Irreversible changes in the brain lead not only to instability of the emotional state and changes in behavior (thinking), but in some cases to loss of ability to work and the inability to perform usual everyday tasks. We will talk further about how to treat dyscirculatory encephalopathy of the brain. Types of disease:
- atherosclerotic;
- hypertensive;
- venous;
- mixed.
Based on the nature of the course, discirculatory encephalopathy (DEP) can be classic (sluggish), remitting with a gradual increase in symptoms, and progressive. The main causes of the disease, according to experts, are hypertension and atherosclerosis. Important: medications for dyscirculatory hypertensive encephalopathy will help improve metabolism and blood supply to the brain.
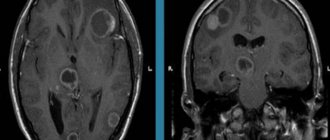
Diagnostics
If you have any of the above symptoms, you should contact a neurologist who knows how to treat such conditions. The doctor conducts a targeted neuropsychological examination, then identifies failures of a neurological nature, prescribes a computed tomography scan to assess the condition of the blood vessels and identify atrophic processes in the brain area. Another study - REG - determines how full the cerebral vessels are with blood, how they work, and whether there are any changes. Based on the diagnostic results, the doctor makes a diagnosis, taking into account the cause of the disease, selects treatment for grade 2 DEP and makes prognoses. The patient should discuss all questions with the attending physician and not take any action without his knowledge.
A neurologist diagnoses the disease
Who's at risk
It was previously thought that older people were more susceptible to DEP. Currently, the disease has become significantly “younger” and quite often it is diagnosed in patients who are under 50 years of age. In most cases, these are people of creative professions and mental work. The most severe consequences of discirculatory encephalopathy include senile dementia and ischemic stroke.
Factors that provoke the disease are: poor diet with a predominance of fatty and smoked foods, alcohol abuse, smoking, excess weight, hormonal disorders, high blood pressure, head injuries.
Causes of dyscirculatory encephalopathy
Atherosclerosis. Metabolic disorders lead to a decrease in the lumen of blood vessels, as a result of which the brain does not receive the required amount of oxygen and nutrients. Signs of discirculatory atherosclerotic encephalopathy:
- High blood pressure (hypertension) and low blood pressure (hypotension): in the first case, the vessels are excessively filled with blood, and insufficient filling is a consequence of hypotension.
- Osteocondritis of the spine. As a result of compression of the artery, the brain does not receive the amount of nutrients it needs.
- Injuries to the head and spine can cause hematomas that compress blood vessels, disrupting the nutrition of nerve cells.
- Smoking causes a narrowing of blood vessels, especially capillaries.
- Congenital pathologies.
- Vascular diseases.
- Hormonal disorders.
Definition of disease
DE
– this is rather a collective concept in medicine, since there is no such definition in the ICD tenth revision. Therefore, due to its similarity with clinical symptoms, it is most often associated with cerebral ischemia.
Methods for diagnosing dyscirculatory encephalopathy:
| Methods | Description |
| Angiography of head and neck vessels with contrast | Allows you to identify affected areas of blood vessels |
| Electroencephalography | Provides insight into the functional capacity of brain neurons |
| Magnetic resonance imaging | The most informative method for diagnosing microstrokes in ischemic areas |
| Fundus examination | Hemorrhages in the ocular retina and acute swelling of the optic nerve are detected, indicating intracranial hypertension |
| Doppler ultrasound | Allows you to identify blood clots and blocked areas in blood vessels |
The difficulty in determining the disease lies in the fact that several disease factors may play a role in one patient, such as:
Advertising:
- Excessive hypervasoconstriction of cerebral arteries. When, in response to an increase in systemic blood pressure, not a physiological reaction occurs - arterial spasm, but hyperconstriction, which exceeds this physiological reaction in severity.
- Cerebral microangiopathy. Which plays a role in hypertension, but can also be in diabetes mellitus, and in CVD - cerebrovascular disease.
- Insufficiency of collateral circulation. When even minor stenoses of the main vessels of the head can lead to cerebral ischemia.
- Deterioration of the rheological properties of blood.
- Impaired microcirculation at the cerebral level.
- The appearance of microemboli on the main vessels of the head. When a substrate (embolus) forms from an atherosclerotic plaque and clogs the small arteries of the brain, causing the formation of a lacunar infarction.
Advertising:
All these factors affect blood circulation in the brain, change the structure of the tissue, which affects its function. In this regard, three stages of the disease are determined, as well as several of its types, depending on the causes:
- Venous DE
. It is caused by stagnation of blood during outflow from the brain, which causes swelling of the brain vessels. - Hypertensive DE
. Characterized by frequent hypertensive crises. - Atherosclerotic DE
. The cause is cerebral atherosclerosis. The most common form of the disease.
DE of mixed type is a disease of complex genesis that combines several forms of the disease.
[media=
https://youtu.be/4hWZJpiFWq0
]
Symptoms of dyscirculatory encephalopathy of the brain, stage 1
The stage is characterized by a gradual increase in symptoms. Obvious manifestations of the disease are complaints of mood instability (from complete depression to sudden joy), apathy and depression. Unreasonable crying, headache, sleep disturbances, forgetfulness and attacks of aggression towards others are symptoms of stage 1 DEP of the brain. In some cases, patients may experience minor pain in the joints, back and stomach area.
On our website Dobrobut.com you will find more detailed information on this issue. You can make an appointment for a consultation by calling the numbers listed on the pages. At a personal appointment, the doctor will answer all questions and talk about the treatment of dyscirculatory encephalopathy of the 2nd degree of mixed origin.
Characteristics of the disease
Discirculatory encephalopathy stage 2. characterized by slow progression of brain dysfunction, which is associated with long-term insufficiency of its blood supply. DEP of the 2nd degree is a condition that develops as a result of a primary disease, which determines the secondary nature of the process of circulatory disorders. The pathogenesis is based on impaired blood flow in the brain tissue and dyscirculation (hemodynamic changes).
These mechanisms provoke hypoxic-ischemic processes and lead to hyperemia (overflow of blood vessels) of brain tissue. As a result of anoxia (lack of oxygen), functional disturbances in the functioning of the brain occur, and subsequently structural changes in the morphological structure of the brain matter occur. In the second case, the pathological processes are irreversible.
Discirculatory encephalopathy of the 2nd degree of complex genesis is a disease that reflects a multiform process of damage to brain tissue, which is caused by chronic cerebral circulatory failure or repeated episodes of acute disturbance of blood flow. Among the acute circulatory disorders, it is worth noting TIA (transistor ischemic attack) and stroke.
There are multifocal or diffuse (scattered) encephalopathy of the second degree. In the first case, instrumental diagnostics reveals multiple areas of tissue with necrotic changes. In the second case, the boundaries between foci of necrosis and healthy tissue are blurred and unclear. There are several variants of the course of the disease:
- Anomalies in the structure and deformation of blood vessels against the background of damage to large arteries and veins.
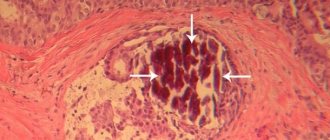
- Segmental dilatation (expansion) of blood vessels with the formation of aneurysms (persistently dilated areas in the blood flow system) against the background of damage to small vessels and arterioles due to the deposition of amyloid (protein) formations on the walls. The appearance of multiple small foci of cerebral infarction is characteristic.
- Thromboembolism (blockage of the lumen with a blood clot) against the background of atrial fibrillation, heart defects (congenital, acquired), myocardial infarction, aortic aneurysm.
- Hemostasiopathy (malfunction of the hemostasis system) due to pathological thickening of the blood.
- Arterial hypotension against the background of venous dysfunction and cardiac disorders.
Discirculatory hypertensive encephalopathy of the 2nd degree is one of the common diagnoses in neurological practice. The disease is accompanied by pathomorphological changes in brain tissue:
- Microgliosis (the process of replacing damaged or dead neurons with microglial cells).
- Astrogliosis (the process of replacing damaged or dead neurons with astrocytes).
- Demyelinating processes (destruction of the myelin sheath of nerve fibers).
- Decreased white matter density.
- Remodeling (change in structure) of capillaries.
Destructive processes that affect the structure of brain tissue provoke other large-scale disorders - leukoaraiosis (damage to the circulatory system supplying blood to the white matter), cortical atrophy with a subsequent increase in subarachnoid (under the arachnoid membrane) spaces, expansion of the cerebral ventricles.
Discirculatory encephalopathy 2nd degree - clinical manifestations
Without proper treatment, DEP of the 1st degree progresses to the second with all the ensuing consequences. Symptoms of grade 1 dyscirculatory encephalopathy of the brain include attention and memory disorders, and spatial orientation is disturbed. Complete apathy towards the outside world appears. In some cases, loss of ability to work may occur.
Stage 3 DEP is a severe degree of the disease, in which the patient loses the ability to perform purposeful actions and needs constant care. Characteristic manifestations are disturbances in speech and pelvic organ function, seizures, and movement disorders. The patient receives disability due to the diagnosis of dyscirculatory encephalopathy of the 3rd degree.
Clinical picture
DEP mainly manifests itself as disturbances in the emotional, cognitive and motor areas. The classic sign of the disease is memory loss.
Discirculatory encephalopathy always progresses, but the patient sometimes does not notice the increase in symptoms due to a decrease in the criticality of his own condition.
There are several key syndromes of the disease:
- Vestibular-coordinator (vestibulocerebellar, vestibuloatactic) syndrome manifests itself in the form of unsteadiness of gait, loss of coordination, dizziness, unsteadiness of walking, nystagmus (oscillations when walking);
- Pyramidal syndrome - positive pathological and high tendon, often asymmetrical reflexes;
- Cephalgic syndrome, in which headaches, dizziness, tinnitus and all symptoms associated with the head, nausea and vomiting are noted. With DEP, the intensity of headaches decreases as they progress;
- Astheno-neurotic syndrome: mood instability, tearfulness, sentimentality, depression, irritability, anxiety, apathy and a predominance of bad mood;
- Dissomnia syndrome - sleep disorders;
- Cognitive syndrome - cognitive impairment (memory loss, loss of concentration, absent-mindedness);
- Parkinsonian syndrome is characterized by the presence of slowness, a decrease in the length and increase in the frequency of steps, shuffling feet, trampling in place, and sliding steps. Weak facial expressions and slight muscle rigidity are also noted. Patients may fall frequently;
- Pseudobulbar syndrome manifests itself in the form of articulation disorders, problems with swallowing, episodes of forced laughter or crying, and reflexes of oral automatism.
Treatment of DEP
The main goal of drug therapy is to restore vascular function, improve blood flow to the brain and normalize the functioning of the nervous system. For this purpose, the patient is prescribed beta-blockers, calcium antagonists, vasodilators, neuroprotectors, and anticoagulants. This is general therapy. Symptomatic treatment is aimed at eliminating individual clinical manifestations, namely depression and behavioral lability.
Surgical intervention is recommended for severe progressive DEP (the degree of vasoconstriction is more than 70%).
How long can you live with dyscirculatory encephalopathy of complex origin?
There is no clear answer. It all depends on the degree of the disease, symptoms, drug therapy, etc. The prognosis is favorable if DEP is detected early. Timely treatment and strict adherence to the doctor’s recommendations will help slow down the development of pathology, and in some cases, stop it.
If you are interested in the question of how long you can live with discirculatory encephalopathy of complex origin, make an appointment with our specialist.
Related services: Computed tomography Encephalogram of the brain