The functions of cells in the nervous system are very diverse. One type is a motor neuron (motoneuron). Its name translated from Latin means “sets in motion.” It is through this that muscle contraction occurs.
The peculiarity of motor nerve cells is that their cytoplasm does not evenly surround the nucleus, but forms two processes. One of them is shorter (dendrite) receives a nerve impulse, the second (axon) transmits it further.
Thus, the peripheral motor neuron conducts nerve impulses from the central nervous system to the muscle. In muscle tissue, its long process branches and connects with dozens of muscle fibers.
Motor neuron disease
The mechanism of this condition is not fully understood, but it has been established that the disease tends to progress and is often chronic.
The disease represents degenerative changes in motor neurons. Damage to the nerve endings responsible for movement will eventually lead to gait disturbances, but coordination does not suffer. In case of untimely diagnosis, the disease ends in paralysis.
Spinal motor neurons are the first to react, this leads to the death of nerve fibers, and muscle weakness increases. In advanced cases, the disease can be fatal.
- Artificial stimulation of a nerve cell[edit | edit code]
- Peripheral motor neurons (alpha and gamma motor neurons)
- Location
- Motor neuron disease: causes, symptoms and what to do
- Connections
- Who can get sick
- Interaction with neurotransmitters
- Bibliography
- Properties and functions of neurons
- Signals
Artificial stimulation of a nerve cell[edit | edit code]
When an electrical impulse from an external source is applied to a nerve cell, current flows from the positively charged electrode (anode) and exits to the negatively charged electrode [cathode]. The nerve fiber below the cathode depolarizes and, provided the threshold potential is reached, an action potential is generated.
The speed of conduction of an impulse along a nerve can be measured by placing two electrodes on the skin along the nerve at a known distance from each other, then stimulating that nerve (containing numerous neurons) and recording the time it takes for the total action potential to travel the distance between the electrodes. The speed of signal transmission in humans is usually from 40 to 70 m/s. Values below 40 m/s are considered pathological.
Accidental exposure to electricity. High voltage, especially low-frequency alternating current (for example, from an electrical outlet), and also under conditions of reduced resistance (bare feet, accident in the bathroom), mainly affects the conduction of signals in the heart, which can cause ventricular fibrillation.
Direct current usually acts as a stimulus only when switched on and off: high-frequency alternating current (> 15 kHz), in contrast, is not capable of causing depolarization, but damages body tissues. Diathermy is based on this principle.
Peripheral motor neurons (alpha and gamma motor neurons)
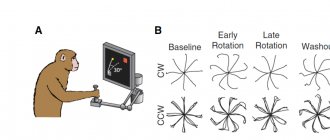
Peripheral motor neurons are divided into alpha motor neurons and gamma motor neurons (Fig. 21.2).
Smaller gamma motor neurons innervate intrafusal muscle fibers. Activation of gamma motor neurons increases the stretch of muscle spindles, thereby facilitating tendon and other reflexes through alpha motor neurons.
Each muscle is innervated by several hundred alpha motor neurons. In turn, each alpha motor neuron innervates many muscle fibers - about twenty in the extrinsic muscles of the eye and hundreds in the muscles of the limbs and trunk.
Acetylcholine is released at neuromuscular junctions.
The axons of peripheral motor neurons are part of the cranial nerves and the anterior roots of the spinal cord. At the level of the intervertebral foramina, the anterior roots and dorsal roots fuse to form the spinal nerves. Several adjacent spinal nerves form a plexus and then branch into peripheral nerves. The latter also branch repeatedly and innervate several muscles. Finally, the axon of each alpha motor neuron forms numerous branches, innervating many muscle fibers.
Each alpha motor neuron receives direct excitatory glutamatergic inputs from cortical motor neurons and from sensory neurons innervating the muscle spindles. Exciting influences also come to alpha and gamma motor neurons from the motor nuclei of the brain stem and interneurons of the spinal cord - both through direct pathways and with switches.
Direct postsynaptic inhibition of alpha motor neurons is carried out by Renshaw cells - intercalary glycinergic neurons. Indirect presynaptic inhibition of alpha motor neurons and indirect presynaptic inhibition of gamma motor neurons are provided by other neurons that form GABAergic synapses on dorsal horn neurons.
Other interneurons of the spinal cord, as well as motor nuclei of the brain stem, also have an inhibitory effect on alpha and gamma motor neurons.
If excitatory inputs predominate, a group of peripheral motor neurons are activated. First, small motor neurons are excited. As the force of muscle contraction increases, the frequency of their discharges increases and large motor neurons are involved. With maximum muscle contraction, the entire corresponding group of motor neurons is excited.
Central motor neuron
SYNDROMES
- Syndromes of central motor neuron damage.
Having established that a patient has paralysis (or paresis) caused by a disease of the nervous system, they first try to find out the nature of the paralysis (or paresis): whether it depends on damage to the central neuron of the motor pathway or the peripheral one. Recall that the central neuron of the main pathway for voluntary movements begins in the motor zone of the cerebral cortex, at the pyramidal cells, passes through the internal bursa and brain stem and ends at the cells of the anterior horns of the spinal cord or at the nuclei of the motor cranial nerves.
The peripheral neuron goes from the cell of the anterior horn of the spinal cord or the nucleus of the cranial nerve to the muscle.
Wherever this motor pathway is interrupted, paralysis will occur. Damage to the central neuron will result in central paralysis, while damage to the peripheral neuron in peripheral paralysis.
The clinical features of central and peripheral paralysis are so different from each other that in the vast majority of cases it is possible to easily differentiate one type of paralysis from another.
Signs of central paralysis - increased tendon and periosteal reflexes, muscle tone, the appearance of pathological, protective reflexes, clonus and unusual friendly movements - are easily explained by the essence of the process.
The intensity of Paresis can be very different. In mild cases, it is necessary to resort to some special techniques to identify the existing weakness of the limb. Suspecting, for example, the subject has weakness in one hand, you can ask him to clench his hands into fists and unclench them many times in a row, repeatedly finger the fingers of both hands with his thumb.
- Semiotics of peripheral motor neuron lesions.
Semiotics of movement disorders. Having identified, based on a study of the volume of active movements and their strength, the presence of paralysis or paresis caused by a disease of the nervous system, its nature is determined: whether it occurs due to damage to central or peripheral motor neurons. Damage to central motor neurons at any level of the corticospinal tract causes central, or spastic, paralysis. When peripheral motor neurons are damaged at any site (anterior horn, root, plexus and peripheral nerve), peripheral or flaccid paralysis occurs.
Central motor neuron
: damage to the motor area of the cerebral cortex or pyramidal tract leads to the cessation of the transmission of all impulses for voluntary movements from this part of the cortex to the anterior horns of the spinal cord. The result is paralysis of the corresponding muscles. If the pyramidal tract is interrupted suddenly, the muscle stretch reflex is suppressed. This means that the paralysis is initially flaccid. It may take days or weeks for this reflex to return.
When this happens, the muscle spindles will become more sensitive to stretching than before. This is especially evident in the arm flexors and leg extensors. Stretch receptor hypersensitivity is caused by damage to the extrapyramidal tracts, which terminate in the anterior horn cells and activate gamma motor neurons that innervate intrafusal muscle fibers. As a result of this phenomenon, the impulse through the feedback rings that regulate muscle length changes so that the arm flexors and leg extensors are fixed in the shortest possible state (minimum length position). The patient loses the ability to voluntarily inhibit overactive muscles.
Spastic paralysis always indicates damage to the central nervous system, i.e. brain or spinal cord. The result of damage to the pyramidal tract is the loss of the most subtle voluntary movements, which is best seen in the hands, fingers, and face.
The main symptoms of central paralysis are: 1) decreased strength combined with loss of fine movements; 2) spastic increase in tone (hypertonicity); 3) increased proprioceptive reflexes with or without clonus; 4) reduction or loss of exteroceptive reflexes (abdominal, cremasteric, plantar); 5) the appearance of pathological reflexes (Babinsky, Rossolimo, etc.); 6) protective reflexes; 7) pathological friendly movements; lack of reaction of degeneration.
2) spastic increase in tone (hypertonicity); 3) increased proprioceptive reflexes with or without clonus; 4) reduction or loss of exteroceptive reflexes (abdominal, cremasteric, plantar); 5) the appearance of pathological reflexes (Babinsky, Rossolimo, etc.); 6) protective reflexes; 7) pathological friendly movements; lack of reaction of degeneration.
Symptoms vary depending on the location of the lesion in the central motor neuron. Damage to the precentral gyrus is characterized by two symptoms: focal epileptic seizures (Jacksonian epilepsy) in the form of clonic seizures and central paresis (or paralysis) of the limb on the opposite side. Paresis of the leg indicates damage to the upper third of the gyrus, the arm to its middle third, half of the face and tongue to its lower third. It is diagnostically important to determine where clonic seizures begin. Often, convulsions, starting in one limb, then move to other parts of the same half of the body. This transition occurs in the order in which the centers are located in the precentral gyrus. Subcortical (corona radiata) lesion, contralateral hemiparesis in the arm or leg, depending on which part of the precentral gyrus the lesion is closer to: if it is in the lower half, then the arm will suffer more, and in the upper half, the leg. Damage to the internal capsule: contralateral hemiplegia. Due to the involvement of corticonuclear fibers, there is a disruption of innervation in the area of the contralateral facial and hypoglossal nerves. Most cranial motor nuclei receive pyramidal innervation on both sides, either completely or partially. Rapid damage to the pyramidal tract causes contralateral paralysis, initially flaccid, since the lesion has a shock-like effect on the peripheral
- Syndrome of transverse lesion of the cervical thickening of the SM.
When the spinal cord is interrupted at the upper cervical level (CI - CIV), the following appears:
- spastic tetraplegia (spastic paralysis of all four limbs) due to bilateral damage to the descending motor tracts, bilateral peripheral (flaccid) paralysis of the muscles of the corresponding myotome (muscles of the occipital region) due to damage to the peripheral motor neurons of the anterior horns, as well as flaccid paralysis of the sternocleidomastoid muscles and upper parts of the trapezius muscles as a result of damage to the spinal portion of the nucleus of the XI pair (n. accesorius), bilateral peripheral paralysis of the diaphragm due to damage to the peripheral motor neurons of the anterior horns of the spinal cord at the level CIII–CIV, the axons of which form the phrenic nerve (n. phrenicus) with the development of acute syndrome respiratory failure or the appearance of a paradoxical type of breathing (when inhaling, the anterior abdominal wall retracts, and when exhaling, it protrudes;
- loss of all types of sensitivity of the conductor type, i.e. below the level of the lesion according to the principle of “everything below” with bilateral damage to all sensitive conductors, as well as of the segmental type in the corresponding sclerotomes (the scalp of the occipital region);
- bilateral dissociated anesthesia of the lateral areas of the face, i.e. loss of superficial types of sensitivity - temperature ( termanesthesia ) and pain ( analgesia ) while maintaining deep types of sensitivity (spatial skin sensitivity) in the posterior dermatomes of Zelder ( "onion" type of sensory disorders) with damage to the lower segment of the nucleus of the spinal tract of the trigeminal nerve (nucl. spinalis n. trigemini);
- dysfunction of the pelvic organs of the central type, which are manifested by acute retention of urine (retentio urinae), feces (retentio alvi) or periodic incontinence of urine (incontinentio intermittens urinae) and feces (incontinentio intermittens alvi). This occurs because the influence of the central neurons of the precentral gyrus, located on the medial surface of the frontal lobe, in the paracentral lobule, is lost, and the peripheral somatic regulation of the function of the pelvic organs is carried out at the level of segments SIII–SV of the spinal cord, where motor neurons are located in the anterior horns of the gray matter, innervating the striated muscles of the pelvic organs (external sphincters). Moreover, with a complete transverse lesion of the spinal cord, the principle of bilateral cortical innervation of the pelvic organs is lost.
Location
Alpha motor neurons innervating the head and neck are located in the brain stem; The α-MNs that innervate the rest of the body are located in the spinal cord. There are more α-MNs in the spinal cord than in the brain stem, because the amount of α-MN is directly proportional to the accuracy of control over the work of an individual muscle. For example, the finger muscles have a higher number of α-MNs per fiber and a higher total number of α-MNs than the quadriceps femoris, allowing for finer control of the fingers.
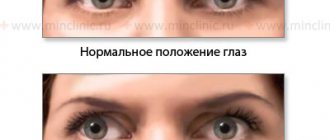
Typically, α-MNs located on one side of the brainstem or spinal cord innervate muscles located on the same side of the body. An exception is the trochlear nerve nuclei, located in the brainstem, which innervate the superior oblique muscle of the eye on the opposite side of the face.
Brain stem
In the brainstem, α-MNs and other neurons are found within clusters of cells called nuclei
, some of which contain cell bodies of neurons belonging to cranial nerves.
Not all cranial nerve nuclei contain α-MNs; on this basis, the nuclei are divided into motor
and
sensory
.
Important Therapeutic and preventive medications for Alzheimer's disease
Typically, motor nuclei located higher in the brainstem (i.e., more rostral) innervate muscles located higher on the face. For example, oculomotor nerve nuclei containing α-MNs that innervate the ocular muscles are located in the midbrain, the most rostral component of the brainstem. On the other hand, the hypoglossal nerve nucleus, which contains α-MNs that innervate the tongue, is located in the medulla oblongata, the most caudal (i.e., located towards the bottom) of the brainstem structures.
Spinal cord
The pyramidal tract is one of the main descending pathways from the brain to the α-MNs of the spinal cord.
In the spinal cord, α-MNs are located in the gray matter of the anterior horns. These α-MNs provide the motor component of the spinal nerves that innervate the muscles of the body.
Alpha motor neurons are located in lamina IX according to the Rexed system.
As in the brainstem, the overlying segments of the spinal cord contain α-MNs that innervate muscles higher up on the body. For example, the biceps brachii muscle, a muscle of the arm, is innervated by α-MNs located in spinal cord segments C5, C6, and C7, which are located in the rostral (upper) part of the spinal cord. On the other hand, the gastrocnemius muscle, one of the leg muscles, is innervated by α-MNs located within the S1 and S2 segments, which are located in the caudal (lower) part of the spinal cord.
Alpha motor neurons are located in a specific region of the gray matter of the spinal cord. This region belongs to lamina IX of the Rexed lamina system, which classifies gray matter regions based on their cytoarchitecture. Plate IX is located predominantly in the medial part of the ventral (anterior) horn, although some of its parts lie within plates VII and VIII. Like other regions of the spinal cord, the cells of this plate are organized somatotopically, meaning that the position of neurons in the spinal cord is related to which muscles they innervate. In particular, α-MNs in the medial zone of lamina IX tend to innervate proximal muscles of the body, whereas neurons in the lateral zone typically innervate more distal muscles. In addition, there is somatotropia associated with α-MNs innervating the flexors and extensors: α-MNs innervating the flexor muscles are usually located in the dorsal part of lamina IX; those that innervate the extensors tend to be located more ventrally.
Motor neuron functions
Central and peripheral motor nerve cells work in concert. Together they provide contraction of certain muscle groups and allow a person to perform any action.
For coordinated movements of the limbs, simultaneous contraction of the flexors and extensors is necessary. When the flexors work, the initial excitation signal arises in the area of the precentral gyrus of the corresponding hemisphere.
Cells called pyramidal cells are responsible for this action. Their processes collected together form the so-called pyramidal motor pathway. Next, the signal goes to the anterior horns of the spinal cord, from where it is transmitted directly to the myofibrils.
Special centers of the posterior sections of the cerebral hemispheres have an activating effect on the motor neurons of the extensor muscles. They form the dorsal and ventral pathways. Thus, two areas of the brain are involved in the formation of coordinated movement.
Based on the nature of their function, the nerve cells involved in the process of muscle contraction are divided into motor neurons and interneurons. The former are responsible for the executive function, while the intercalary ones serve to coordinate nerve impulses. This particular variety is smaller in size and more numerous.
Article on the topic: DMT: effectiveness of therapy for multiple sclerosis
For comparison, in the area of the anterior horns there are 30 times more of them than motor horns. When excitation is carried out along the axon of the motor nerve, it initially passes to the interneuron. Depending on the nature of the signal, it can be amplified or weakened, after which it is transmitted further.
Intercalated cells have more processes and are more sensitive. They have a large number of processes and are also called multipolar.
To optimize the signals emanating from the axons and going to the muscle fibers, special Renshaw cells are used, which transmit excitation from one process to another. This mechanism serves to equalize the intensity of the nerve signal.
Along the process of the motor neuron, the impulse reaches the muscle fiber, which contracts. Each group of motor neurons and the muscle fibers they innervate are responsible for specific movements.
Nerve cells providing motor function:
| Types of neurons | Localization | Function |
| central innervating flexors | precentral gyrus area | contraction of skeletal flexor muscles by transmitting impulse to the anterior horns |
| central innervating extensors | hindbrain region | contraction of skeletal extensor muscles by transmitting impulses to the anterior horns |
| peripheral alpha | anterior horn of the spinal cord | direct contraction of skeletal muscles |
| peripheral gamma | anterior horn of the spinal cord | regulation of tone |
| insertion | all parts of the central nervous system | communication of signals within the central nervous system |
Large alpha neurons conducting a strong impulse cause myofibril contraction. Small ones conduct weak signals and serve to maintain muscle tone.
In addition to the fibers responsible for contraction, muscle tissue also contains special spiral fibrils that regulate the force of muscle tension.
These extrafusal muscle fibers are innervated by gamma neurons.
Excitation of the gamma motor neuron leads to an increase in the stretch of myofibrils and facilitates the passage of the tendon reflex impulse. An example would be the passage of a nerve signal along the arc of the knee reflex.
The coordinated work of peripheral motor neurons achieves fine tuning of muscle tone, which allows for precise coordinated movements. When peripheral motor neurons are damaged, muscle tone disappears and movement is impossible.
Motor neuron disease: causes, symptoms and what to do
This disease, which is characterized by the progression of degeneration of the corticospinal tracts, anterior horn neurons and motor nuclei, is quite rare among patients. It has special symptoms, if they occur, it is recommended to consult a neurologist.
After a thorough examination, treatment is prescribed. The effectiveness of therapy depends on the correct diagnosis. Treatment will depend on the symptoms present. If you ignore this pathology of the nervous system, it can lead to death.
Causes of the disease
In modern medicine, several forms of the disease are identified, but the causes of their occurrence have not yet been precisely established. It is also unknown why only motor neurons are affected.
The most common factors that can provoke pathology include:
- Triggering damaged neurons that are under the influence of glutamate.
- Excessive intake of calcium ions into cells, which leads to a violation of the ratio of intracellular and extracellular calcium.
- Lack of neurotrophic factors.
- Autoimmune processes.
- Exposure to exotoxins.
- Tobacco smoking.
Forms
In modern medicine, there are several forms of this pathology, which differ in their special symptoms:
- Amyotrophic lateral sclerosis. It is considered the most common form of the disease. Accompanied by the gradual manifestation of the following symptoms: painful cramps of the limbs, weakness in the arms and legs, fasciculation, spasticity, stiffness of movement, weight loss. Then fatigue sets in and it is difficult to control facial expressions and tongue movements. Death occurs due to paralysis of the respiratory muscles.
- Progressive boulevard palsy. Accompanied by difficulty chewing, swallowing, speaking, voice changes, fasciculation and weakness of facial expressions and tongue are noted. The survival rate for this form of pathology is low.
- Progressive muscular atrophy. Refers to a hereditary disease. Develops at any age and progresses slowly. An early manifestation is fasciculation. Weakness is noted first in the arms, then in the shoulders and legs. Survival rate is more than 23 years.
Diagnosis and treatment
At the first manifestations of pathology, you should immediately contact a specialist and undergo a full examination. If the patient notices progressive generalized motor weakness, which is simultaneously accompanied by significant deviations in sensitivity, then these are the first alarming signs of the disease.
The examination includes:
- Needle EMG. Considered to be informative methods.
- Study of the speed of excitation.
- Laboratory tests. A complete blood test is required to determine the level of electrolytes, protein, and thyroid hormones.
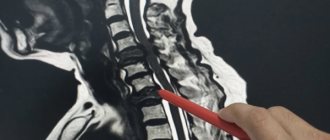
- Magnetic resonance imaging of the cervical spine. It is carried out only if there are no clinical and EMG data indicating damage to the cranial nerves.
As for treatment, there is no specific therapy. The patient is prescribed:
- "Riluzole", which must be taken regularly twice a day. Helps relieve the bulbar form of amyotrophic lateral sclerosis.
- "Baclofen."
- "Glycopyrropate", "Amtriptyline".
- "Fluvoxamine."
Important Healing herbs that help against insomnia: list and recipes
In later stages of the disease, opioids and benzodiazepines may be prescribed.
To help the patient overcome neurological abnormalities of this nature, it is also worth paying attention to the following methods:
- Physiotherapy. Supports muscle function. It is recommended to use orthopedic bandages that have a fixing function.
- Consultation and sessions with a speech therapist. Helps you select communication devices that will facilitate the communication process.
- Percutaneous endoscopic gastrostomy.
- Non-invasive respiratory support. Prescribed for respiratory weakness.
Surgical intervention to facilitate swallowing is performed in rare cases, as it is considered ineffective.
Motor neuron disease is a serious neurological pathology that leads not only to serious consequences, but even to death. It is advisable to carry out timely diagnosis and treatment.
Symptoms of central motor neuron damage
Damage to central motor nerve cells most often occurs during stroke. When ischemia or hemorrhage occurs in the substance of the cerebral hemispheres, a section of tissue dies. Such lesions are almost always unilateral.
As a result, when central motor neurons are damaged, muscle dysfunction on one side is observed. The most noticeable symptom is unilateral paralysis, leading to the inability to actively move the arm and leg.
On the same side, muscle tone in the torso and facial muscles decreases. Damage to the central motor areas is accompanied by a number of changes in reflex activity.
Clinically, this is expressed in the appearance of various pathological reflexes. Their combination, decreased muscle tone and sensory disturbances allow the doctor to make a diagnosis.
Connections
Like other neurons, lower motor neurons have both afferent (incoming) and efferent (outgoing) connections. Alpha motor neurons receive afferent innervation from a number of sources, including upper motor neurons, sensory neurons, and interneurons. In turn, α-MN innervate extrafusal muscle fibers. These afferent and efferent connections are involved in the coordination of muscle activity.
Afferent input
Some pathways between upper motor neurons and alpha motor neurons
| Location of the VMN | Location of α-MN | Path name |
| Brain | Brain stem | Corticonuclear pathway |
| Brain | Spinal cord | Pyramidal tract |
| Red core | Spinal cord | Red nuclear spinal tract |
| Vestibular nuclei | Spinal cord | vestibulospinal tract |
| Roof of the midbrain | Spinal cord | Tectospinal tract |
| Reticular formation | Spinal cord | Reticular spinal tract |
Upper motor neurons (UMNs) send axons to α-MNs through several pathways, including (but not limited to) the corticonuclear, pyramidal, and red nuclear spinal tracts.
The corticonuclear tract connects the cerebral cortex with the nuclei of the cranial nerves. (The corticonuclear tract is also called the corticobulbar tract
.) It is a bundle of upper motor neuron axons that descends from the cortex and terminates at synapses on brainstem α-MNs. Similarly, cortical UMNs directly control α-MNs in the spinal cord through the lateral and ventral corticospinal tracts.
Afferent (sensory) input to α-MNs is extensive and originates in Golgi tendon organs, muscle spindles, mechanoreceptors, thermoreceptors, and other sensory neurons in the periphery. These connections form the structure of neural circuits that underlie reflexes. There are several types of reflex circuits, the simplest of which consists of a single synapse between a sensory neuron and an α-MN. The knee jerk reflex is an example of such a monosynaptic reflex.
The most significant afferentation comes to α-MNs from local interneurons, which are the most abundant type of neurons in the spinal cord. In addition to the many other functions they perform, interneurons send axons to α-MNs, which create more complex reflex circuits. One type of interneuron is the Renshaw cell, which will be discussed below.
Efferent output
Alpha motor neurons send out axons that mainly terminate at synapses on extrafusal muscle fibers. Some α-MN axons terminate on Renshaw cells, inhibitory interneurons that send axons to α-MNs and limit their activity to prevent muscle damage.
Reflex-motor sphere: general concepts
1. Terminology:
– Reflex – is the body’s reaction to a stimulus, realized with the participation of the nervous system.
– Tone is a reflex muscle tension that ensures the preservation of posture and balance and preparation for movement.
2. Classification of reflexes
– By origin:
1) unconditional (constantly occurring in individuals of a given species and age with adequate stimulation of certain receptors);
2) conditional (acquired during an individual’s life).
– By type of stimulus and receptor:
1) exteroceptive (touch, temperature, light, sound, smell),
2) proprioceptor (deep) are divided into tendon, which arise when muscles are stretched, and tonic, to maintain the position of the body and its parts in space.
3) interoreceptor.
– According to the level of arc closure: spinal; stem; cerebellar; subcortical; cortical.
– According to the effect caused: motor; vegetative.
3. Types of motor neurons:
– Alpha large motor neurons - performing fast (phasic) movements (from the motor cortex);
– Alpha small motor neurons - maintaining muscle tone (from the extrapyramidal system), are the first link of the gamma loop;
– Gamma motor neurons - maintaining muscle tone (from muscle spindle receptors), are the last link of the gamma loop - are involved in the formation of the tonic reflex.
4. Types of proprioceptors:
– Muscle spindles - consist of intrafusal muscle fiber (similar to embryonic fibers) and the receptor apparatus, excited during relaxation (passive lengthening) of the muscle and inhibited during contraction (parallel activation with the muscle) :
1) phasic (1 type of receptors - annulo-spiral, “core-chain”), activated in response to sudden lengthening of the muscle - the basis of tendon reflexes,
2) tonic (type 2 receptors - cluster-shaped, “bursa-nuclei”), activated in response to slow lengthening of the muscle - the basis for maintaining muscle tone.
– Golgi receptors - an afferent fiber located among the connective tissue fibers of the tendon - are excited when the muscle is tense and inhibited when relaxing (sequential activation with the muscle) - inhibits overstretching of the muscle.
Who can get sick
Until now, science does not have answers to many questions regarding this disease. Here's what you can say for sure about MND:
- Motor neuron disease is not infectious and is not contagious.
- MND can affect any adult, but most people diagnosed with the disease are over 40 years of age, and the disease is most common between the ages of 50 and 70.
- Men are affected by this disease more often than women.
- The incidence of MND is 2 new cases per 100,000 population per year.
- The prevalence of MND is approximately 5–7 people per 100,000 population.
The triggers underlying each individual case of ALS may be different. There are hereditary forms in which the disease is transmitted from ancestors, and then the main cause is a breakdown in a specific gene. However, in most cases, the patient does not have relatives suffering from this disease. Scientists believe that the disease is caused by many factors, both hereditary and environmental, which individually slightly increase the risk of the disease, but together can tip the scales in its favor.
Amyotrophic lateral sclerosis is a chronic, slowly progressive neurodegenerative disease of the central nervous system. It is characterized by damage to the central and peripheral motor neuron, the main participant in conscious human movements. J. Charcot was the first to describe this disease in 1869. Synonyms for the disease: motor neuron disease, motor neuron disease, Charcot's disease or Lou Gehrig's disease. ALS, like one of many other neurodegenerative diseases, progresses slowly and is difficult to treat.
The average life expectancy after the onset of the pathological process is 3 years. The life prognosis depends on the form: in some variants the life expectancy does not exceed two years. However, less than 10% of patients live longer than 7 years. There are known cases of longevity in amyotrophic lateral sclerosis. Thus, the famous physicist and popularizer of science Stephen Hawking lived 76 years: he lived with the disease for 50 years. Epidemiology: the disease affects 2-3 people per 1 million population in one year. The average age of the patient is from 30 to 50 years. Statistically, women get sick more often than men.
Important Mental states. reactive and stable states (page 1 of 2)
Reflex-motor sphere: symptoms of damage
1. Symptoms of loss
— Peripheral paralysis develops when a peripheral motor neuron is damaged in any area; symptoms are caused by a weakening of the level of segmental reflex activity:
1) decreased muscle strength,
2) muscle Areflexia (hyporeflexia) - a decrease or complete absence of deep and superficial reflexes.
3) muscle atony - decreased muscle tone,
4) muscle atrophy - decrease in muscle mass,
+ fibrillar or fascicular twitching (symptom of irritation) - spontaneous contractions of muscle fibers (fibrillar) or groups of muscle fibers (fascicular) - a specific sign of damage to the body of a peripheral neuron.
— Central paralysis (unilateral damage to the pyramidal tract) develops when the central motor neuron is damaged in any area; symptoms are caused by an increase in the level of segmental reflex activity:
1) decreased muscle strength,
2) hyperreflexia of tendon reflexes with expansion of reflexogenic zones.
3) reduction or absence of superficial (abdominal, cremasteric and plantar) reflexes
4) clonus of the feet, hands and kneecaps - rhythmic muscle contractions in response to tendon stretching.
5) pathological reflexes:
- Foot flexion reflexes - reflex flexion of the toes:
- Rossolimo - a short, jerky blow to the tips of the 2-5 toes,
- Zhukovsky - a short jerky blow with a hammer in the middle of the patient’s foot,
- Hoffman - pinching irritation of the nail phalanx of the II or III toes,
- Ankylosing spondylitis - a short jerky blow with a hammer on the back of the foot in the area of 4-5 metatarsal bones,
- Ankylosing spondylitis heel - a short jerky blow with a hammer on the heel.
- Foot extensor reflexes - the appearance of extension of the big toe and fan-shaped divergence of 2-5 toes:
- Babinsky - moving the handle of the hammer along the outer edge of the foot,
- Oppenheim - passing along the anterior edge of the tibia,
- Gordon - compression of the calf muscles,
- Schaeffer - compression of the Achilles tendon,
- Chaddok - streak irritation around the outer ankle,
- Carpal analogues of flexion reflexes - reflex flexion of the fingers (thumb):
- Rossolimo - a jerky blow to the tips of the 2-5 fingers of the hand in a pronated position,
- Hoffman - pinching irritation of the nail phalanx of the II or III fingers of the hand (1), IV or V fingers of the hand (2),
- Zhukovsky - a short jerky blow with a hammer in the middle of the patient’s palm,
- Bekhtereva - a short jerky blow with a hammer on the back of the hand,
- Galanta - a short jerky blow with a hammer on the tenar,
- Jacobson-Lask - a short jerky blow with a hammer on the styloid process.
6) protective reflexes: Bekhterev-Marie-Foy - with sharp painful flexion of the toes, “triple flexion” of the leg occurs (in the hip, knee and ankle joints).
7) muscle hypertension - increased muscle tone of a spastic type (the “jackknife” symptom is determined - with passive extension of a bent limb, resistance is felt only at the beginning of the movement), development of contractures, Wernicke-Mann posture (flexion of the arm, extension of the leg)
 pathological synkinesis - involuntary friendly movements that accompany the performance of active actions ( physiological - waving arms while walking, pathological - occur in a paralyzed limb due to the loss of inhibitory influences of the cortex on intraspinal automatisms:
pathological synkinesis - involuntary friendly movements that accompany the performance of active actions ( physiological - waving arms while walking, pathological - occur in a paralyzed limb due to the loss of inhibitory influences of the cortex on intraspinal automatisms:
- global - change in the tone of the injured limbs in response to prolonged muscle tension on the healthy side (sneezing, laughing, coughing) - shortening in the hand (flexion of the fingers and forearm, shoulder abduction), lengthening in the leg (hip adduction, leg extension, foot flexion),
- coordinator - involuntary contractions of paretic muscles with voluntary contraction of functionally associated muscles (Strumpel's tibial phenomenon - dorsiflexion is impossible, but appears when bending the knee joint; Raymist's symptom - does not adduct the leg at the hip, but when the healthy leg is adducted, movement occurs in paretic; Babinski phenomenon - standing up without the help of hands - a healthy and paretic leg rises),
- imitation - involuntary movements of a paretic limb, imitating volitional movements of a healthy one.
— Central paralysis (bilateral damage to the pyramidal tract):
+ dysfunction of the pelvic organs of the central type - acute urinary retention when the pyramidal tract is damaged, followed by periodic urinary incontinence (reflex emptying of the bladder during overdistension), accompanied by an imperative urge to urinate.
— Central paralysis (unilateral lesion of the corticonuclear pathway): according to the rule of 1.5 nuclei, only the lower ½ nucleus of the facial nerve and the nucleus of the hypoglossal nerve have unilateral cortical innervation:
1) smoothness of the nasolabial fold and drooping of the corner of the mouth on the side opposite to the lesion,
2) deviation of the tongue in the direction opposite to the lesion (deviation is always towards the weak muscles).
— Central palsy (bilateral damage to the corticonuclear pathway):
1) decrease in muscle strength of the muscles of the pharynx, larynx, tongue (dysphagia, dysphonia, dysarthria);
2) strengthening of the chin reflex;
3) pathological reflexes = reflexes of oral automatism:
- Sucking (Oppenheim) - sucking movements with line irritation of the lips,
- Proboscis - a blow with a hammer on the upper lip causes the lips to be pulled forward or the orbicularis oris muscle to contract,
- Nasolabial (Astvatsaturova) - a blow with a hammer to the back of the nose causes the lips to be pulled forward or the orbicularis oris muscle to contract,
- Distance-oral (Karchikyan) - bringing the hammer to the lips causes the lips to be pulled forward,
- Palmomental (Marinescu-Radovici) - line irritation of the thenar skin causes contraction of the mental muscle on the same side.
2. Symptoms of irritation
— Jacksonian epilepsy – paroxysmal clonic convulsions of individual muscle groups, with possible spread and secondary generalization (most often from the thumb (maximum zone of representation in the precentral gyrus) – other fingers – hand – upper limb – face – whole body = Jacksonian march)
— Kozhevnikov epilepsy ( epilepsia partialis continua) – constant convulsions (myoclonus in combination with torsion dystonia, choreoathetosis) with periodic generalization (chronic tick-borne encephalitis)
Interaction with neurotransmitters
Neurons of different locations communicate with each other using electrical impulses of a chemical nature. So, what is the basis of their education? There are so-called neurotransmitters (neurotransmitters) - complex chemical compounds. On the surface of the axon there is a nerve synapse - the contact surface. On one side there is a presynaptic cleft, and on the other there is a postsynaptic cleft. Between them there is a gap - this is the synapse. On the presynaptic part of the receptor there are sacs (vesicles) containing a certain amount of neurotransmitters (quanta).
When the impulse approaches the first part of the synapse, a complex biochemical cascade mechanism is initiated, as a result of which the sacs with mediators are opened, and quanta of mediator substances smoothly flow into the gap. At this stage, the impulse disappears and reappears only when the neurotransmitters reach the postsynaptic cleft. Then biochemical processes are activated again with the opening of the gates for mediators and those, acting on the smallest receptors, are converted into an electrical impulse that goes further into the depths of the nerve fibers.
Meanwhile, different groups of these same neurotransmitters are distinguished, namely:
- Inhibitory neurotransmitters are a group of substances that exert an inhibitory effect on excitation. These include: gamma-aminobutyric acid (GABA);
- glycine.
- acetylcholine;
Bibliography
- ICD-10 (International Classification of Diseases)
- Yusupov Hospital
- Batueva E.A., Kaygorodova N.B., Karakulova Yu.V. The influence of neurotrophic therapy on neuropathic pain and the psycho-vegetative status of patients with diabetic neuropathy // Russian Journal of Pain. 2011. No. 2. P. 46.
- Boyko A.N., Batysheva T.T., Kostenko E.V., Pivovarchik E.M., Ganzhula P.A., Ismailov A.M., Lisinker L.N., Khozova A.A., Otcheskaya O .V., Kamchatnov P.R. Neurodiclovit: possibility of use in patients with back pain // Farmateka. 2010. No. 7. pp. 63–68.
- Morozova O.G. Polyneuropathy in somatic practice // Internal medicine. 2007. No. 4 (4). pp. 37–39.
Properties and functions of neurons
Properties:
- The presence of a transmembrane potential difference
(up to 90 mV), the outer surface is electropositive with respect to the inner surface. - Very sensitive
to certain chemicals and electrical current. - The ability to neurosecretion
, that is, to synthesize and release special substances (neurotransmitters) into the environment or synaptic cleft.
High energy consumption, high level of energy processes, which necessitates a constant influx of main energy sources - glucose and oxygen, necessary for oxidation.
Functions:
- Receiving function
(synapses are contact points; we receive information in the form of an impulse from receptors and neurons). - Integrative function
(information processing, as a result, a signal is generated at the neuron output that carries information from all summed signals). - Conductor function
(information flows from the neuron along the axon in the form of electric current to the synapse). - Transmitting function
(a nerve impulse, having reached the end of an axon, which is already part of the structure of the synapse, causes the release of a mediator - a direct transmitter of excitation to another neuron or executive organ).
How does a motor neuron work?
In order for a bioelectric impulse to occur, a potential difference is required on the membrane of the nerve cell. This occurs as a result of changes in the concentration of potassium and sodium ions from the outer and inner surfaces of the membrane.
Subsequently, the impulse travels to the end of the long process, the axon, and reaches the junction with another cell. The place of such contact is called a synapse.
On the other side of the synapse, a short branching process, a dendrite, is adjacent to the point of contact. Signal transmission across a synapse is driven by active chemicals called transmitters.
Article on the topic: Tizin - instructions for spray and drops
Having arisen on the dendrite, the signal spreads along its membrane and passes further to the axon. To contract a skeletal muscle, the signal originates in the motor neuron of the cortex, passes along the pyramidal tract, passes to the interneuron and then to the region of the anterior horns of the spinal cord. This chain ends in muscle tissue.
The result of excitation of the motor center of the cortex will be a contraction of a group of muscle fibers.